Clin Orthop Surg.
2016 Dec;8(4):358-366. 10.4055/cios.2016.8.4.358.
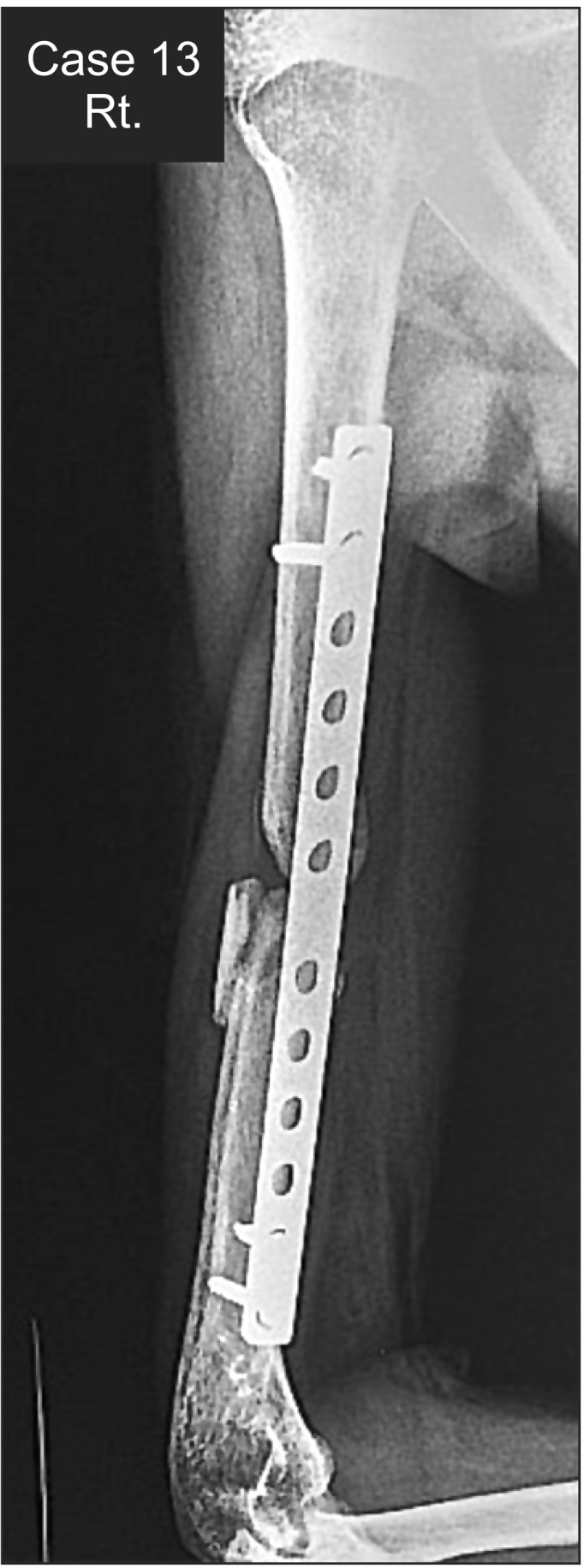
Is Anterior Bridge Plating for Mid-Shaft Humeral Fractures a Suitable Option for Patients Predominantly Involved in Overhead Activities? A Functional Outcome Study in Athletes and Manual Laborers
- Affiliations
-
- 1Department of Orthopedics & Joint Center, CHA Bundang Medical Center, Seongnam, Korea. drjkim@cha.ac.kr
- 2Department of Orthopaedics, Dr. V. M. Government Medical College & S. C. S. M. General Hospital, Solapur, India.
- KMID: 2412316
- DOI: http://doi.org/10.4055/cios.2016.8.4.358
Abstract
- BACKGROUND
To assess the functional and radiological outcomes of minimally invasive anterior bridge plating (ABP) for mid-shaft humerus fractures in patients predominantly involved in overhead activities (athletes and manual laborers).
METHODS
Forty-eight patients fulfilling inclusion criteria were treated with ABP at a level-I trauma center using a 4.5-mm dynamic/locking compression plate and followed for a period of 1 year. Functional outcome was assessed using the Constant, Mayo elbow, and Disabilities of the Arm, Shoulder and Hand (DASH) scores. Range of motion (ROM), subjective strength, and radiographic union were assessed. A general satisfaction questionnaire was also administered.
RESULTS
Most patients achieved excellent functional and radiological outcomes. ROM and strength of the shoulder girdle exhibited clinically nonsignificant loss as compared to the opposite side. The mean time for return to the original activities was 64 days (range, 36 to 182 days) and the mean time for confirmed radiographic union was 45 days (range, 34 to 180 days). The mean Constant, Mayo elbow, DASH scores were 95.73 ± 5.76 (range, 79 to 100), 95.94 ± 6.74 (range, 85 to 100), and 1.56 ± 3.15 (range, 0.0 to 14.0), respectively. The majority of patients (43 patients, 89.6%) who fell in the excellent or very good category according to our questionnaire were extremely satisfied. There were 2 cases (4.17%) of nonunion and 3 patients (6.25%) had to change/modify their original occupation.
CONCLUSIONS
ABP is fundamentally different from traditional open posterior plating or conventional intramedullary nailing. It gives relative stability with union taking place by callus formation, and a longer plate on the tensile surface ensures that the humerus can withstand greater amount of rotational and bending stresses. The minimally invasive nature causes minimal soft tissue damage and, if done correctly, causes no damage to the vital structures in proximity. ABP for mid-shaft humerus fractures in patients predominantly engaged in overhead activities is a safe and effective treatment modality yielding high rates of union, excellent functional recovery, minimal biological disruption, better cosmesis, and superior satisfaction rates.
MeSH Terms
-
Adult
Athletes
*Bone Plates
Female
Fracture Fixation, Internal/instrumentation/*methods/statistics & numerical data
Humans
Humeral Fractures/*surgery
Male
Middle Aged
Minimally Invasive Surgical Procedures/instrumentation/*methods/statistics & numerical data
Patient Satisfaction
Prospective Studies
Range of Motion, Articular/*physiology
Young Adult
Figure
Reference
-
1. Walker M, Palumbo B, Badman B, Brooks J, Van Gelderen J, Mighell M. Humeral shaft fractures: a review. J Shoulder Elbow Surg. 2011; 20(5):833–844. PMID: 21393016.
Article2. Sarmiento A, Zagorski JB, Zych GA, Latta LL, Capps CA. Functional bracing for the treatment of fractures of the humeral diaphysis. J Bone Joint Surg Am. 2000; 82(4):478–486. PMID: 10761938.
Article3. Kurup H, Hossain M, Andrew JG. Dynamic compression plating versus locked intramedullary nailing for humeral shaft fractures in adults. Cochrane Database Syst Rev. 2011; (6):CD005959. PMID: 21678350.
Article4. An Z, Zeng B, He X, Chen Q, Hu S. Plating osteosynthesis of mid-distal humeral shaft fractures: minimally invasive versus conventional open reduction technique. Int Orthop. 2010; 34(1):131–135. PMID: 19301000.
Article5. Chao TC, Chou WY, Chung JC, Hsu CJ. Humeral shaft fractures treated by dynamic compression plates, Ender nails and interlocking nails. Int Orthop. 2005; 29(2):88–91. PMID: 15714304.
Article6. Vilaca PR Jr, Uezumi MK. Anterior minimally invasive bridge-plate technique for treatment of humeral shaft nonunion. J Orthop Traumatol. 2012; 13(4):211–216. PMID: 22717617.7. Concha JM, Sandoval A, Streubel PN. Minimally invasive plate osteosynthesis for humeral shaft fractures: are results reproducible? Int Orthop. 2010; 34(8):1297–1305. PMID: 19844708.
Article8. Shetty MS, Kumar MA, Sujay K, Kini AR, Kanthi KG. Minimally invasive plate osteosynthesis for humerus diaphyseal fractures. Indian J Orthop. 2011; 45(6):520–526. PMID: 22144745.
Article9. Jiang R, Luo CF, Zeng BF, Mei GH. Minimally invasive plating for complex humeral shaft fractures. Arch Orthop Trauma Surg. 2007; 127(7):531–535. PMID: 17401571.
Article10. Kim JW, Oh CW, Byun YS, Kim JJ, Park KC. A prospective randomized study of operative treatment for noncomminuted humeral shaft fractures: conventional open plating versus minimal invasive plate osteosynthesis. J Orthop Trauma. 2015; 29(4):189–194. PMID: 25210833.11. Bhandari M, Devereaux PJ, McKee MD, Schemitsch EH. Compression plating versus intramedullary nailing of humeral shaft fractures: a meta-analysis. Acta Orthop. 2006; 77(2):279–284. PMID: 16752291.12. Ziran BH, Belangero W, Livani B, Pesantez R. Percutaneous plating of the humerus with locked plating: technique and case report. J Trauma. 2007; 63(1):205–210. PMID: 17622893.
Article13. Zhiquan A, Bingfang Z, Yeming W, Chi Z, Peiyan H. Minimally invasive plating osteosynthesis (MIPO) of middle and distal third humeral shaft fractures. J Orthop Trauma. 2007; 21(9):628–633. PMID: 17921838.
Article14. Matsunaga FT, Tamaoki MJ, Matsumoto MH, dos Santos JB, Faloppa F, Belloti JC. Treatment of the humeral shaft fractures: minimally invasive osteosynthesis with bridge plate versus conservative treatment with functional brace: study protocol for a randomised controlled trial. Trials. 2013; 14:246. PMID: 23924198.
Article15. Wang C, Li J, Li Y, Dai G, Wang M. Is minimally invasive plating osteosynthesis for humeral shaft fracture advantageous compared with the conventional open technique? J Shoulder Elbow Surg. 2015; 24(11):1741–1748. PMID: 26480879.
Article16. Krettek C, Miclau T, Grun O, Schandelmaier P, Tscherne H. Intraoperative control of axes, rotation and length in femoral and tibial fractures: technical note. Injury. 1998; 29(Suppl 3):C29–C39. PMID: 10341895.
Article17. Apivatthakakul T, Patiyasikan S, Luevitoonvechkit S. Danger zone for locking screw placement in minimally invasive plate osteosynthesis (MIPO) of humeral shaft fractures: a cadaveric study. Injury. 2010; 41(2):169–172. PMID: 19735916.
Article18. Livani B, Belangero W, Andrade K, Zuiani G, Pratali R. Is MIPO in humeral shaft fractures really safe? Postoperative ultrasonographic evaluation. Int Orthop. 2009; 33(6):1719–1723. PMID: 18704415.
Article19. Shin SJ, Sohn HS, Do NH. Minimally invasive plate osteosynthesis of humeral shaft fractures: a technique to aid fracture reduction and minimize complications. J Orthop Trauma. 2012; 26(10):585–589. PMID: 22534690.20. Apivatthakakul T, Arpornchayanon O, Bavornratanavech S. Minimally invasive plate osteosynthesis (MIPO) of the humeral shaft fracture. Is it possible? A cadaveric study and preliminary report. Injury. 2005; 36(4):530–538. PMID: 15755436.21. Malhan S, Thomas S, Srivastav S, et al. Minimally invasive plate osteosynthesis using a locking compression plate for diaphyseal humeral fractures. J Orthop Surg (Hong Kong). 2012; 20(3):292–296. PMID: 23255632.
Article22. Wang ZH, Xiang M, Xie J, Tang HC, Chen H, Liu X. Treatment of humerus shaft fractures using minimally invasive percutaneous plate osteosynthesis through anterior approach. Zhongguo Gu Shang. 2009; 22(9):681–683. PMID: 19817201.23. Singisetti K, Ambedkar M. Nailing versus plating in humerus shaft fractures: a prospective comparative study. Int Orthop. 2010; 34(4):571–576. PMID: 19506868.
Article24. Uhthoff HK, Poitras P, Backman DS. Internal plate fixation of fractures: short history and recent developments. J Orthop Sci. 2006; 11(2):118–126. PMID: 16568382.
Article25. Seroyer ST, Nho SJ, Bach BR, Bush-Joseph CA, Nicholson GP, Romeo AA. The kinetic chain in overhand pitching: its potential role for performance enhancement and injury prevention. Sports Health. 2010; 2(2):135–146. PMID: 23015931.
Article26. O'Toole RV, Andersen RC, Vesnovsky O, et al. Are locking screws advantageous with plate fixation of humeral shaft fractures? A biomechanical analysis of synthetic and cadaveric bone. J Orthop Trauma. 2008; 22(10):709–715. PMID: 18978547.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A prospective cohort study: promising results with minimally invasive plate osteosynthesis of anterior bridge plating in adult humeral shaft fractures
- Minimally Invasive Anterior Plating of Humeral Shaft Fractures
- Internal Fixation of Humeral Shaft Fractures Using Anterior Plating Technique
- Helical Plating for Fractures of the Proximal Humeral Shaft
- Comparative Analysis of the Result of Minimally Invasive Anterior Plating and Open Reduction and Internal Fixation in Humerus Shaft Simple Fracture