Clin Orthop Surg.
2017 Dec;9(4):472-479. 10.4055/cios.2017.9.4.472.
The Validation of Ultrasound-Guided Target Segment Identification in Thoracic Spine as Confirmed by Fluoroscopy
- Affiliations
-
- 1Department of Orthopedic Surgery, Kwangju Christian Hospital, Gwangju, Korea. stemcellchoi@gmail.com
- KMID: 2412248
- DOI: http://doi.org/10.4055/cios.2017.9.4.472
Abstract
- BACKGROUND
The role of ultrasound in the thoracic spine has been underappreciated, partly because of the relative efficacy of the landmark-guided technique and the limitation of imaging through the narrow acoustic windows produced by the bony framework of thoracic spine. The aim of this study was to make a comparison between the 12th rib and the spinous process of C7 as a landmark for effective ultrasound-guided target segment identification in the thoracic spine.
METHODS
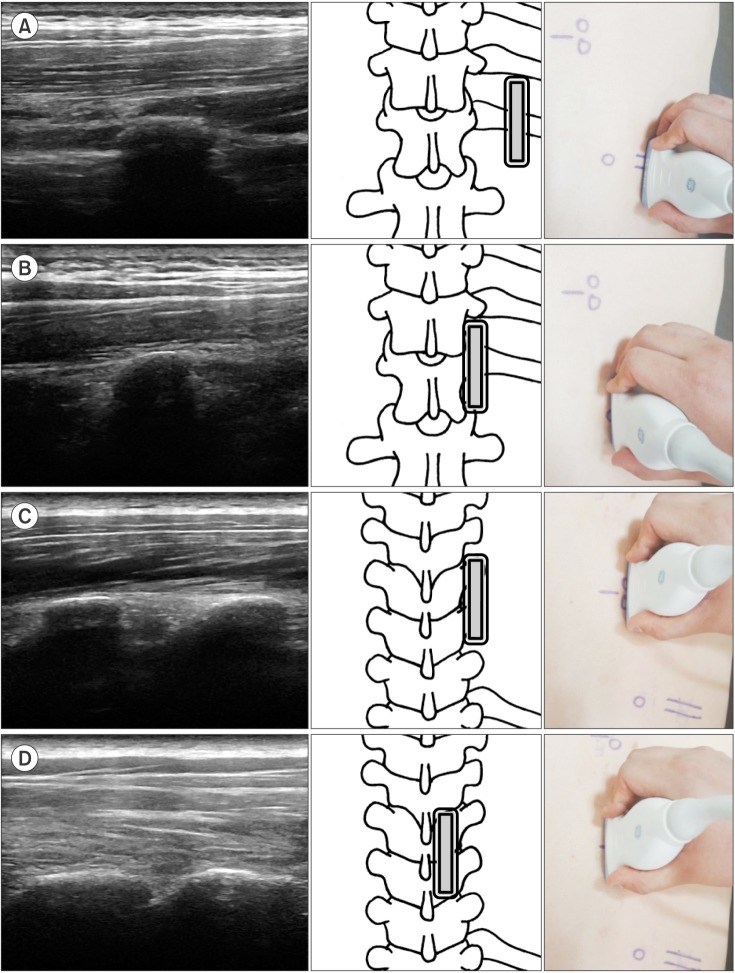
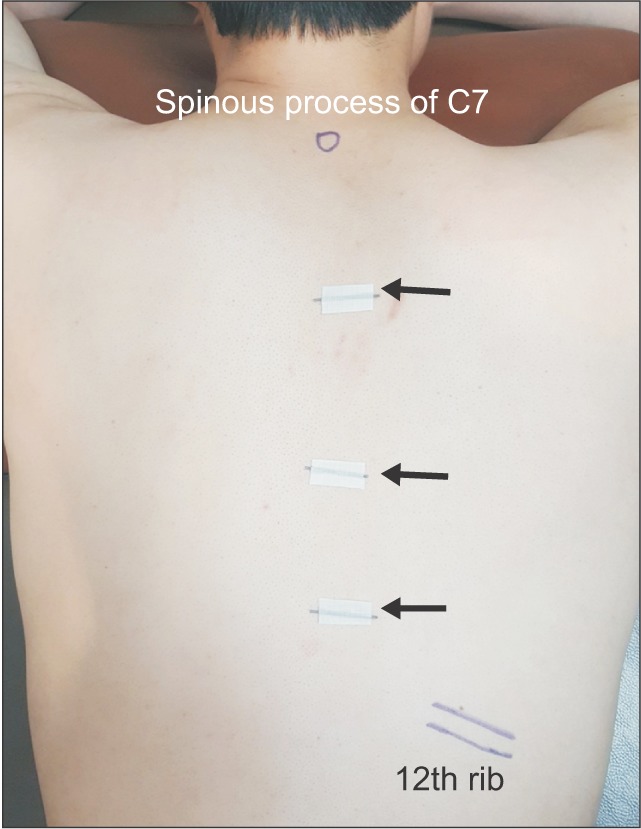
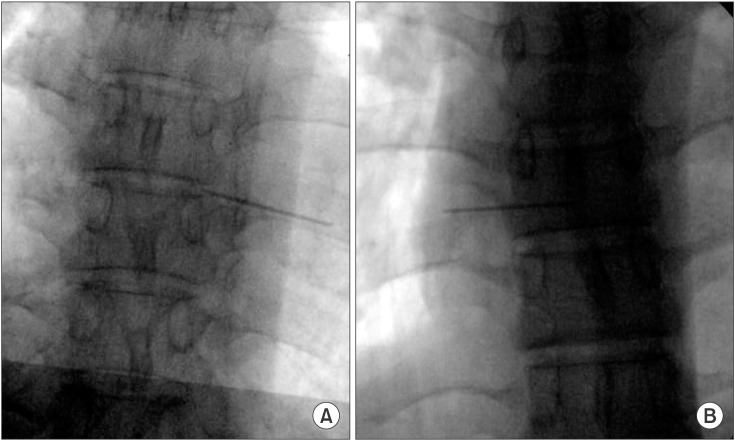
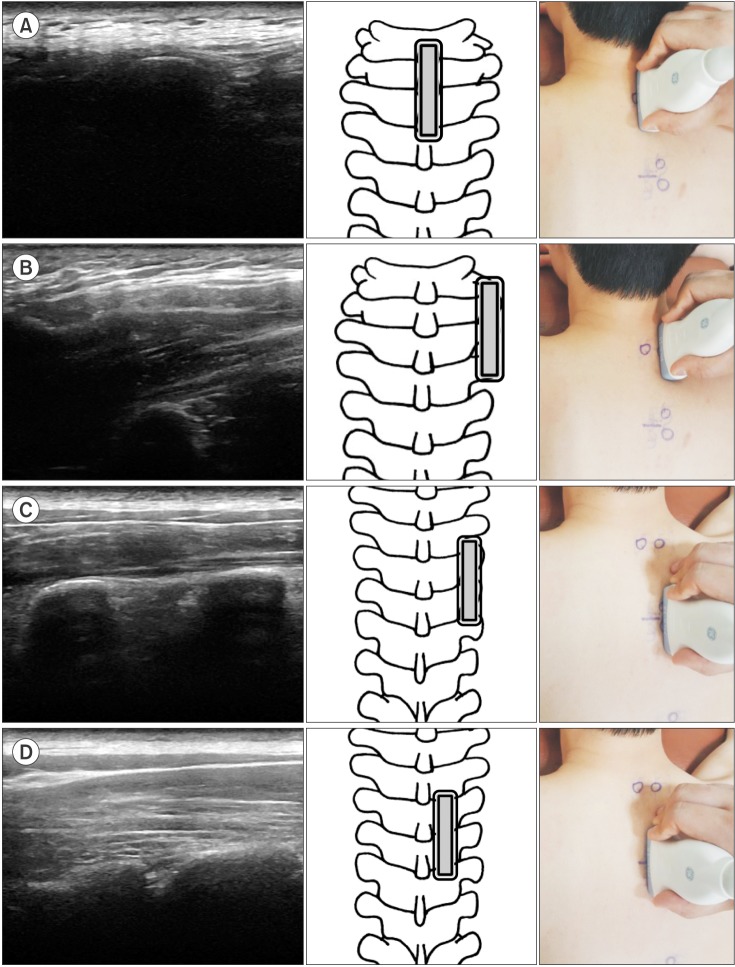
Ultrasonography of 44 thoracic spines was performed and the same procedure was carried out 1 week later again. The target segments (T3-4, T7-8, and T10-11) were identified using the 12th rib (group 1) or the spinous process of C7 (group 2) as a starting landmark. Ultrasound scanning was done proximally (group 1) or distally (group 2) toward the target transverse process and further medially and slightly superior to the target thoracic facet. Then, a metal marker was placed on the T3-4, T7-8, and T10-11 and the location of each marker was confirmed by fluoroscopy.
RESULTS
In the total 132 segments, sonographic identification was confirmed to be successful with fluoroscopy in 84.1% in group 1 and 56.8% in group 2. Group 1 had a greater success rate in ultrasound-guided target segment identification than group 2 (p = 0.001), especially in T10-11 (group 1, 93.2%; group 2, 43.2%; p = 0.001) and T7-8 (group 1, 86.4%; group 2, 56.8%; p = 0.002). The intrarater reliability of ultrasound-guided target segment identification was good (group 1, r = 0.76; group 2, r = 0.82), showing no difference between right and left sides. Ultrasound-guided target segment identification was more effective in the non-obese subjects (p = 0.001), especially in group 1.
CONCLUSIONS
Ultrasound-guided detection using the 12th rib as a starting landmark for scanning could be a promising technique for successful target segment identification in the thoracic spine.
Keyword
MeSH Terms
Figure
Reference
-
1. Linton SJ, Hellsing AL, Hallden K. A population-based study of spinal pain among 35-45-year-old individuals: prevalence, sick leave, and health care use. Spine (Phila Pa 1976). 1998; 23(13):1457–1463. PMID: 9670397.2. Leboeuf-Yde C, Nielsen J, Kyvik KO, Fejer R, Hartvigsen J. Pain in the lumbar, thoracic or cervical regions do age and gender matter A population-based study of 34,902 Danish twins 20-71 years of age. BMC Musculoskelet Disord. 2009; 10:39. PMID: 19379477.
Article3. Schnabel A, Reichl SU, Kranke P, Pogatzki-Zahn EM, Zahn PK. Efficacy and safety of paravertebral blocks in breast surgery: a meta-analysis of randomized controlled trials. Br J Anaesth. 2010; 105(6):842–852. PMID: 20947592.
Article4. Manchikanti L, Singh V, Falco FJ, Cash KA, Pampati V, Fellows B. Comparative effectiveness of a one-year follow-up of thoracic medial branch blocks in management of chronic thoracic pain: a randomized, double-blind active controlled trial. Pain Physician. 2010; 13(6):535–548. PMID: 21102966.5. Park KD, Jee H, Nam HS, et al. Effect of medial branch block in chronic facet joint pain for osteoporotic compression fracture: one year retrospective study. Ann Rehabil Med. 2013; 37(2):191–201. PMID: 23705113.
Article6. Mitra R, Do H, Alamin T, Cheng I. Facet pain in thoracic compression fractures. Pain Med. 2010; 11(11):1674–1677. PMID: 21029349.
Article7. Moon SH, Lee S, Lee JI. Ultrasound-guided intervention in thoracic spine. J Korean Orthop Assoc. 2015; 50(2):93–106.
Article8. Stulc SM, Hurdle MF, Pingree MJ, Brault JS, Porter CA. Ultrasound-guided thoracic facet injections: description of a technique. J Ultrasound Med. 2011; 30(3):357–362. PMID: 21357557.9. O Riain SC, Donnell BO, Cuffe T, Harmon DC, Fraher JP, Shorten G. Thoracic paravertebral block using real-time ultrasound guidance. Anesth Analg. 2010; 110(1):248–251. PMID: 19933536.10. Deimel GW, Hurdle MF, Murthy N, Cartwright JA, Smith J, Pingree MJ. Sonographically guided costotransverse joint injections: a computed tomographically controlled cadaveric feasibility study. J Ultrasound Med. 2013; 32(12):2083–2089. PMID: 24277889.11. Marhofer P, Kettner SC, Hajbok L, Dubsky P, Fleischmann E. Lateral ultrasound-guided paravertebral blockade: an anatomical-based description of a new technique. Br J Anaesth. 2010; 105(4):526–532. PMID: 20685684.
Article12. Choi DH, Jung HG, Lee JH, Park JH, Choi YS. Effectiveness of Doppler image of the vertebral artery as an anatomical landmark for identification of ultrasound-guided target level in cervical spine. Asian Spine J. 2015; 9(5):683–688. PMID: 26435784.
Article13. Narouze SN, Vydyanathan A, Kapural L, Sessler DI, Mekhail N. Ultrasound-guided cervical selective nerve root block: a fluoroscopy-controlled feasibility study. Reg Anesth Pain Med. 2009; 34(4):343–348. PMID: 19574867.14. Greher M, Scharbert G, Kamolz LP, et al. Ultrasound-guided lumbar facet nerve block: a sonoanatomic study of a new methodologic approach. Anesthesiology. 2004; 100(5):1242–1248. PMID: 15114223.15. Galiano K, Obwegeser AA, Bodner G, et al. Ultrasound-guided periradicular injections in the middle to lower cervical spine: an imaging study of a new approach. Reg Anesth Pain Med. 2005; 30(4):391–396. PMID: 16032592.
Article16. Mehta MH, Patel RV, Mehta LV, Bhatt YC. Congenital absence of ribs. Indian Pediatr. 1992; 29(9):1149–1152. PMID: 1452315.17. Saranteas T. Limitations in ultrasound imaging techniques in anesthesia: obesity and muscle atrophy? Anesth Analg. 2009; 109(3):993–994. PMID: 19690282.
Article18. Rauch S, Kasuya Y, Turan A, Neamtu A, Vinayakan A, Sessler DI. Ultrasound-guided lumbar medial branch block in obese patients: a fluoroscopically confirmed clinical feasibility study. Reg Anesth Pain Med. 2009; 34(4):340–342. PMID: 19585701.19. Ueshima H, Kubo K, Sakamoto S, et al. A case of the transversus abdominis plane block in a super obese patient using a convex probe. Masui. 2013; 62(4):439–441. PMID: 23697197.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ultrasound-Guided Intervention in Thoracic Spine
- The Validation of Ultrasound-Guided Lumbar Facet Nerve Blocks as Confirmed by Fluoroscopy
- Ultrasound-guided interventions for spinal pain
- Ultrasound-Guided Intervention in Lumbar Spine
- Feasibility of Ultrasound-Guided Lumbar and S1 Nerve Root Block: A Cadaver Study