Prevalence of unrecognized depression in patients with chronic pain without a history of psychiatric diseases
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Seoul National University Bundang Hospital, Seongnam, Korea. painfree@snubh.org
- 2Department of Neuropsychiatry, Seoul National University Bundang Hospital, Seongnam, Korea.
- KMID: 2410834
- DOI: http://doi.org/10.3344/kjp.2018.31.2.116
Abstract
- BACKGROUND
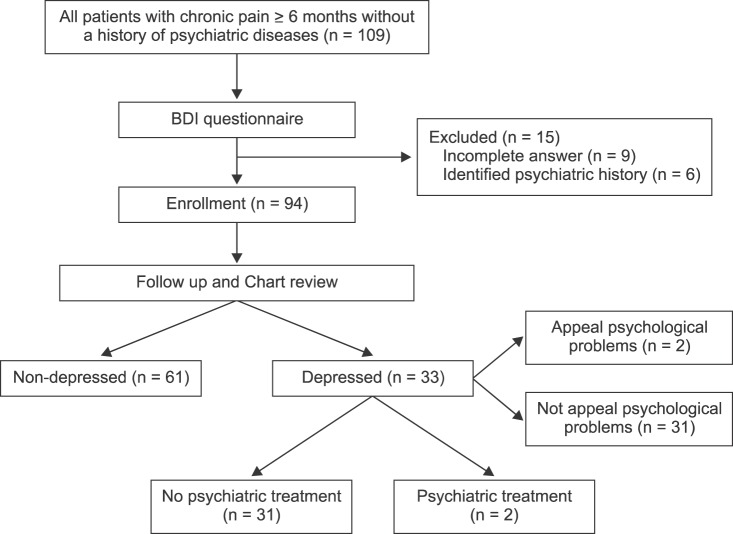
We aimed to investigate the prevalence of unrecognized depression in patients with chronic pain, but with no history of psychiatric diseases.
METHODS
Patients with chronic pain who did not have a history of psychiatric disease were selected for this study. The Beck Depression Index (BDI) was used to evaluate depression. Participants' socio-demographic characteristics and pain-related characteristics were also recorded.
RESULTS
The study included 94 consecutive patients with chronic pain (28 men and 66 women). Based on the BDI scores, 33/94 (35.1%) patients with chronic pain had comorbid depression. The prevalence of depression was significantly higher in our cohort than it was in the general population (P < 0.001). The standardized incidence ratio, adjusted for age and sex, was 2.77 in men and 2.60 in women. Patients who were unmarried (odds ratio [OR] = 3.714, P = 0.044), and who had subjective sleep disturbance (OR = 8.885, P < 0.001), were more likely to have moderate to severe depression. Patients with high education levels (OR = 0.244, P = 0.016), and who were economically active (OR = 0.284, P = 0.023), were less likely to have moderate to severe depression.
CONCLUSIONS
Our results indicate that unrecognized depression in patients with chronic pain is common. Therefore, pain physicians should actively seek to identify these problems rather than relying on the patient to volunteer such information.
Keyword
MeSH Terms
Figure
Cited by 7 articles
-
The opioid epidemic and crisis in US: how about Korea?
Joon-Ho Lee
Korean J Pain. 2019;32(4):243-244. doi: 10.3344/kjp.2019.32.4.243.The phenomenology of pain in Parkinson’s disease
José Antonio Camacho-Conde, Víctor Manuel Campos-Arillo
Korean J Pain. 2020;33(1):90-96. doi: 10.3344/kjp.2020.33.1.90.Determinants of depression in non-cardiac chest pain patients: a cross sectional study
Hamidreza Roohafza, Niloufar Yavari, Awat Feizi, Azam Khani, Parsa Saneian, Sara Bagherieh, Fereshteh Sattar, Masoumeh Sadeghi
Korean J Pain. 2021;34(4):417-426. doi: 10.3344/kjp.2021.34.4.417.Cross-cultural adaptation and validation of the Turkish Yellow Flag Questionnaire in patients with chronic musculoskeletal pain
Meltem Koç, Zilan Bazancir, Hakan Apaydın, Burcu Talu, Kılıçhan Bayar
Korean J Pain. 2021;34(4):501-508. doi: 10.3344/kjp.2021.34.4.501.The effect of stabilization exercise on pain-related disability, sleep disturbance, and psychological status of patients with non-specific chronic low back pain
Ashiyat Kehinde Akodu, Oluwagbemisola Marian Akindutire
Korean J Pain. 2018;31(3):199-205. doi: 10.3344/kjp.2018.31.3.199.Mental health stigma: another enemy for defeat chronic pain
Joon Ho Lee
Korean J Pain. 2018;31(2):71-72. doi: 10.3344/kjp.2018.31.2.71.Impact of coronavirus disease 2019 on patients with chronic pain: multicenter study in Korea
Hyunji John, Yun Hee Lim, Sung Jun Hong, Jae Hun Jeong, Hey Ran Choi, Sun Kyung Park, Jung Eun Kim, Byung-soo Kim, Jae Hun Kim
Korean J Pain. 2022;35(2):209-223. doi: 10.3344/kjp.2022.35.2.209.
Reference
-
1. Pain terms: a list with definitions and notes on usage. Recommended by the IASP Subcommittee on Taxonomy. Pain. 1979; 6:249. PMID: 460932.2. Keogh E, Cochrane M. Anxiety sensitivity, cognitive biases, and the experience of pain. J Pain. 2002; 3:320–329. PMID: 14622756.
Article3. Gatchel RJ, Turk DC. Psychosocial factors in pain: critical perspectives. New York (NY): Guilford Press;1999.
Article4. Gaskin ME, Greene AF, Robinson ME, Geisser ME. Negative affect and the experience of chronic pain. J Psychosom Res. 1992; 36:707–713. PMID: 1432860.
Article5. Benjamin S, Morris S, McBeth J, Macfarlane GJ, Silman AJ. The association between chronic widespread pain and mental disorder: a population-based study. Arthritis Rheum. 2000; 43:561–567. PMID: 10728749.
Article6. Gureje O, Simon GE, Von Korff M. A cross-national study of the course of persistent pain in primary care. Pain. 2001; 92:195–200. PMID: 11323140.
Article7. Bair MJ, Robinson RL, Katon W, Kroenke K. Depression and pain comorbidity: a literature review. Arch Intern Med. 2003; 163:2433–2445. PMID: 14609780.8. Kim AR, Seo BB, Kim JM, Bae JI, Jang YH, Lee YC, et al. Beck depression inventory score and associated factors in Korean patients with lumbar spinal stenosis. Korean J Pain. 2007; 20:138–142.
Article9. Boakye PA, Olechowski C, Rashiq S, Verrier MJ, Kerr B, Witmans M, et al. A critical review of neurobiological factors involved in the interactions between chronic pain, depression, and sleep disruption. Clin J Pain. 2016; 32:327–336. PMID: 26035521.
Article10. Lamb SE, Guralnik JM, Buchner DM, Ferrucci LM, Hochberg MC, Simonsick EM, et al. Factors that modify the association between knee pain and mobility limitation in older women: the Women's Health and Aging Study. Ann Rheum Dis. 2000; 59:331–337. PMID: 10784513.
Article11. Croft PR, Papageorgiou AC, Ferry S, Thomas E, Jayson MI, Silman AJ. Psychologic distress and low back pain. Evidence from a prospective study in the general population. Spine (Phila Pa 1976). 1995; 20:2731–2737. PMID: 8747252.12. Burton AK, Tillotson KM, Main CJ, Hollis S. Psychosocial predictors of outcome in acute and subchronic low back trouble. Spine (Phila Pa 1976). 1995; 20:722–728. PMID: 7604349.
Article13. Arnow BA, Hunkeler EM, Blasey CM, Lee J, Constantino MJ, Fireman B, et al. Comorbid depression, chronic pain, and disability in primary care. Psychosom Med. 2006; 68:262–268. PMID: 16554392.
Article14. Cepoiu M, McCusker J, Cole MG, Sewitch M, Belzile E, Ciampi A. Recognition of depression by non-psychiatric physicians: a systematic literature review and meta-analysis. J Gen Intern Med. 2008; 23:25–36. PMID: 17968628.
Article15. Wancata J, Windhaber J, Bach M, Meise U. Recognition of psychiatric disorders in nonpsychiatric hospital wards. J Psychosom Res. 2000; 48:149–155. PMID: 10719131.
Article16. Kohli C, Kishore J, Agarwal P, Singh SV. Prevalence of unrecognised depression among outpatient department attendees of a rural hospital in delhi, India. J Clin Diagn Res. 2013; 7:1921–1925. PMID: 24179898.
Article17. Barney LJ, Griffiths KM, Jorm AF, Christensen H. Stigma about depression and its impact on help-seeking intentions. Aust N Z J Psychiatry. 2006; 40:51–54. PMID: 16403038.
Article18. Roeloffs C, Sherbourne C, Unützer J, Fink A, Tang L, Wells KB. Stigma and depression among primary care patients. Gen Hosp Psychiatry. 2003; 25:311–315. PMID: 12972221.
Article19. Rhee M, Lee Y, Park S, Shon C, Jeong Y, Hong S, et al. A standardization study of beck depression inventory I-Korean version (K-BDI): reliability and factor analysis. Korean J Psychopathol. 1995; 4:77–95.20. Love AW. Depression in chronic low back pain patients: diagnostic efficiency of three self-report questionnaires. J Clin Psychol. 1987; 43:84–89. PMID: 2951398.
Article21. Geisser ME, Roth RS, Robinson ME. Assessing depression among persons with chronic pain using the Center for Epidemiological Studies-Depression Scale and the Beck Depression Inventory: a comparative analysis. Clin J Pain. 1997; 13:163–170. PMID: 9186024.
Article22. Aragon T, Fay M, Wollschlaeger D. EpiTools: R package for epidemiologic data and graphics. Vienna: Comprehensive R Archive Network;2010.23. Ministry of Health and Welfare. Korea Health Statistics 2013: Korea National Health and Nutrition Examination Survey (KNHANESVI-1). Cheongju: Korea Centers for Disease Control and Prevention;2014.24. Cho M, Sung S, Shin S, Kim J, Jeon S, Kim M. The epidemiological survey of mental disorders in Korea. Seoul: Ministry of Health and Welfare.25. Goldman LS, Nielsen NH, Champion HC. Awareness, diagnosis, and treatment of depression. J Gen Intern Med. 1999; 14:569–580. PMID: 10491249.
Article26. O'Connor DW, Rosewarne R, Bruce A. Depression in primary care. 1: elderly patients' disclosure of depressive symptoms to their doctors. Int Psychogeriatr. 2001; 13:359–365. PMID: 11768382.27. Cho SJ, Lee JY, Hong JP, Lee HB, Cho MJ, Hahm BJ. Mental health service use in a nationwide sample of Korean adults. Soc Psychiatry Psychiatr Epidemiol. 2009; 44:943–951. PMID: 19294325.
Article28. Jang Y, Kim G, Hansen L, Chiriboga DA. Attitudes of older Korean Americans toward mental health services. J Am Geriatr Soc. 2007; 55:616–620. PMID: 17397442.
Article29. Menchetti M, Belvederi Murri M, Bertakis K, Bortolotti B, Berardi D. Recognition and treatment of depression in primary care: effect of patients' presentation and frequency of consultation. J Psychosom Res. 2009; 66:335–341. PMID: 19302892.
Article30. Bertakis KD, Azari R, Callahan EJ. Patient pain: its influence on primary care physician-patient interaction. Fam Med. 2003; 35:119–123. PMID: 12607809.31. Whooley MA. Screening for depression—A tale of two questions. JAMA Intern Med. 2016; 176:436–438. PMID: 26814016.
Article32. Whooley MA, Avins AL, Miranda J, Browner WS. Case-finding instruments for depression. Two questions are as good as many. J Gen Intern Med. 1997; 12:439–445. PMID: 9229283.33. Hahm BJ, Kim JK, Cho MJ. Prevalence, incidence, and risk factors of dementia and depressive disorders of the elderly residing in the community: a two stage one-year follow-up study. J Korean Geriatr Psychiatry. 1999; 3:140–148.34. Wilson KG, Eriksson MY, D'Eon JL, Mikail SF, Emery PC. Major depression and insomnia in chronic pain. Clin J Pain. 2002; 18:77–83. PMID: 11882770.
Article35. Gerrits MM, van Oppen P, van Marwijk HW, Penninx BW, van der Horst HE. Pain and the onset of depressive and anxiety disorders. Pain. 2014; 155:53–59. PMID: 24012953.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prevalence of chronic pain and contributing factors: a cross-sectional population-based study among 2,379 Iranian adolescents
- Psychosocial Factors in Patients with Chronic Kidney Disease
- Depressive Disorder in Patients with Chronic Pains
- Reported Histories of Abuse and Psychiatric Symptomatology in Women Psychiatric Outpatients
- Prevalence and Correlates of Depression in Older Koreans: Comparison of Young-old and Old-old