Korean J Radiol.
2018 Jun;19(3):397-409. 10.3348/kjr.2018.19.3.397.
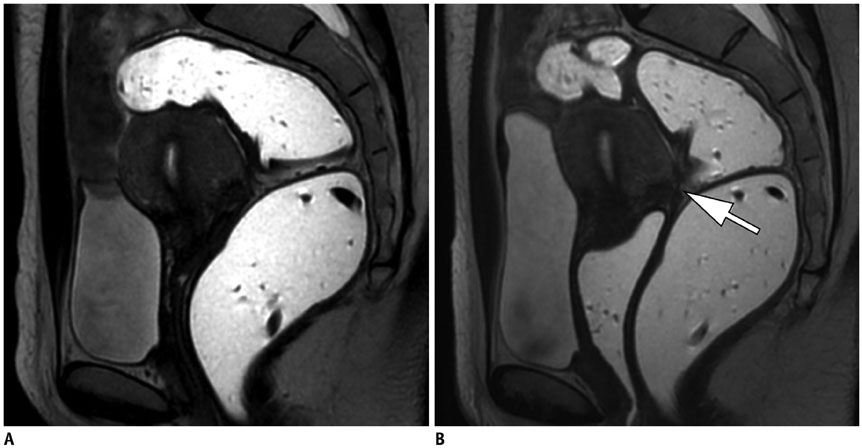
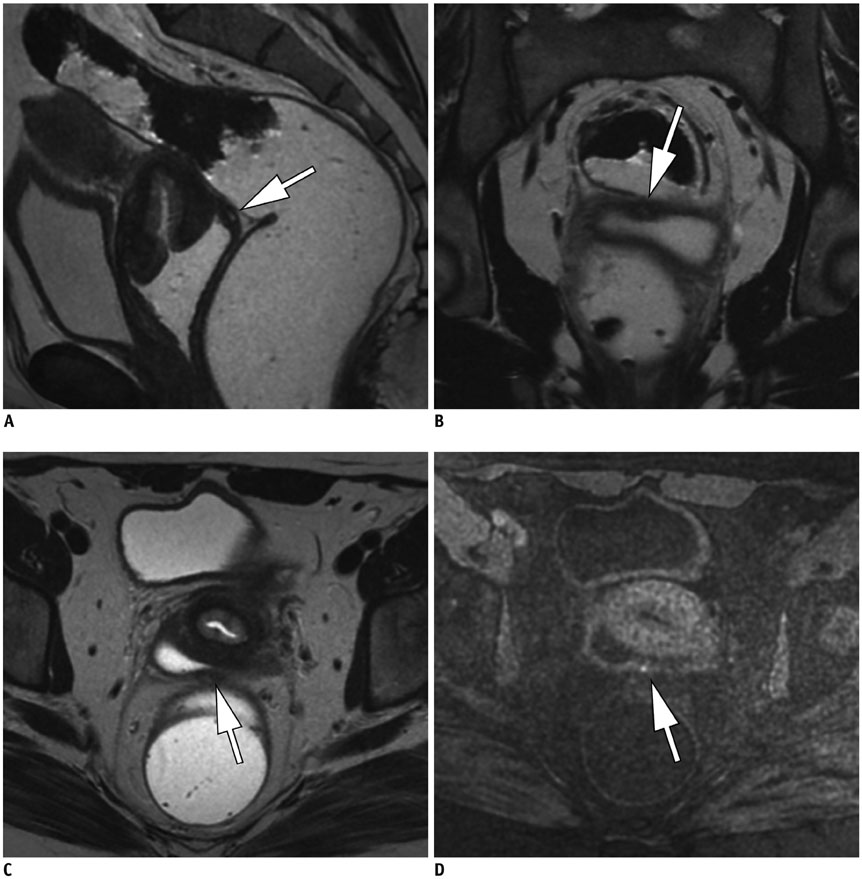
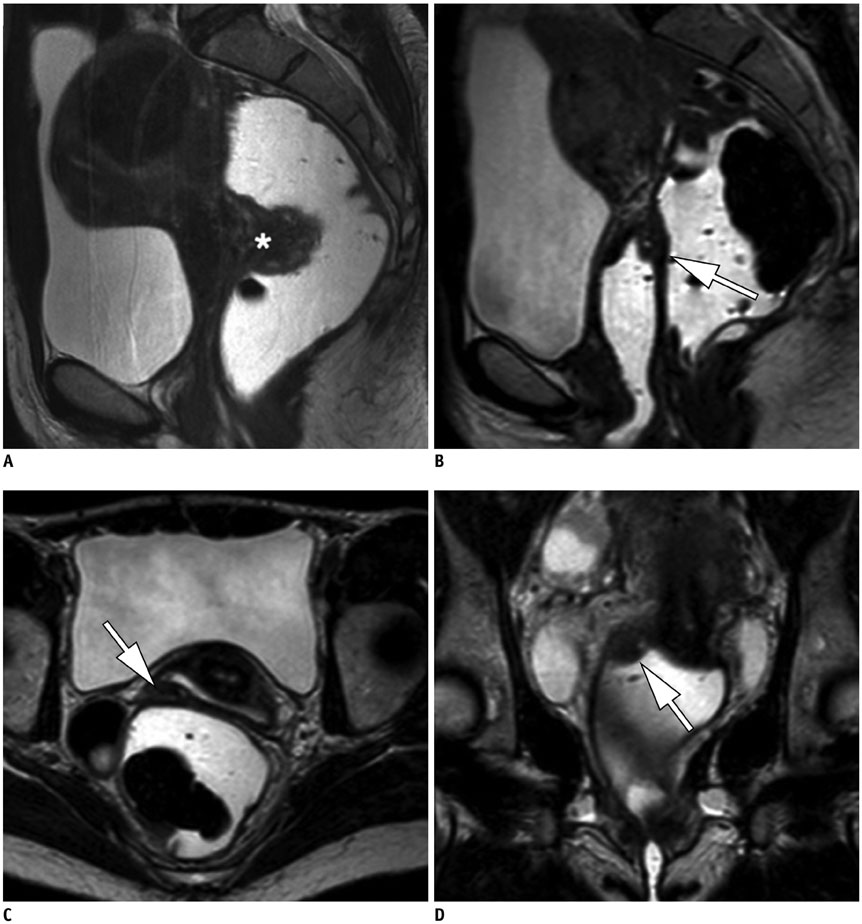
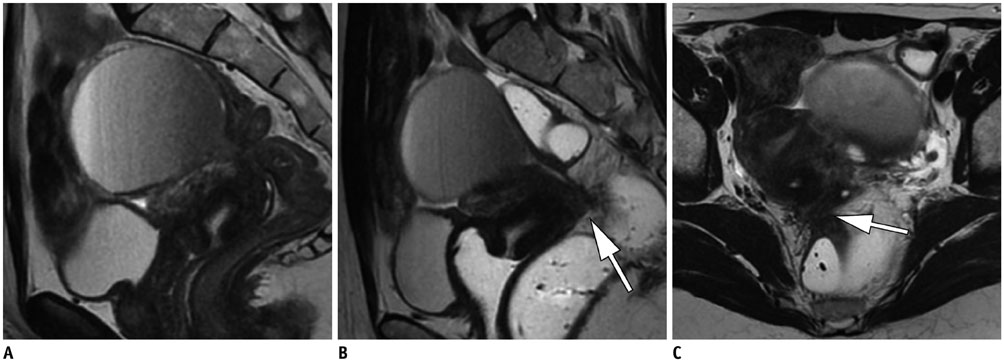
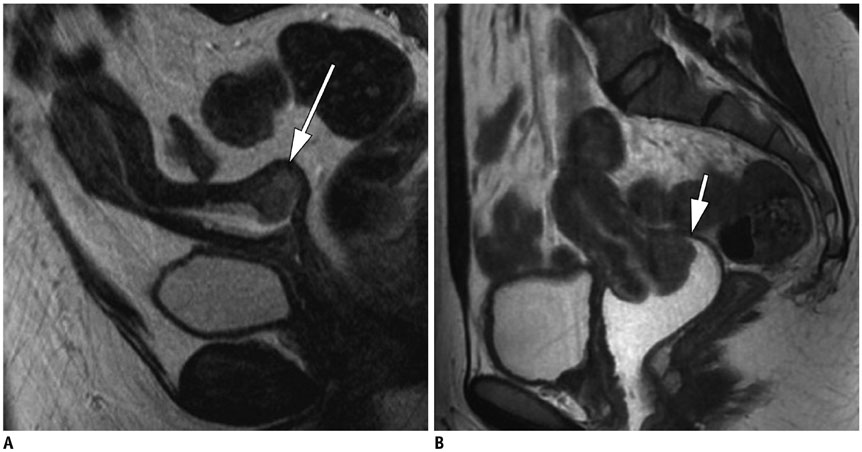
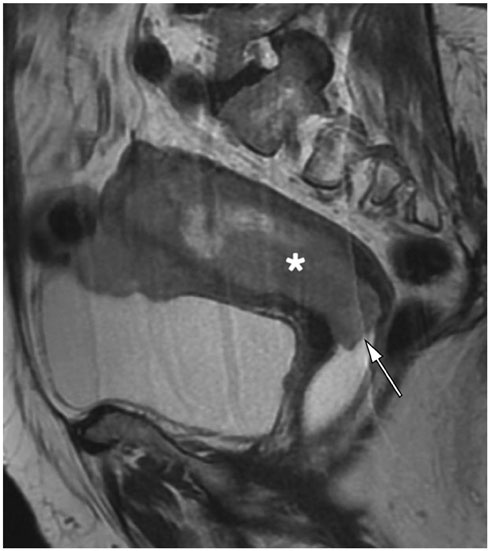
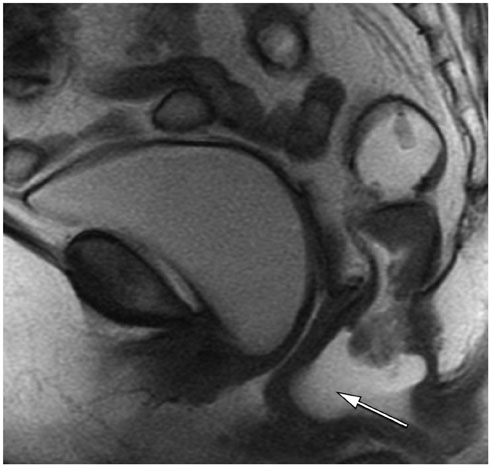
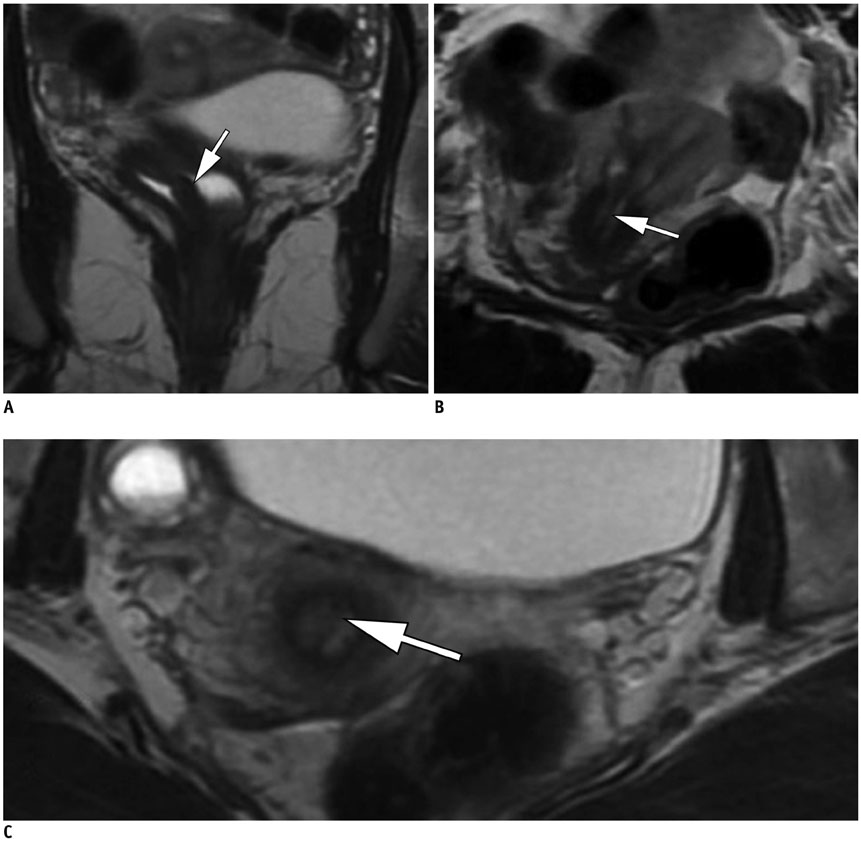
Pelvic MRI: Is Endovaginal or Rectal Filling Needed?
- Affiliations
-
- 1Department of Radiology, Centre Hospitalo-Universitaire de Reims, Reims 51092, France. constance.e@hotmail.fr
- 2Department of Radiology, Centre Hospitalier de Valenciennes, Valenciennes 59300, France.
- 3Department of Abdominal Imaging, Hôpital Lariboisière-APHP, Paris 75010, France.
- 4Department of Radiology, Hospices civils de Lyon, Centre hospitalier Lyon-Sud, Université Claude-Bernard Lyon 1, Pierre-Bénite 69495, France.
- KMID: 2410810
- DOI: http://doi.org/10.3348/kjr.2018.19.3.397
Abstract
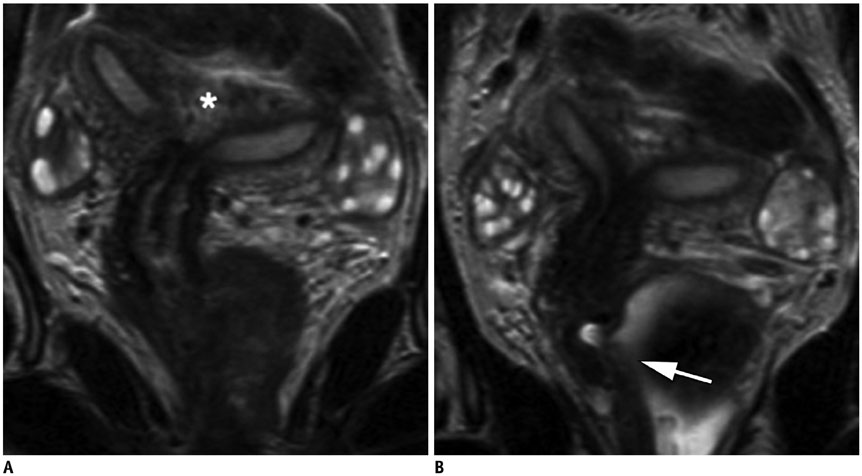
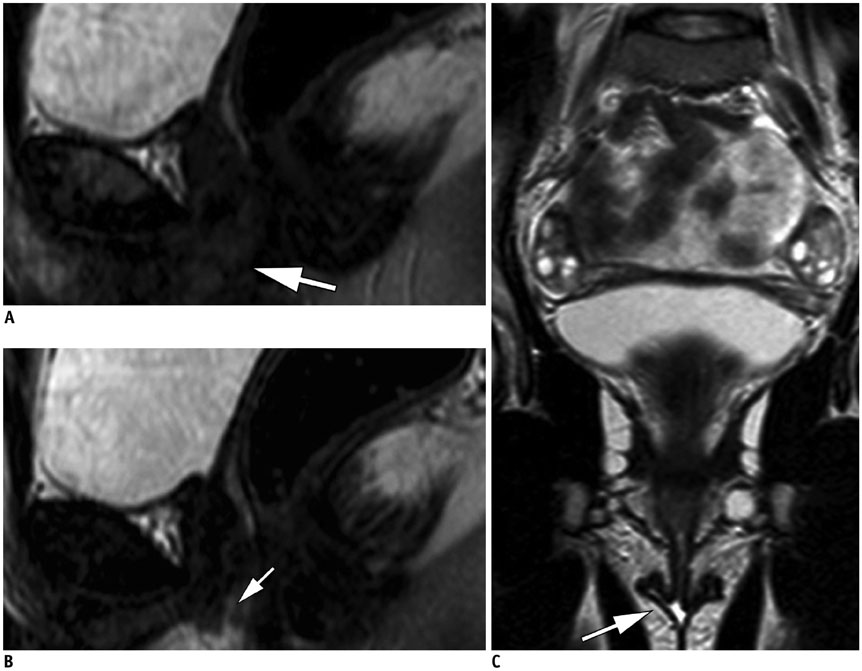
- Magnetic resonance imaging is the optimal modality for pelvic imaging. It is based on T2-weighted magnetic resonance (MR) sequences allowing uterine and vaginal cavity assessment as well as rectal evaluation. Anatomical depiction of these structures may benefit from distension, and conditions either developing inside the lumen of cavities or coming from the outside may then be better delineated and localized. The need for distension, either rectal or vaginal, and the way to conduct it are matters of debate, depending on indication for which the MR examination is being conducted. In this review, we discuss advantages and potential drawbacks of this technique, based on literature and our experience, in the evaluation of various gynecological and rectal diseases.
Keyword
Figure
Reference
-
1. Lienemann A, Fischer T. Functional imaging of the pelvic floor. Eur J Radiol. 2003; 47:117–122.
Article2. Bitti GT, Argiolas GM, Ballicu N, Caddeo E, Cecconi M, Demurtas G, et al. Pelvic floor failure: MR imaging evaluation of anatomic and functional abnormalities. Radiographics. 2014; 34:429–448.
Article3. Marchiolè P, Cittadini G, Sala P, Moioli M, Mathevet P, Capaccio E, et al. Pre- and post-operative work-up in patients affected by early cervical cancer and eligible for fertilitysparing treatment: role of MRI with saline hydrocolpos. Abdom Imaging. 2010; 35:271–279.
Article4. Maccioni F. Functional disorders of the ano-rectal compartment of the pelvic floor: clinical and diagnostic value of dynamic MRI. Abdom Imaging. 2013; 38:930–951.
Article5. Hetzer FH, Andreisek G, Tsagari C, Sahrbacher U, Weishaupt D. MR defecography in patients with fecal incontinence: imaging findings and their effect on surgical management. Radiology. 2006; 240:449–457.
Article6. Reiner CS, Weishaupt D. Dynamic pelvic floor imaging: MRI techniques and imaging parameters. Abdom Imaging. 2013; 38:903–911.
Article7. Reiner CS, Tutuian R, Solopova AE, Pohl D, Marincek B, Weishaupt D. MR defecography in patients with dyssynergic defecation: spectrum of imaging findings and diagnostic value. Br J Radiol. 2011; 84:136–144.
Article8. Maas M, Lambregts DM, Lahaye MJ, Beets GL, Backes W, Vliegen RF, et al. T-staging of rectal cancer: accuracy of 3.0 Tesla MRI compared with 1.5 Tesla. Abdom Imaging. 2012; 37:475–481.9. Ye F, Zhang H, Liang X, Ouyang H, Zhao X, Zhou C. Journal club: preoperative MRI evaluation of primary rectal cancer: intrasubject comparison with and without rectal distention. AJR Am J Roentgenol. 2016; 207:32–39.
Article10. Fiaschetti V, Crusco S, Meschini A, Cama V, Di Vito L, Marziali M, et al. Deeply infiltrating endometriosis: evaluation of retro-cervical space on MRI after vaginal opacification. Eur J Radiol. 2012; 81:3638–3645.
Article11. Chassang M, Novellas S, Bloch-Marcotte C, Delotte J, Toullalan O, Bongain A, et al. Utility of vaginal and rectal contrast medium in MRI for the detection of deep pelvic endometriosis. Eur Radiol. 2010; 20:1003–1010.
Article12. Novellas S, Marcotte Bloch C, Berthier F, Fournol M, Delotte J, Bongain A, et al. [Anatomy of the female pelvis on MRI: value of intravaginal contrast]. J Radiol. 2009; 90(7-8 Pt 1):819–824.13. Bazot M, Gasner A, Lafont C, Ballester M, Dara E. Deep pelvic endometriosis: limited additional diagnostic value of postcontrast in comparison with conventional MR images. Eur J Radiol. 2011; 80:331–339.
Article14. Macario S, Chassang M, Novellas S, Baudin G, Delotte J, Toullalan O, et al. The value of pelvic MRI in the diagnosis of posterior cul-de-sac obliteration in cases of deep pelvic endometriosis. AJR Am J Roentgenol. 2012; 199:1410–1415.
Article15. Chami LP, Blasbalg R, Pereira RM, Warmbrand G, Serafini PC. Findings of pelvic endometriosis at transvaginal US, MR imaging, and laparoscopy. Radiographics. 2011; 31:77–100.
Article16. Takeuchi H, Kuwatsuru R, Kitade M, Sakurai A, Kikuchi I, Shimanuki H, et al. A novel technique using magnetic resonance imaging jelly for evaluation of rectovaginal endometriosis. Fertil Steril. 2005; 83:442–447.
Article17. Kikuchi I, Kuwatsuru R, Yamazaki K, Kumakiri J, Aoki Y, Takeda S. Evaluation of the usefulness of the MRI jelly method for diagnosing complete cul-de-sac obliteration. Biomed Res Int. 2014; 2014:437962.
Article18. Loubeyre P, Copercini M, Frossard JL, Wenger JM, Petignat P. Pictorial review: rectosigmoid endometriosis on MRI with gel opacification after rectosigmoid colon cleansing. Clin Imaging. 2012; 36:295–300.
Article19. Bazot M, Bharwani N, Huchon C, Kinkel K, Cunha TM, Guerra A, et al. European society of urogenital radiology (ESUR) guidelines: MR imaging of pelvic endometriosis. Eur Radiol. 2017; 27:2765–2775.
Article20. Coutinho A Jr, Bittencourt LK, Pires CE, Junqueira F, Lima CM, Coutinho E, et al. MR imaging in deep pelvic endometriosis: a pictorial essay. Radiographics. 2011; 31:549–567.
Article21. Brown MA, Mattrey RF, Stamato S, Sirlin CB. MRI of the female pelvis using vaginal gel. AJR Am J Roentgenol. 2005; 185:1221–1227.
Article22. El Sayed RF, Alt CD, Maccioni F, Meissnitzer M, Masselli G, Manganaro L, et al. Magnetic resonance imaging of pelvic floor dysfunction - joint recommendations of the ESUR and ESGAR pelvic floor working group. Eur Radiol. 2017; 27:2067–2085.
Article23. Colaiacomo MC, Masselli G, Polettini E, Lanciotti S, Casciani E, Bertini L, et al. Dynamic MR imaging of the pelvic floor: a pictorial review. Radiographics. 2009; 29:e35.
Article24. Khatri G, Bailey AA, Bacsu C, Christie AL, Kumar N, Pedrosa I, et al. Influence of rectal gel volume on defecation during dynamic pelvic floor magnetic resonance imaging. Clin Imaging. 2015; 39:1027–1031.
Article25. Francesca M, Najwa AA, Valeria B, Fabrizio M, Marileda I, Massimo M, et al. Prospective comparison between two different magnetic resonance defecography techniques for evaluating pelvic floor disorders: air-balloon versus gel for rectal filling. Eur Radiol. 2016; 26:1783–1791.
Article26. García del Salto L, de Miguel Criado J, Aguilera del Hoyo LF, Gutiérrez Velasco L, Fraga Rivas P, Manzano Paradela M, et al. MR imaging-based assessment of the female pelvic floor. Radiographics. 2014; 34:1417–1439.
Article27. Lienemann A, Anthuber C, Baron A, Kohz P, Reiser M. Dynamic MR colpocystorectography assessing pelvic-floor descent. Eur Radiol. 1997; 7:1309–1317.
Article28. Hoeffel C, Mulé S, Laurent V, Bouché O, Volet J, Soyer P. Primary rectal cancer local staging. Diagn Interv Imaging. 2014; 95:485–494.
Article29. Loubeyre P, Petignat P, Jacob S, Egger JF, Dubuisson JB, Wenger JM. Anatomic distribution of posterior deeply infiltrating endometriosis on MRI after vaginal and rectal gel opacification. AJR Am J Roentgenol. 2009; 192:1625–1631.
Article30. Hottat N, Larrousse C, Anaf V, Noël J-C, Matos C, Absil J, et al. Endometriosis: contribution of 3.0-T pelvic MR imaging in preoperative assessment--initial results. Radiology. 2009; 253:126–134.
Article31. Balleyguier C, Sala E, Da Cunha T, Bergman A, Brkljacic B, Danza F, et al. Staging of uterine cervical cancer with MRI: guidelines of the European Society of Urogenital Radiology. Eur Radiol. 2011; 21:1102–1110.
Article32. Akata D, Kerimoglu U, Hazirolan T, Karcaaltincaba M, Köse F, Ozmen MN, et al. Efficacy of transvaginal contrast-enhanced MRI in the early staging of cervical carcinoma. Eur Radiol. 2005; 15:1727–1733.
Article33. Young P, Daniel B, Sommer G, Kim B, Herfkens R. Intravaginal gel for staging of female pelvic cancers--preliminary report of safety, distention, and gel-mucosal contrast during magnetic resonance examination. J Comput Assist Tomogr. 2012; 36:253–256.
Article34. Mondot L, Novellas S, Senni M, Piche T, Dausse F, Caramella T, et al. Pelvic prolapse: static and dynamic MRI. Abdom Imaging. 2007; 32:775–783.
Article35. Chan YY, Jayaprakasan K, Zamora J, Thornton JG, Raine-Fenning N, Coomarasamy A. The prevalence of congenital uterine anomalies in unselected and high-risk populations: a systematic review. Hum Reprod Update. 2011; 17:761–771.
Article36. Troiano RN, McCarthy SM. Mullerian duct anomalies: imaging and clinical issues. Radiology. 2004; 233:19–34.37. Griffin N, Grant LA, Sala E. Magnetic resonance imaging of vaginal and vulval pathology. Eur Radiol. 2008; 18:1269–1280.
Article38. Yoo RE, Cho JY, Kim SY, Kim SH. A systematic approach to the magnetic resonance imaging-based differential diagnosis of congenital Müllerian duct anomalies and their mimics. Abdom Imaging. 2015; 40:192–206.
Article39. Beets-Tan RG, Lambregts DM, Maas M, Bipat S, Barbaro B, Caseiro-Alves F, et al. Magnetic resonance imaging for the clinical management of rectal cancer patients: recommendations from the 2012 European Society of Gastrointestinal and Abdominal Radiology (ESGAR) consensus meeting. Eur Radiol. 2013; 23:2522–2531.
Article40. Slater A, Halligan S, Taylor SA, Marshall M. Distance between the rectal wall and mesorectal fascia measured by MRI: effect of rectal distension and implications for preoperative prediction of a tumour-free circumferential resection margin. Clin Radiol. 2006; 61:65–70.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Preoperative Evaluation of Lower Rectal Cancer by Pelvic MR with and without Gel Filling
- Interpretation of Rectal MRI after Neoadjuvant Treatment in Patients with Rectal Cancer
- Clinical Implication of Lateral Pelvic Lymph Node Metastasis in Rectal Cancer Treated with Neoadjuvant Chemoradiotherapy
- The efficacy of MRI to diagnosis the bladder and rectal invasion in cervical cancer
- Rectal Injury Associated with Pelvic Fracture