Clin Orthop Surg.
2016 Dec;8(4):452-457. 10.4055/cios.2016.8.4.452.
Treatment of Late-Onset Legg-Calve-Perthes Disease by Arthrodiastasis
- Affiliations
-
- 1Department of Orthopaedic Surgery, Dong-A University College of Medicine, Busan, Korea. libi33@dau.ac.kr
- KMID: 2412329
- DOI: http://doi.org/10.4055/cios.2016.8.4.452
Abstract
- BACKGROUND
To evaluate the efficacy of arthrodiastasis for Legg-Calve-Perthes disease.
METHODS
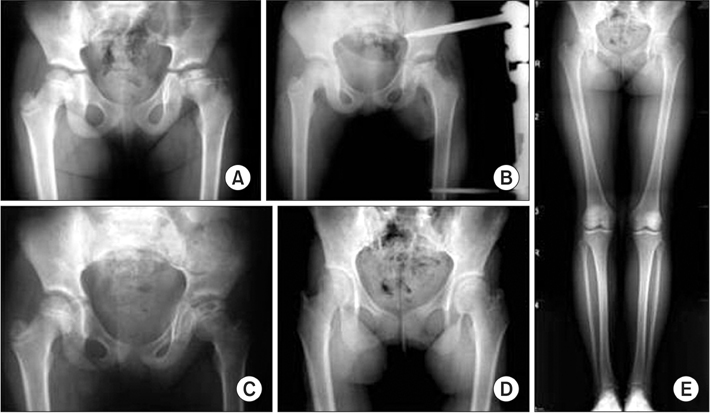
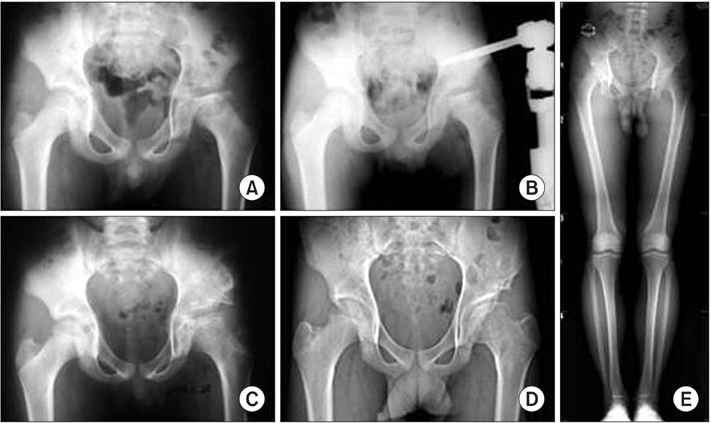
Arthrodiastasis was conducted using external fixator devices (Orthofix) in 7 patients at least 8 years of age with a diagnosis of Legg-Calve-Perthes disease. The average follow-up was 80 months (range, 32 to 149 months), and their average age was 9.1 years (range, 8 to 12 years). The results of treatment were evaluated by measuring the degree of hip pain and the range of motion of the hip at 6 months after the operation and comparing the values with preoperative measurements. Radiological recovery was evaluated by the epiphyseal index and compared with the preoperative values. At the final follow-up, clinical and radiological results were evaluated using the Iowa hip score and the Stulberg classification.
RESULTS
On the clinical evaluation performed at 6 months after arthrodiastasis, the degree of pain decreased by 1.8 points on average, and the average flexion, internal rotation, and abduction increased by 35°, 16°, and 11°, respectively. Based on radiological findings, the epiphyseal index showed a remarkable increase of 6.6 on average (from 19 preoperatively to 26 postoperatively). At the final follow-up, the average Iowa hip score improved from 65 points preoperatively to 84 points. There were 1 Stulberg class I hip, 2 Stulberg class II hips, 3 Stulberg class III hips, 1 Stulberg class IV hip, and no Stulberg class V hip.
CONCLUSIONS
We conclude that arthrodiastasis using an external fixator can be a relatively promising surgical procedure for the treatment of late-onset Legg-Calve-Perthes disease.
Keyword
MeSH Terms
Figure
Reference
-
1. Stulberg SD, Cooperman DR, Wallensten R. The natural history of Legg-Calve-Perthes disease. J Bone Joint Surg Am. 1981; 63(7):1095–1108.2. Bellyei A, Mike G. Acetabular development in Legg-Calve-Perthes disease. Orthopedics. 1988; 11(3):407–411.3. Mazda K, Pennecot GF, Zeller R, Taussig G. Perthes' disease after the age of twelve years: role of the remaining growth. J Bone Joint Surg Br. 1999; 81(4):696–698.4. Herring JA, Kim HT, Browne R. Legg-Calve-Perthes disease. Part I: classification of radiographs with use of the modified lateral pillar and Stulberg classifications. J Bone Joint Surg Am. 2004; 86(10):2103–2120.5. Heyman CH, Herndon CH. Legg-Perthes disease: a method for the measurement of the roentgenographic result. J Bone Joint Surg Am. 1950; 32(4):767–778.6. Aldegheri R, Trivella G, Saleh M. Articulated distraction of the hip. In : De Bastiani G, Apley AG, Goldberg A, editors. Orthofix external fixation in trauma and orthopaedics. London: Springer Verlag;2000. p. 605–612.7. Aldegheri R, Trivella G, Saleh M. Articulated distraction of the hip: conservative surgery for arthritis in young patients. Clin Orthop Relat Res. 1994; (301):94–101.
Article8. Kocaoglu M, Kilicoglu OI, Goksan SB, Cakmak M. Ilizarov fixator for treatment of Legg-Calve-Perthes disease. J Pediatr Orthop B. 1999; 8(4):276–281.9. Guamiero R, Luzo CA, Montenegro NB, Godoy RM. Legg-Calve-Perthes disease: a comparative study between two types of treatment: femoral varus osteotomy and arthrochondrodiastasis with external fixation. In : 25th European Paediatric Ophthalmological Society (EPOS); 2000; Milan, Italy.10. Kucukkaya M, Kabukcuoglu Y, Ozturk I, Kuzgun U. Avascular necrosis of the femoral head in childhood: the results of treatment with articulated distraction method. J Pediatr Orthop. 2000; 20(6):722–728.
Article11. Daly K, Bruce C, Catterall A. Lateral shelf acetabuloplasty in Perthes' disease: a review of the end of growth. J Bone Joint Surg Br. 1999; 81(3):380–384.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Observation of the Legg-Calve-Perthes Disease: Preliminary Report
- Legg - Calve Perthes disease in Monozygotic Male Twins
- Osteochondritis Dissecans of Femoral Head Following Legg-Calve-Perthes Disease
- Innominate Osteotomy in Legg-Calve-Perthes Disease
- Late Complications of Legg-Calve-Perthes Disease