Clin Orthop Surg.
2017 Dec;9(4):506-513. 10.4055/cios.2017.9.4.506.
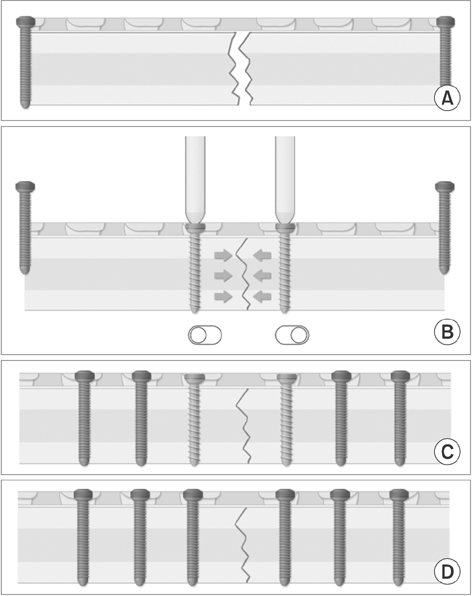
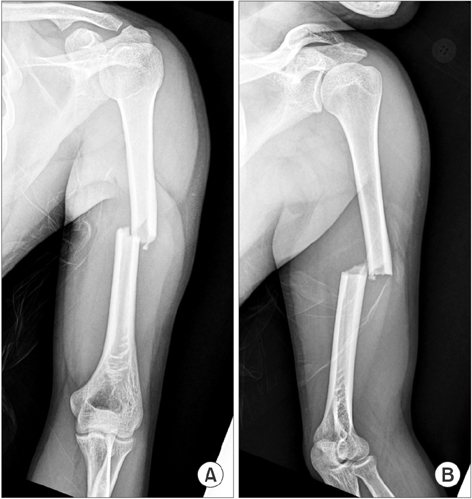
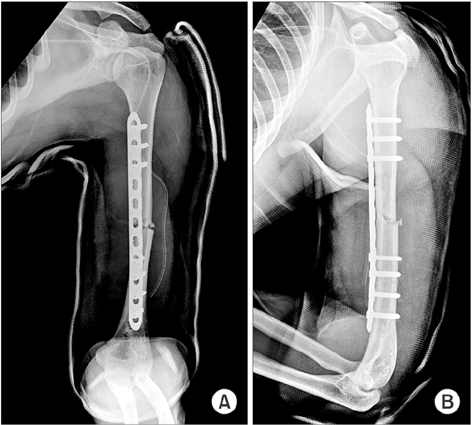
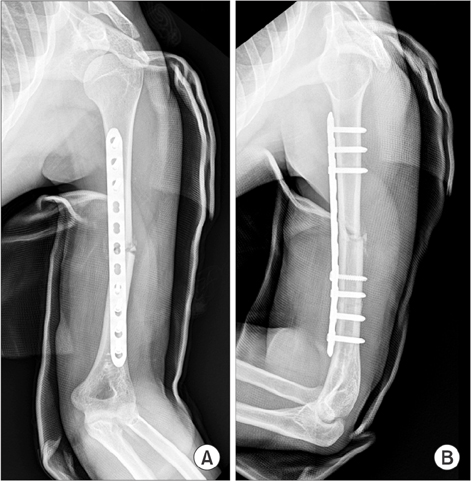
Minimally Invasive Plate Osteosynthesis Using a Screw Compression Method for Treatment of Humeral Shaft Fractures
- Affiliations
-
- 1Department of Orthopedic Surgery, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea. shkoshko@naver.com, fissura@naver.com
- KMID: 2412252
- DOI: http://doi.org/10.4055/cios.2017.9.4.506
Abstract
- BACKGROUND
This study aims to compare the surgical outcomes of open reduction and internal fixation (ORIF) and minimally invasive plate osteosynthesis (MIPO) using a screw compression method in simple humeral shaft fractures.
METHODS
This retrospective study was performed with 50 patients who had surgical interventions for the treatment of simple humeral shaft fractures and had follow-ups of at least 12 months in Ulsan University Hospital between August 2008 and June 2015. Group 1 included 23 patients treated with ORIF and group 2 included 27 patients treated with the MIPO technique using a locking screw plate. The time to clinical/radiographic union, the joint range of motion (ROM), and function were evaluated.
RESULTS
The average time to clinical/radiographic bone union was shorter in group 2 (12.0 ± 3.7 weeks/14.8 ± 2.0 weeks in group 1 and 9.4 ± 1.3 weeks/12.0 ± 3.3 weeks in group 2; p = 0.022/p = 0.034). Shoulder and elbow joint function evaluated by joint ROM and visual analogue scale (VAS), Korean Shoulder Elbow Society (KSS), American Shoulder and Elbow Surgeons (ASES), and the University of California at Los Angeles (UCLA) scores was excellent in both groups. On the average shoulder ROM at 12 months after the operation, group 1 had forward elevation of 160°, external rotation of 30° in adduction and lumbar vertebra 10 level in internal rotation and group 2 had forward elevation of 170°, external rotation of 35° in adduction and lumbar vertebra 9 level in internal rotation. The mean VAS, KSS, ASES, and UCLA scores were 2.8, 87.0 ± 0.9, 89.4 ± 0.9, and 31.0 ± 1.4, respectively, in group 1 and 1.7, 89.1 ± 2.7, 91.0 ± 1.6, and 32.4 ± 3.2, respectively, in group 2. There were statistically significant intergroup differences in VAS score (p = 0.011). There were significantly less postoperative infections in group 2 (three cases, 10.7% in group 1 and 0 case in group 2; p = 0.041) although all of them were superficial infections and well-treated by an average 4-week course of antibiotics (range, 2 to 6 weeks).
CONCLUSIONS
MIPO using a screw compression method in simple humeral shaft fractures demonstrated superior efficacy to ORIF in terms of the time to clinical/radiographic union, pain score, and postoperative infection rate.
MeSH Terms
-
Adult
Aged
Bone Plates
Bone Screws
Diaphyses/injuries/surgery
Elbow Joint/physiopathology
Female
Fracture Fixation, Internal/instrumentation/*methods
Fracture Healing
Humans
Humeral Fractures/diagnostic imaging/*surgery
Male
Middle Aged
Minimally Invasive Surgical Procedures/adverse effects/*methods
*Open Fracture Reduction/adverse effects
Radiography
Range of Motion, Articular
Retrospective Studies
Rotation
Shoulder Joint/physiopathology
Surgical Wound Infection/etiology
Time Factors
Treatment Outcome
Figure
Reference
-
1. Volgas DA, Stannard JP, Alonso JE. Nonunions of the humerus. Clin Orthop Relat Res. 2004; (419):46–50.
Article2. Fears RL, Gleis GE, Seligson D. Diagnosis and treatment of complications: fractures of the diaphyseal humerus. In : Browner BD, Jupiter JB, Levine AM, Trafton PG, editors. Skeletal trauma: fractures, dislocations, ligamentous injuries. Toronto: WB Saunders;1998. p. 567–578.3. Gregory PR. Fractures of the humeral shaft. In : Rockwood CA, Green DP, Heckman JD, Bucholz RW, editors. Rockwood and Green's fractures in adults. Philadelphia, PA: Lippincott Williams & Wilkins;2002. p. 973–976.4. Schemitsch EH, Bhandari M. Fractures of the diaphyseal humerus. In : Browner BD, Jupiter JB, Levine AM, Trafton PG, editors. Skeletal trauma: basic science, management, and reconstruction. Toronto: WB Saunders;2003. p. 1481–1511.5. McKee MD. Fractures of the shaft of the humerus. In : Bucholz RW, Heckman JD, Court-Brown C, Koval KJ, Tornetta P, Wirth MA, editors. Rockwood and Green's fractures in adults. Philadelphia, PA: Lippincott Williams & Wilkins;2006. p. 1117–1159.6. Bae SW, Kim WJ, Song BY, Choi NH, Lee JH. Postoperative functional assessments in adult humerus shaft fractures: comparison among plates and screws, intramedullary nail and external fixator. J Korean Soc Fract. 2001; 14(2):228–235.
Article7. Byun YS. Minimally invasive plate osteosynthesis, MIPO. J Korean Fract Soc. 2007; 20(1):99–114.
Article8. Sohn HS, Shin SJ. Minimally invasive plate osteosynthesis for proximal humeral fractures: clinical and radiologic outcomes according to fracture type. J Shoulder Elbow Surg. 2014; 23(9):1334–1340.
Article9. Shin SJ, Sohn HS, Do NH. Minimally invasive plate osteosynthesis of humeral shaft fractures: a technique to aid fracture reduction and minimize complications. J Orthop Trauma. 2012; 26(10):585–589.10. Xue Z, Jiang C, Hu C, Qin H, Ding H, An Z. Effects of different surgical techniques on mid-distal humeral shaft vascularity: open reduction and internal fixation versus minimally invasive plate osteosynthesis. BMC Musculoskelet Disord. 2016; 17:370.
Article11. Kim JW, Oh CW, Byun YS, Kim JJ, Park KC. A prospective randomized study of operative treatment for noncomminuted humeral shaft fractures: conventional open plating versus minimal invasive plate osteosynthesis. J Orthop Trauma. 2015; 29(4):189–194.
Article12. Moon JG, Kwon HN, Biraris S, Shon WY. Minimally invasive plate osteosynthesis using a helical plate for metadiaphyseal complex fractures of the proximal humerus. Orthopedics. 2014; 37(3):e237–e243.
Article13. Esmailiejah AA, Abbasian MR, Safdari F, Ashoori K. Treatment of humeral shaft fractures: minimally invasive plate osteosynthesis versus open reduction and internal fixation. Trauma Mon. 2015; 20(3):e26271.
Article14. Shetty MS, Kumar MA, Sujay K, Kini AR, Kanthi KG. Minimally invasive plate osteosynthesis for humerus diaphyseal fractures. Indian J Orthop. 2011; 45(6):520–526.
Article15. Gautier E, Sommer C. Guidelines for the clinical application of the LCP. Injury. 2003; 34:Suppl 2. B63–B76.
Article16. Mast J, Jakob R, Ganz R. Planning and reduction technique in fracture surgery. Berlin, Germany: Springer-Verlag;1989. p. 49–54.17. Perren SM. Evolution of the internal fixation of long bone fractures: the scientific basis of biological internal fixation: choosing a new balance between stability and biology. J Bone Joint Surg Br. 2002; 84(8):1093–1110.18. Ruedi TP, Murphy WM. AO principles of fracture management. Stuttgart, Germany: Thieme;2000. p. 68–75.19. Tong GO, Bavonratanavech S. Minimally invasive plate osteosynthesis (MIPO): concepts and cases presented by AO East Aisa. Stuttgart, Germany: Thieme;2007. p. 99–108.20. Wagner M. General principles for the clinical use of the LCP. Injury. 2003; 34:Suppl 2. B31–B42.
Article21. Collinge C, Sanders R, DiPasquale T. Treatment of complex tibial periarticular fractures using percutaneous techniques. Clin Orthop Relat Res. 2000; (375):69–77.
Article22. Krettek C, Schandelmaier P, Miclau T, Tscherne H. Minimally invasive percutaneous plate osteosynthesis (MIPPO) using the DCS in proximal and distal femoral fractures. Injury. 1997; 28:Suppl 1. A20–A30.
Article23. Schutz M, Muller M, Krettek C, et al. Minimally invasive fracture stabilization of distal femoral fractures with the LISS: a prospective multicenter study. Results of a clinical study with special emphasis on difficult cases. Injury. 2001; 32:Suppl 3. SC48–SC54.
Article24. Stannard JP, Wilson TC, Volgas DA, Alonso JE. Fracture stabilization of proximal tibial fractures with the proximal tibial LISS: early experience in Birmingham, Alabama (USA). Injury. 2003; 34:Suppl 1. A36–A42.
Article25. Jung SW. Indirect reduction maneuver and minimally invasive approach for displaced proximal humerus fractures in elderly patients. Clin Orthop Surg. 2013; 5(1):66–73.
Article26. Park J, Jeong SY. Complications and outcomes of minimally invasive percutaneous plating for proximal humeral fractures. Clin Orthop Surg. 2014; 6(2):146–152.
Article27. Kobayashi M, Watanabe Y, Matsushita T. Early full range of shoulder and elbow motion is possible after minimally invasive plate osteosynthesis for humeral shaft fractures. J Orthop Trauma. 2010; 24(4):212–216.
Article28. Apivatthakakul T, Arpornchayanon O, Bavornratanavech S. Minimally invasive plate osteosynthesis (MIPO) of the humeral shaft fracture. Is it possible? A cadaveric study and preliminary report. Injury. 2005; 36(4):530–538.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Minimally Invasive Plate Osteosynthesis for Humeral Proximal or Distal Shaft Fractures Using a 3.5/5.0 Metaphyseal Locking Plate
- Positional Screw Effect in the Treatment of Humeral Shaft Fractures Using a Minimally Invasive Plate Osteosynthesis Technique
- Minimally Invasive Anterior Plating of Humeral Shaft Fractures
- Comparison between minimally invasive plate osteosynthesis and the deltopectoral approach with allogenous fibular bone graft in proximal humeral fractures
- Comparison of Results of Minimally Invasive Plate Osteosynthesis according to Types of Locking Plate in Distal Femoral Fractures