Clin Orthop Surg.
2017 Jun;9(2):169-176. 10.4055/cios.2017.9.2.169.
Robotic Total Knee Arthroplasty with a Cruciate-Retaining Implant: A 10-Year Follow-up Study
- Affiliations
-
- 1Department of Orthopedic Surgery, Center for Joint Disease, Chonnam National University Bitgoeul Hospital, Gwangju, Korea. eksong@chonnam.ac.kr
- 2Chonnam National University Research Institute of Medical Science, Gwangju, Korea.
- KMID: 2412284
- DOI: http://doi.org/10.4055/cios.2017.9.2.169
Abstract
- BACKGROUND
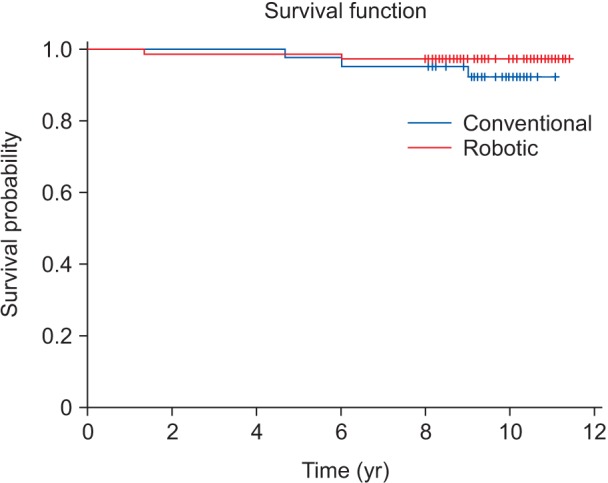
This study compared clinical and radiological results between robotic total knee arthroplasty (TKA) and conventional TKA with a cruciate-retaining implant at 10-year follow-up. The hypothesis was that robotic TKA would allow for more accurate leg alignment and component placement, and thus enhance clinical and radiological results and long-term survival rates.
METHODS
A total of 113 primary TKAs performed using a cruciate-retaining implant in 102 patients from 2004 to 2007 were reviewed retrospectively. Of the 113 TKAs, 71 were robotic TKAs and 42 were conventional TKAs. Clinical outcomes (visual analogue scale pain score, Hospital for Special Surgery score, Western Ontario and McMaster University score, range of motion, and complications), radiological outcomes, and long-term survival rates were evaluated at a mean follow-up of 10 years.
RESULTS
Clinical outcomes and long-term survival rates were similar between the two groups. Regarding the radiological outcomes, the robotic TKA group had significantly fewer postoperative leg alignment outliers (femoral coronal inclination, tibial coronal inclination, femoral sagittal inclination, tibial sagittal inclination, and mechanical axis) and fewer radiolucent lines than the conventional TKA group.
CONCLUSIONS
Both robotic and conventional TKAs resulted in good clinical outcomes and postoperative leg alignments. Robotic TKA appeared to reduce the incidence of leg alignment outliers and radiolucent lines compared to conventional TKA.
Keyword
MeSH Terms
Figure
Reference
-
1. Laskin RS. The Genesis total knee prosthesis: a 10-year followup study. Clin Orthop Relat Res. 2001; (388):95–102.2. Rodriguez JA, Bhende H, Ranawat CS. Total condylar knee replacement: a 20-year followup study. Clin Orthop Relat Res. 2001; (388):10–17.3. Scott WN, Rubinstein M, Scuderi G. Results after knee replacement with a posterior cruciate-substituting prosthesis. J Bone Joint Surg Am. 1988; 70(8):1163–1173. PMID: 3417701.
Article4. Griffin FM, Insall JN, Scuderi GR. Accuracy of soft tissue balancing in total knee arthroplasty. J Arthroplasty. 2000; 15(8):970–973. PMID: 11112189.
Article5. Laskin RS, Rieger MA. The surgical technique for performing a total knee replacement arthroplasty. Orthop Clin North Am. 1989; 20(1):31–48. PMID: 2919077.6. Ritter MA, Faris PM, Keating EM, Meding JB. Postoperative alignment of total knee replacement: its effect on survival. Clin Orthop Relat Res. 1994; (299):153–156. PMID: 8119010.
Article7. Takahashi T, Wada Y, Yamamoto H. Soft-tissue balancing with pressure distribution during total knee arthroplasty. J Bone Joint Surg Br. 1997; 79(2):235–239. PMID: 9119849.
Article8. Jacofsky DJ, Allen M. Robotics in arthroplasty: a comprehensive review. J Arthroplasty. 2016; 31(10):2353–2363. PMID: 27325369.
Article9. Song EK, Seon JK, Park SJ, Jung WB, Park HW, Lee GW. Simultaneous bilateral total knee arthroplasty with robotic and conventional techniques: a prospective, randomized study. Knee Surg Sports Traumatol Arthrosc. 2011; 19(7):1069–1076. PMID: 21311869.
Article10. Song EK, Seon JK, Yim JH, Netravali NA, Bargar WL. Robotic-assisted TKA reduces postoperative alignment outliers and improves gap balance compared to conventional TKA. Clin Orthop Relat Res. 2013; 471(1):118–126. PMID: 22669549.
Article11. Matsen FA 3rd, Garbini JL, Sidles JA, Pratt B, Baumgarten D, Kaiura R. Robotic assistance in orthopaedic surgery: a proof of principle using distal femoral arthroplasty. Clin Orthop Relat Res. 1993; (296):178–186.12. Decking J, Theis C, Achenbach T, Roth E, Nafe B, Eckardt A. Robotic total knee arthroplasty: the accuracy of CT-based component placement. Acta Orthop Scand. 2004; 75(5):573–579. PMID: 15513489.13. Park SE, Lee CT. Comparison of robotic-assisted and conventional manual implantation of a primary total knee arthroplasty. J Arthroplasty. 2007; 22(7):1054–1059. PMID: 17920481.
Article14. Song EK, Jung WB, Yoon TR, Park KS, Seo HY, Seon JK. Comparison of outcomes after bilateral simultaneous total knee arthroplasty using gender-specific and unisex knees. J Arthroplasty. 2012; 27(2):226–231. PMID: 21704482.
Article15. Asano H, Hoshino A, Wilton TJ. Soft-tissue tension total knee arthroplasty. J Arthroplasty. 2004; 19(5):558–561. PMID: 15284975.
Article16. Adam C, Eckstein F, Milz S, Putz R. The distribution of cartilage thickness within the joints of the lower limb of elderly individuals. J Anat. 1998; 193(Pt 2):203–214. PMID: 9827636.17. Ateshian GA, Soslowsky LJ, Mow VC. Quantitation of articular surface topography and cartilage thickness in knee joints using stereophotogrammetry. J Biomech. 1991; 24(8):761–776. PMID: 1918099.
Article18. Shepherd DE, Seedhom BB. Thickness of human articular cartilage in joints of the lower limb. Ann Rheum Dis. 1999; 58(1):27–34. PMID: 10343537.
Article19. Sasanuma H, Sekiya H, Takatoku K, Takada H, Sugimoto N. Evaluation of soft-tissue balance during total knee arthroplasty. J Orthop Surg (Hong Kong). 2010; 18(1):26–30. PMID: 20427829.
Article20. Sekiya H, Takatoku K, Takada H, Sasanuma H, Sugimoto N. Postoperative lateral ligamentous laxity diminishes with time after TKA in the varus knee. Clin Orthop Relat Res. 2009; 467(6):1582–1586. PMID: 18941848.
Article21. Winemaker MJ. Perfect balance in total knee arthroplasty: the elusive compromise. J Arthroplasty. 2002; 17(1):2–10.
Article22. Sugama R, Kadoya Y, Kobayashi A, Takaoka K. Preparation of the flexion gap affects the extension gap in total knee arthroplasty. J Arthroplasty. 2005; 20(5):602–607. PMID: 16309995.
Article23. Ewald FC. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res. 1989; (248):9–12.
Article24. Jeffery RS, Morris RW, Denham RA. Coronal alignment after total knee replacement. J Bone Joint Surg Br. 1991; 73(5):709–714. PMID: 1894655.
Article25. Saragaglia D, Picard F, Chaussard C, Montbarbon E, Leitner F, Cinquin P. Computer-assisted knee arthroplasty: comparison with a conventional procedure: results of 50 cases in a prospective randomized study. Rev Chir Orthop Reparatrice Appar Mot. 2001; 87(1):18–28. PMID: 11240534.26. Fadda M, Marcacci M, Toksvig-Larsen S, Wang T, Meneghello R. Improving accuracy of bone resections using robotics tool holder and a high speed milling cutting tool. J Med Eng Technol. 1998; 22(6):280–284. PMID: 9884932.
Article27. Peersman G, Laskin R, Davis J, Peterson MG, Richart T. Prolonged operative time correlates with increased infection rate after total knee arthroplasty. HSS J. 2006; 2(1):70–72. PMID: 18751850.
Article28. Bathis H, Perlick L, Tingart M, Perlick C, Luring C, Grifka J. Intraoperative cutting errors in total knee arthroplasty. Arch Orthop Trauma Surg. 2005; 125(1):16–20. PMID: 15538589.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Posterior Cruciate Ligament Retaining Total Knee Arthroplasty
- Results of Posterior Cruciate Retaining and Cruciate Substituting Total Knee Arthroplasty (3 to 8 years follow up)
- Short Term Results of Cruciate Retaining TypeMobile Bearing Total Knee Arthroplasty: Using a Navigation System
- Cruciate Retaining Medial Pivot Knee
- Comparison of Posterior Cruciate Retaining & Substituting Total Knee Arthroplasty in Varus Deformity of Knee