Clin Orthop Surg.
2017 Mar;9(1):71-76. 10.4055/cios.2017.9.1.71.
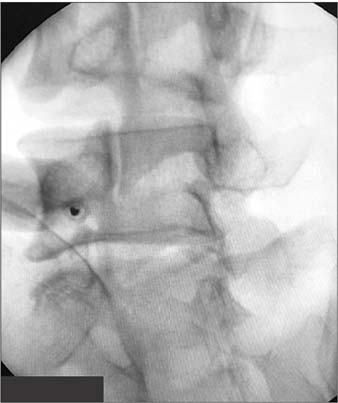
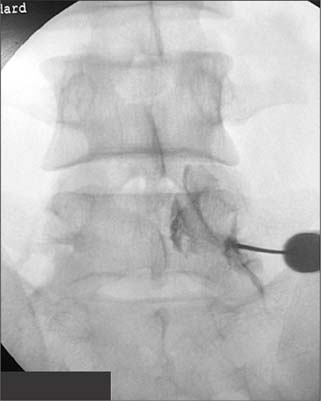
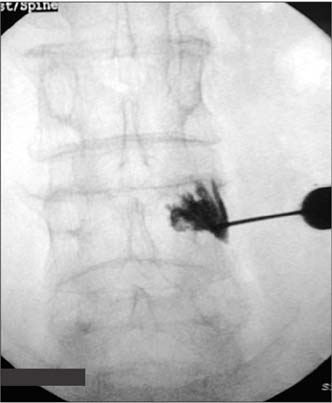
Assessment of Anteroposterior Subpedicular Approach and Oblique Scotty Dog Subpedicular Approach for Selective Nerve Root Block
- Affiliations
-
- 1Department of Orthopaedic Surgery, Melmaruvathur Adhiparasakthi Institute of Medical Sciences and Research, Melmaruvathur, Tamil Nadu, India. dr.arunkumar.orth@gmail.com
- 2Department of Orthopaedic Surgery, Chang Gung Memorial Hospital, Chang Gung University College of Medicine, Taoyuan, Taiwan.
- 3Universiti Tunku Abdul Rahman, Sungai Long, Malaysia.
- KMID: 2412306
- DOI: http://doi.org/10.4055/cios.2017.9.1.71
Abstract
- BACKGROUND
The technique used to administer a selective nerve root block (SNRB) varies depending on individual expertise. Both the anteroposterior (AP) subpedicular approach and oblique Scotty dog subpedicular approach are widely practiced. However, the literature does not provide a clear consensus regarding which approach is more suitable. Hence, we decided to analyse the procedural parameters and clinical outcomes following SNRBs using these two approaches.
METHODS
Patients diagnosed with a single lumbar herniated intervertebral disc (HIVD) refractory to conservative management but not willing for immediate surgery were selected for a prospective nonrandomized comparative study. An SNRB was administered as a therapeutic alternative using the AP subpedicular approach in one group (n = 25; mean age, 45 ± 5.4 years) and the oblique Scotty dog subpedicular approach in the other group (n = 22; mean age, 43.8 ± 4.7 years). Results were compared in terms of the duration of the procedure, the number of C-arm exposures, accuracy, pain relief, functional outcome and the duration of relief.
RESULTS
Our results suggest that the oblique Scotty dog subpedicular approach took a significantly longer duration (p = 0.02) and a greater number of C-arm exposures (p = 0.001). But, its accuracy of needle placement was 95.5% compared to only 72% using the AP subpedicular approach (p = 0.03). There was no significant difference in terms of clinical outcomes between these approaches.
CONCLUSIONS
The AP subpedicular approach was simple and facile, but the oblique Scotty dog subpedicular approach was more accurate. However, a brief window period of pain relief was achieved irrespective of the approaching technique used.
MeSH Terms
Figure
Cited by 1 articles
-
Revalidating Pfirrmann's Magnetic Resonance Image-Based Grading of Lumbar Nerve Root Compromise by Calculating Reliability among Orthopaedic Residents
Arun-Kumar Kaliya-Perumal, Senthil-Kumar Ariputhiran-Tamilselvam, Chi-An Luo, Sivaharivelan Thiagarajan, Udhayakumar Selvam, Raj-Prabhakar Sumathi-Edirolimanian
Clin Orthop Surg. 2018;10(2):210-215. doi: 10.4055/cios.2018.10.2.210.
Reference
-
1. Stafford MA, Peng P, Hill DA. Sciatica: a review of history, epidemiology, pathogenesis, and the role of epidural steroid injection in management. Br J Anaesth. 2007; 99(4):461–473.
Article2. Patel N. Surgical disorders of the thoracic and lumbar spine: a guide for neurologists. J Neurol Neurosurg Psychiatry. 2002; 73:Suppl 1. i42–i48.3. Shelerud RA, Paynter KS. Rarer causes of radiculopathy: spinal tumors, infections, and other unusual causes. Phys Med Rehabil Clin N Am. 2002; 13(3):645–696.
Article4. Yeom JS, Lee JW, Park KW, et al. Value of diagnostic lumbar selective nerve root block: a prospective controlled study. AJNR Am J Neuroradiol. 2008; 29(5):1017–1023.
Article5. Narozny M, Zanetti M, Boos N. Therapeutic efficacy of selective nerve root blocks in the treatment of lumbar radicular leg pain. Swiss Med Wkly. 2001; 131(5-6):75–80.6. Eastley NC, Spiteri V, Newey ML. Variations in selective nerve root block technique. Ann R Coll Surg Engl. 2013; 95(7):515–518.
Article7. Pfirrmann CW, Oberholzer PA, Zanetti M, et al. Selective nerve root blocks for the treatment of sciatica: evaluation of injection site and effectiveness: a study with patients and cadavers. Radiology. 2001; 221(3):704–711.
Article8. Eckel TS, Bartynski WS. Epidural steroid injections and selective nerve root blocks. Tech Vasc Interv Radiol. 2009; 12(1):11–21.
Article9. Hui CW, Chan PH, Cheung KK. Selective nerve root block for sciatica. Hong Kong J Orthop Surg. 2005; 9(1):22–27.10. Arun-Kumar K, Jayaprasad S, Senthil K, Lohith H, Jayaprakash KV. The outcomes of selective nerve root block for disc induced lumbar radiculopathy. Malays Orthop J. 2015; 9(3):17–22.
Article11. Pfirrmann CW, Dora C, Schmid MR, Zanetti M, Hodler J, Boos N. MR image-based grading of lumbar nerve root compromise due to disk herniation: reliability study with surgical correlation. Radiology. 2004; 230(2):583–588.
Article12. Chiba S, Tsutsui S, Chiba T, et al. Relationship among analgesic effects, radiating pain, and radiological contrast material distribution in lumbosacral selective nerve root block. J Pain Relief. 2014; 3(5):157.
Article13. Fish DE, Lee PC, Marcus DB. The S1 “Scotty dog”: report of a technique for S1 transforaminal epidural steroid injection. Arch Phys Med Rehabil. 2007; 88(12):1730–1733.
Article14. Fardon DF, Williams AL, Dohring EJ, Murtagh FR, Gabriel Rothman SL, Sze GK. Lumbar disc nomenclature: version 2.0: recommendations of the combined task forces of the North American Spine Society, the American Society of Spine Radiology and the American Society of Neuroradiology. Spine J. 2014; 14(11):2525–2545.15. Boden SD, Davis DO, Dina TS, Patronas NJ, Wiesel SW. Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects: a prospective investigation. J Bone Joint Surg Am. 1990; 72(3):403–408.
Article16. Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res (Hoboken). 2011; 63:Suppl 11. S240–S252.17. Roland M, Morris R. A study of the natural history of back pain. part I: development of a reliable and sensitive measure of disability in low-back pain. Spine (Phila Pa 1976). 1983; 8(2):141–144.18. Stevens ML, Lin CC, Maher CG. The Roland Morris Disability Questionnaire. J Physiother. 2016; 62(2):116.
Article19. Vassiliev D. Spread of contrast during L4 and L5 nerve root infiltration under fluoroscopic guidance. Pain Physician. 2007; 10(3):461–466.20. Tauheed N, Usmani H, Siddiqui AH. A comparison of the analgesic efficacy of transforaminal methylprednisolone alone and with low doses of clonidine in lumbo-sacral radiculopathy. Saudi J Anaesth. 2014; 8(1):51–58.
Article21. Owlia MB, Salimzadeh A, Alishiri G, Haghighi A. Comparison of two doses of corticosteroid in epidural steroid injection for lumbar radicular pain. Singapore Med J. 2007; 48(3):241–245.22. Benedetti EM, Siriwetchadarak R. Selective nerve root blocks as predictors of surgical outcome: fact or fiction? Tech Reg Anesth Pain Manag. 2011; 15(1):4–11.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Kambin's Triangle Approach of Lumbar Transforaminal Epidural Injection with Spinal Stenosis
- Retrodiscal Approach of Lumbar Epidural Block
- The Value of Selective Nerve Root Block to Predict Surgical Outcome for Spinal Surgery
- Selective Dual Nerve Root Block Through Extreme Lateral Transforaminal Approach
- Selective Spinal Nerve Root Block for the Treatment of Sciatica