J Korean Fract Soc.
2012 Oct;25(4):305-309. 10.12671/jkfs.2012.25.4.305.
Minimally Invasive Plate Osteosynthesis for Humeral Proximal or Distal Shaft Fractures Using a 3.5/5.0 Metaphyseal Locking Plate
- Affiliations
-
- 1Department of Orthopedic Surgery, Inje University Ilsan Paik Hospital, Goyang, Korea. osd11@paik.ac.kr
- KMID: 1434071
- DOI: http://doi.org/10.12671/jkfs.2012.25.4.305
Abstract
- PURPOSE
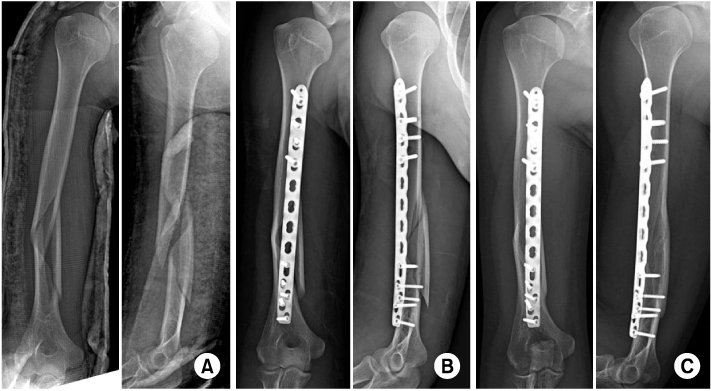
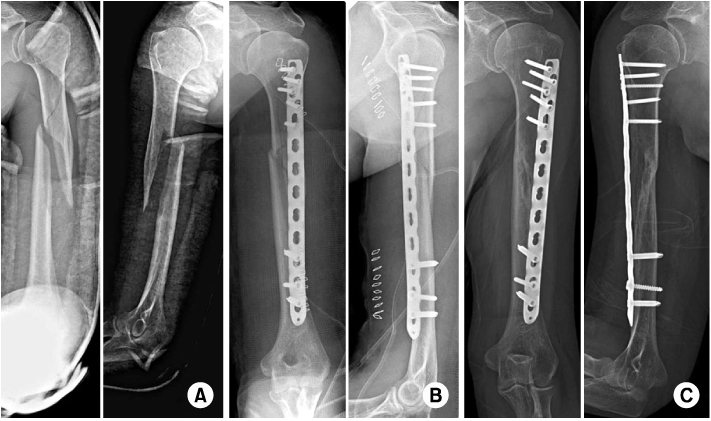
Our study aimed to investigate the clinical and radiological results of humerus proximal or distal shaft fractures treated with minimally invasive plate osteosynthesis (MIPO) using a 3.5/5.0 metaphyseal locking plate.
MATERIALS AND METHODS
We reviewed the clinical and radiographic records of 17 patients with humeral proximal or distal shaft fractures who had undergone 3.5/5.0 metaphyseal locking plate osteosynthesis with a minimally invasive technique. We evaluated the results with respect to the anatomical reduction and union of the humerus shaft fracture through radiologic studies. We also evaluated the clinical results using the motion of shoulder and elbow functional outcome, American Shoulder and Elbow Surgeons (ASES) score, Mayo elbow performance score (MEPS), and postoperative complications.
RESULTS
Complete union was achieved in all cases. The mean union time was 14.2 weeks. According to the functional outcome rated by the ASES score and MEPS, 15 cases were considered excellent and 2 cases were good. There were no cases of surgically-related complications like metal failure, loss of anatomical reduction, or postoperative nerve injuries.
CONCLUSION
Using a 5.0 metaphyseal locking plate for humerus shaft fracture has the limitation that difficulties can arise in achieving sufficient screw fixation for small bony fragments. The 3.5/5.0 metaphyseal locking plate used in MIPO for humerus 1/3 proximal or distal shaft fractures was concluded to give good clinical and radiologic results.
Keyword
Figure
Cited by 1 articles
-
Polarus Intramedullary Nail for Proximal Humeral and Humeral Shaft Fractures in Elderly Patients with Osteoporosis
Youn-Soo Hwang, Kwang-Yeol Kim, Hyung-Chun Kim, Su-Han Ahn, Dong-Eun Lee
J Korean Fract Soc. 2013;26(1):14-20. doi: 10.12671/jkfs.2013.26.1.14.
Reference
-
1. Ahn HS, Cho YH, Byun YS, Kwon DY, Nam SO, Kim DY. Elbow function and complications after internal fixation for fractures of the distal humerus. J Korean Fract Soc. 2006. 19:56–61.
Article2. Apivatthakakul T, Patiyasikan S, Luevitoonvechkit S. Danger zone for locking screw placement in minimally invasive plate osteosynthesis (MIPO) of humeral shaft fractures: a cadaveric study. Injury. 2010. 41:169–172.
Article3. Bono CM, Grossman MG, Hochwald N, Tornetta P 3rd. Radial and axillary nerves. Anatomic considerations for humeral fixation. Clin Orthop Relat Res. 2000. (373):259–264.
Article4. Chapman JR, Henley MB, Agel J, Benca PJ. Randomized prospective study of humeral shaft fracture fixation: intramedullary nails versus plates. J Orthop Trauma. 2000. 14:162–166.
Article5. Flinkkilä T, Hyvönen P, Lakovaara M, Linden T, Ristiniemi J, Hämäläinen M. Intramedullary nailing of humeral shaft fractures. A retrospective study of 126 cases. Acta Orthop Scand. 1999. 70:133–136.
Article6. Ha SS, Kim JY, Hong KD, Sim JC, Kang JH, Park KH. Operative treatment with locking compression plate (LCP) in proximal humerus fracture. J Korean Shoulder Elbow Soc. 2008. 11:137–142.
Article7. Kobayashi M, Watanabe Y, Matsushita T. Early full range of shoulder and elbow motion is possible after minimally invasive plate osteosynthesis for humeral shaft fractures. J Orthop Trauma. 2010. 24:212–216.
Article8. Lee HJ, Oh CW. Operative treatment of humerus shaft fracture: conventional open plating or minimally invasive plate osteosynthesis. J Korean Fract Soc. 2012. 25:155–162.
Article9. Livani B, Belangero WD. Bridging plate osteosynthesis of humeral shaft fractures. Injury. 2004. 35:587–595.
Article10. Michener LA, McClure PW, Sennett BJ. American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form, patient self-report section: reliability, validity, and responsiveness. J Shoulder Elbow Surg. 2002. 11:587–594.
Article11. Rommens PM, Blum J, Runkel M. Retrograde nailing of humeral shaft fractures. Clin Orthop Relat Res. 1998. (350):26–39.
Article12. Shin SJ, Do NH, Song MH, Sohn HS. Minimal invasive plate osteosynthesis in proximal humerus fractures. Clin Should Elbow. 2010. 13:202–208.
Article13. Shin SJ, Sohn HS, Do NH, Kang SS, Baek KY. Minimally invasive plate osteosynthesis of proximal, middle and distal humerus fractures. J Korean Orthop Assoc. 2010. 45:448–455.
Article14. Vander Griend R, Tomasin J, Ward EF. Open reduction and internal fixation of humeral shaft fractures. Results using AO plating techniques. J Bone Joint Surg Am. 1986. 68:430–433.
Article15. Zhiquan A, Bingfang Z, Yeming W, Chi Z, Peiyan H. Minimally invasive plating osteosynthesis (MIPO) of middle and distal third humeral shaft fractures. J Orthop Trauma. 2007. 21:628–633.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Minimally Invasive Percutaneous Plate Stabilization Using a Medial Locking Plate for Proximal Tibial Fractures: Technical Note
- Comparison of Results of Minimally Invasive Plate Osteosynthesis according to Types of Locking Plate in Distal Femoral Fractures
- Minimally Invasive Plate Osteosynthesis of Proximal, Middle and Distal Humerus Fractures
- Axial Malalignment after Minimally Invasive Plate Osteosynthesis in Distal Femur Fractures with Metaphyseal Comminution
- Analysis of the Result Treated with Locking Compression Plate-Distal Tibia and Zimmer Periarticular Locking Plate in Distal Tibia Fracture