Ann Surg Treat Res.
2018 Jun;94(6):298-305. 10.4174/astr.2018.94.6.298.
Nationwide survey of partial fundoplication in Korea: comparison with total fundoplication
- Affiliations
-
- 1Department of Surgery, Korea University College of Medicine, Seoul, Korea. ppongttai@gmail.com
- 2Department of Surgery, Chung-Ang University College of Medicine, Seoul, Korea.
- 3Department of Surgery, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 4Department of Surgery, Chosun University College of Medicine, Gwangju, Korea.
- 5Department of Surgery, Kosin University College of Medicine, Busan, Korea.
- 6Department of Surgery, Ajou University School of Medicine, Suwon, Korea.
- KMID: 2412399
- DOI: http://doi.org/10.4174/astr.2018.94.6.298
Abstract
- PURPOSE
Laparoscopic total fundoplication is the standard surgery for gastroesophageal reflux disease. However, partial fundoplication may be a viable alternative. Here, we conducted a nationwide survey of partial fundoplication in Korea.
METHODS
The Korean Anti-Reflux Surgery study group recorded 32 cases of partial fundoplication at eight hospitals between September 2009 and January 2016. The surgical outcomes and postoperative adverse symptoms in these cases were evaluated and compared with 86 cases of total fundoplication.
RESULTS
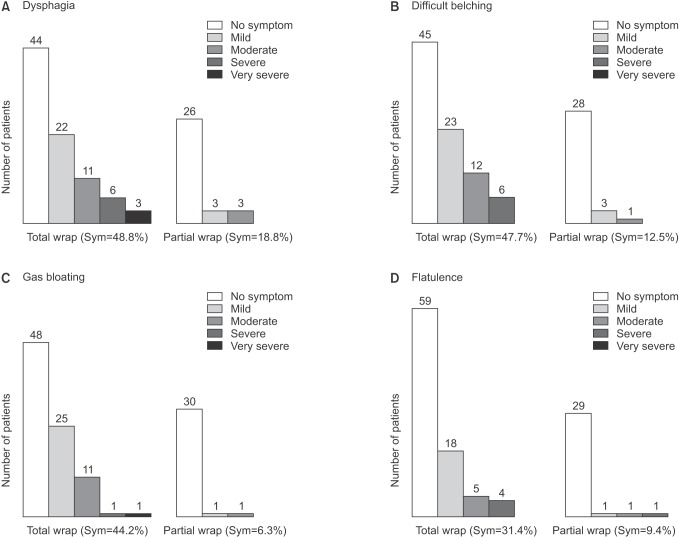
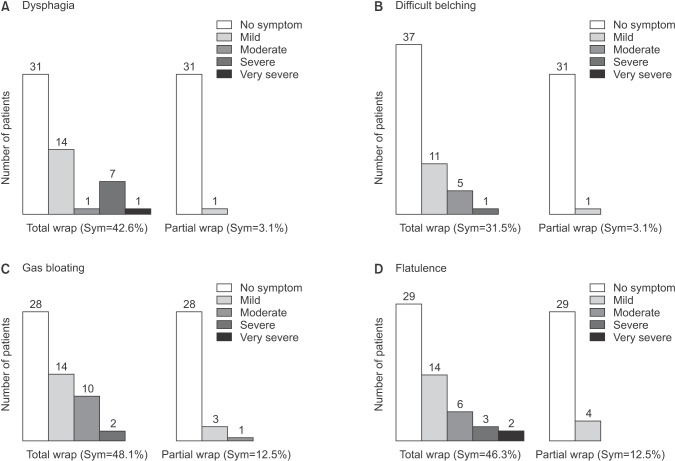
Anterior partial fundoplication was performed in 20 cases (62.5%) and posterior in 12 (37.5%). In most cases, partial fundoplication was a secondary procedure after operations for other conditions. Half of patients who underwent partial fundoplication had typical symptoms at the time of initial diagnosis, and most of them showed excellent (68.8%), good (25.0%), or fair (6.3%) symptom resolution at discharge. Compared to total fundoplication, partial fundoplication showed no difference in the resolution rate of typical and atypical symptoms. However, adverse symptoms such as dysphagia, difficult belching, gas bloating and flatulence were less common after partial fundoplication.
CONCLUSION
Although antireflux surgery is not popular in Korea and total fundoplication is the primary surgical choice for gastroesophageal reflux disease, partial fundoplication may be useful in certain conditions because it has less postoperative adverse symptoms but similar efficacy to total fundoplication.
MeSH Terms
Figure
Reference
-
1. Kim KM, Cho YK, Bae SJ, Kim DS, Shim KN, Kim JH, et al. Prevalence of gastroesophageal reflux disease in Korea and associated health-care utilization: a national population-based study. J Gastroenterol Hepatol. 2012; 27:741–745. PMID: 21916988.
Article2. Lee SK, Kim EK. Laparoscopic Nissen fundoplication in Korean patients with gastroesophageal reflux disease. Yonsei Med J. 2009; 50:89–94. PMID: 19259354.
Article3. Lee SB, Jeon KM, Kim BS, Kim KC, Jung HY, Choi YB. Early experiences of minimally invasive surgery to treat gastroesophageal reflux disease. J Korean Surg Soc. 2013; 84:330–337. PMID: 23741690.
Article4. Dallemagne B, Weerts JM, Jehaes C, Markiewicz S, Lombard R. Laparoscopic Nissen fundoplication: preliminary report. Surg Laparosc Endosc. 1991; 1:138–143. PMID: 1669393.5. Mahon D, Rhodes M, Decadt B, Hindmarsh A, Lowndes R, Beckingham I, et al. Randomized clinical trial of laparoscopic Nissen fundoplication compared with proton-pump inhibitors for treatment of chronic gastro-oesophageal reflux. Br J Surg. 2005; 92:695–699. PMID: 15898130.
Article6. Galmiche JP, Hatlebakk J, Attwood S, Ell C, Fiocca R, Eklund S, et al. Laparoscopic antireflux surgery vs esomeprazole treatment for chronic GERD: the LOTUS randomized clinical trial. JAMA. 2011; 305:1969–1977. PMID: 21586712.
Article7. Salminen P. The laparoscopic Nissen fundoplication: a better operation? Surgeon. 2009; 7:224–227. PMID: 19736889.8. Hunter JG, Swanstrom L, Waring JP. Dysphagia after laparoscopic antireflux surgery. The impact of operative technique. Ann Surg. 1996; 224:51–57. PMID: 8678618.9. Rantanen TK, Salo JA, Salminen JT, Kellokumpu IH. Functional outcome after laparoscopic or open Nissen fundoplication: a follow-up study. Arch Surg. 1999; 134:240–244. PMID: 10088561.10. Tupet A. Technique d'oesophago-gastroplastie avec phreno-gastropexie appliquee dans la cure radicale des hernies hiatales et comme complement de l'operation d Heller dans les cardiospasmes. Mem Acad Chir. 1963; 89:394–399.11. Broeders JA, Broeders EA, Watson DI, Devitt PG, Holloway RH, Jamieson GG. Objective outcomes 14 years after laparoscopic anterior 180-degree partial versus nissen fundoplication: results from a randomized trial. Ann Surg. 2013; 258:233–239. PMID: 23207247.12. Broeders JA, Roks DJ, Ahmed Ali U, Watson DI, Baigrie RJ, Cao Z, et al. Laparoscopic anterior 180-degree versus nissen fundoplication for gastroesophageal reflux disease: systematic review and meta-analysis of randomized clinical trials. Ann Surg. 2013; 257:850–859. PMID: 23470572.13. Singaporewalla RM, Baladas GH, Lee TD. Laparoendoscopic removal of a benign gastric stromal tumor at the cardia. JSLS. 2006; 10:117–121. PMID: 16709375.14. Park W, Vaezi MF. Etiology and pathogenesis of achalasia: the current understanding. Am J Gastroenterol. 2005; 100:1404–1414. PMID: 15929777.
Article15. Wang L, Li YM, Li L. Meta-analysis of randomized and controlled treatment trials for achalasia. Dig Dis Sci. 2009; 54:2303–2311. PMID: 19107596.
Article16. Boeckxstaens GE, Annese V, des Varannes SB, Chaussade S, Costantini M, Cuttitta A, et al. Pneumatic dilation versus laparoscopic Heller's myotomy for idiopathic achalasia. N Engl J Med. 2011; 364:1807–1816. PMID: 21561346.
Article17. Rebecchi F, Giaccone C, Farinella E, Campaci R, Morino M. Randomized controlled trial of laparoscopic Heller myotomy plus Dor fundoplication versus Nissen fundoplication for achalasia: long-term results. Ann Surg. 2008; 248:1023–1030. PMID: 19092347.18. Mitiek MO, Andrade RS. Giant hiatal hernia. Ann Thorac Surg. 2010; 89:S2168–S2173. PMID: 20494004.
Article19. Morino M, Giaccone C, Pellegrino L, Rebecchi F. Laparoscopic management of giant hiatal hernia: factors influencing long-term outcome. Surg Endosc. 2006; 20:1011–1016. PMID: 16763927.
Article20. Stylopoulos N, Gazelle GS, Rattner DW. Paraesophageal hernias: operation or observation? Ann Surg. 2002; 236:492–500. PMID: 12368678.
Article21. Lal DR, Pellegrini CA, Oelschlager BK. Laparoscopic repair of paraesophageal hernia. Surg Clin North Am. 2005; 85:105–118. xPMID: 15619532.
Article22. Swanstrom LL, Jobe BA, Kinzie LR, Horvath KD. Esophageal motility and outcomes following laparoscopic paraesophageal hernia repair and fundoplication. Am J Surg. 1999; 177:359–363. PMID: 10365869.
Article23. Fuller CB, Hagen JA, DeMeester TR, Peters JH, Ritter M, Bremmer CG. The role of fundoplication in the treatment of type II paraesophageal hernia. J Thorac Cardiovasc Surg. 1996; 111:655–661. PMID: 8601982.
Article24. Seo KW, Park MI, Yoon KY, Park SJ, Kim SE. Laparoscopic partial fundoplication in case of gastroesophageal reflux disease patient with absent esophageal motility. J Gastric Cancer. 2015; 15:127–131. PMID: 26161286.
Article25. Lee JH, Park JM, Han SU, Kim JJ, Song KY, Ryu SW, et al. Antireflux surgery in Korea: a nationwide study from 2011 to 2014. Gut Liver. 2016; 10:726–730. PMID: 27114420.
Article26. Laws HL, Clements RH, Swillie CM. A randomized, prospective comparison of the Nissen fundoplication versus the Toupet fundoplication for gastroesophageal reflux disease. Ann Surg. 1997; 225:647–653. PMID: 9230805.
Article27. Chrysos E, Tsiaoussis J, Zoras OJ, Athanasakis E, Mantides A, Katsamouris A, et al. Laparoscopic surgery for gastroesophageal reflux disease patients with impaired esophageal peristalsis: total or partial fundoplication? J Am Coll Surg. 2003; 197:8–15. PMID: 12831918.
Article28. Guerin E, Betroune K, Closset J, Mehdi A, Lefebvre JC, Houben JJ, et al. Nissen versus Toupet fundoplication: results of a randomized and multicenter trial. Surg Endosc. 2007; 21:1985–1990. PMID: 17704884.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison between Laparoscopic and Open Nissen Fundoplication in Pediatric Patients
- The Eleven Years' Experience with Fundoplication in Infants and Children
- Nissen Fundoplication for the Treatment of Gastroesophageal Reflux After Repair of Esophageal Atresia
- A Case of Belsey Mark IV Fundoplication after Failed Nissen Antireflux Surgery
- Effective Management of Gastroparesis with Erythromycin after Laparoscopic Nissen Fundoplication: A case report