Investig Clin Urol.
2018 May;59(3):177-181. 10.4111/icu.2018.59.3.177.
Utilization of cryopreserved sperm cells based on the indication for storage
- Affiliations
-
- 1Division of Urology, Department of Surgery, Scott & White Medical Center and Texas A&M Health Science Center College of Medicine, Temple, Texas, USA. Graham.Machen@BSWHealth.org
- 2Department of Pathology, Scott & White Medical Center and Texas A&M Health Science Center College of Medicine, Temple, Texas, USA.
- 3Department of Obstetrics and Gynecology, Scott & White Medical Center and Texas A&M Health Science Center College of Medicine, Temple, Texas, USA.
- KMID: 2410590
- DOI: http://doi.org/10.4111/icu.2018.59.3.177
Abstract
- PURPOSE
Cryopreservation of sperm from human semen has been available since the 1950s. The actual utilization of available cryopreservation technology has been infrequently reported. We set out to examine the utilization and outcomes of cryopreserved sperm cells based on the indication for storage.
MATERIALS AND METHODS
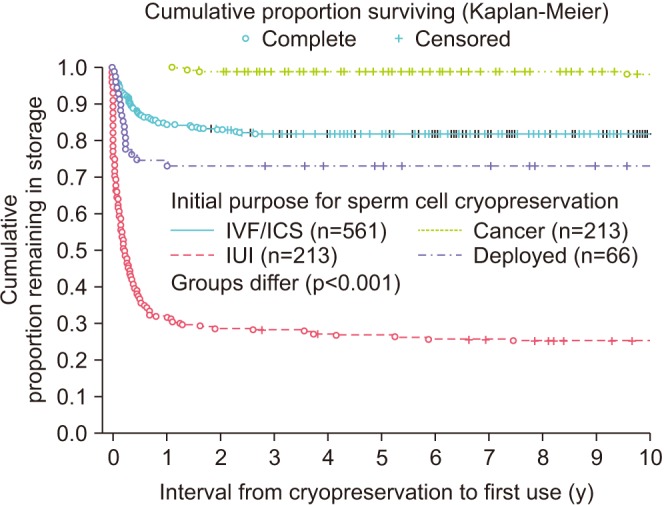
A dataset was developed from retrospective review. The purposes for cryopreservation, eventual utilization, and outcomes of use for insemination were recorded. The types of utilization were accumulated as proportions for different purposes. The timing for use of samples for insemination procedures was evaluated using survival statistics. The frequency of patients arranging to destroy samples was also reported.
RESULTS
From September 1988 through March 2015, 1442 samples were cryopreserved. Samples were cryopreserved for four primary purposes: infertility treatments focused on intrauterine insemination (IUI) or in vitro fertilization/intracellular injection (IVF/ICSI), for fertility preservation related to cancer treatment, or prior to military deployment. Total utilization rates were 19.3%. Samples cryopreserved for IUI were more likely to be used (64.3%), while samples cryopreserved as backup for IVF/ICSI were more likely to be destroyed (29.8%). Pregnancy rates varied based on the indication and ART used. Pregnancies per cycle were 35% for IVF/ICSI and were 10% for IUI.
CONCLUSIONS
Cryopreservation of sperm is a valuable and underutilized resource, particularly amongst male cancer patients. This technology can facilitate infertility treatments based on a variety of indications, including deployment"”a patient cohort unique to our dataset.
Keyword
MeSH Terms
Figure
Reference
-
1. Bunge RG, Sherman JK. Fertilizing capacity of frozen human spermatozoa. Nature. 1953; 172:767–768.
Article2. Agarwal A, Tolentino MV Jr, Sidhu RS, Ayzman I, Lee JC, Thomas AJ Jr, et al. Effect of cryopreservation on semen quality in patients with testicular cancer. Urology. 1995; 46:382–389. PMID: 7660514.
Article3. Brezina PR, Kutteh WH, Bailey AP, Ding J, Ke RW, Klosky JL. Fertility preservation in the age of assisted reproductive technologies. Obstet Gynecol Clin North Am. 2015; 42:39–54. PMID: 25681839.
Article4. Kelleher S, Wishart SM, Liu PY, Turner L, Di Pierro I, Conway AJ, et al. Long-term outcomes of elective human sperm cryostorage. Hum Reprod. 2001; 16:2632–2639. PMID: 11726587.
Article5. Saito K, Suzuki K, Iwasaki A, Yumura Y, Kubota Y. Sperm cryopreservation before cancer chemotherapy helps in the emotional battle against cancer. Cancer. 2005; 104:521–524. PMID: 15968690.
Article6. Pacey A, Merrick H, Arden-Close E, Morris K, Rowe R, Stark D, et al. Implications of sperm banking for health-related quality of life up to 1 year after cancer diagnosis. Br J Cancer. 2013; 108:1004–1011. PMID: 23470465.
Article7. Girasole CR, Cookson MS, Smith JA Jr, Ivey BS, Roth BJ, Chang SS. Sperm banking: use and outcomes in patients treated for testicular cancer. BJU Int. 2007; 99:33–36. PMID: 17034492.
Article8. Schover LR, Brey K, Lichtin A, Lipshultz LI, Jeha S. Oncologists' attitudes and practices regarding banking sperm before cancer treatment. J Clin Oncol. 2002; 20:1890–1897. PMID: 11919249.
Article9. Sheth KR, Sharma V, Helfand BT, Cashy J, Smith K, Hedges JC, et al. Improved fertility preservation care for male patients with cancer after establishment of formalized oncofertility program. J Urol. 2012; 187:979–986. PMID: 22264454.
Article10. Johnson MD, Cooper AR, Jungheim ES, Lanzendorf SE, Odem RR, Ratts VS. Sperm banking for fertility preservation: a 20-year experience. Eur J Obstet Gynecol Reprod Biol. 2013; 170:177–182. PMID: 23870186.
Article11. Chung K, Irani J, Knee G, Efymow B, Blasco L, Patrizio P. Sperm cryopreservation for male patients with cancer: an epidemiological analysis at the University of Pennsylvania. Eur J Obstet Gynecol Reprod Biol. 2004; 113(Suppl 1):S7–S11. PMID: 15041122.
Article12. Magelssen H, Haugen TB, von Düring V, Melve KK, Sandstad B, Fosså SD. Twenty years experience with semen cryopreservation in testicular cancer patients: who needs it? Eur Urol. 2005; 48:779–785. PMID: 15963629.
Article13. Ping P, Gu BH, Li P, Huang YR, Li Z. Fertility outcome of patients with testicular tumor: before and after treatment. Asian J Androl. 2014; 16:107–111. PMID: 24369141.
Article14. Menon S, Rives N, Mousset-Siméon N, Sibert L, Vannier JP, Mazurier S, et al. Fertility preservation in adolescent males: experience over 22 years at Rouen University Hospital. Hum Reprod. 2009; 24:37–44. PMID: 18945713.
Article15. Cressman BE, Pace-Owens S, Pliego JF, Wincek TJ, Kuehl TJ. Effect of sperm dose on pregnancy rate from intrauterine insemination: a retrospective analysis. Tex Med. 1996; 92:74–79. PMID: 8979764.16. Anger JT, Gilbert BR, Goldstein M. Cryopreservation of sperm: indications, methods and results. J Urol. 2003; 170:1079–1084. PMID: 14501696.
Article17. Ferrari S, Paffoni A, Filippi F, Busnelli A, Vegetti W, Somigliana E. Sperm cryopreservation and reproductive outcome in male cancer patients: a systematic review. Reprod Biomed Online. 2016; 33:29–38. PMID: 27156003.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Establishment of Sperm Penetration Assay Using Cryopreserved Hamster Oocyte
- A Case of Pregnancy from Cryopreserved Embryos following ICSI with Frozen-Thawed Epididymal Sperms
- The Need for Sperm Cryopreservation at the Time of Vasovasostomy or Vasoepididymostomy
- Potential use of ashwagandha extract in storage of liquid boar semen
- Comparison of ICSI Outcomes between Fresh and Cryopreserved-Thawed Testicular Spermatozoa