J Korean Soc Echocardiogr.
1994 Dec;2(2):129-135. 10.4250/jkse.1994.2.2.129.
The Effects of Late Angioplasty of Infarct Related Artery on Left Ventricular Remodeling in Acute Myocardial Infarction
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Kyung Hee University, Seoul, Korea.
- KMID: 2410440
- DOI: http://doi.org/10.4250/jkse.1994.2.2.129
Abstract
- BACKGROUND
Acute early reperfusion of infarct-related artery was most important predictor of survival in patients with acute myocardial infarcton(AMI). But, it is well accepted that the degree of left ventricular dilatation after an acute myocardial infarction is an important predictor of death at 1 year. The severity of residual stenosis of the infarct-related artery(IRA) was an impartant predictor of subsequent left ventricular remodeling after myocardial infarction. We evaluated the effect of late PTCA of an residual stenotic lesion of IRA on left ventricular dilatation and function.
SUBJECTS AND METHODS
Twenty six patients with first acute anterior wall myocardial infarction were evaluated. All patients recieved immediate thrombolytic therapy(within 6hrs after AMI) and coronary angiogram(mean 1.8 days after onset). PTCA was performed successfully in eleven patients(mean 6.8 days after onset). LV volume and EF was measured by echocardiography at discharge and follow-up(mean 5.8 months after AMI onset).
RESULTS
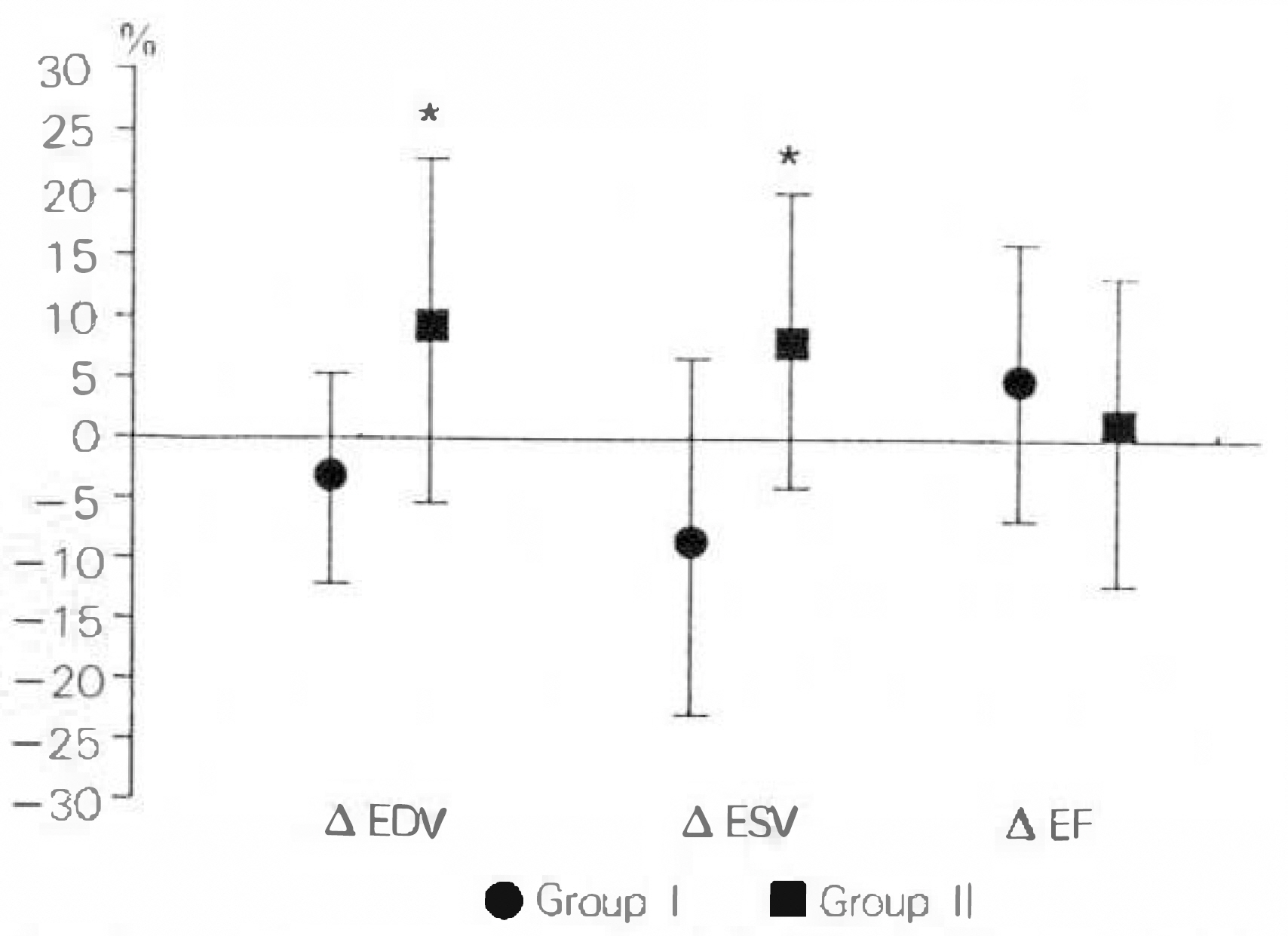
1) After thrombolytic therapy, degree of residual stenotic lesion of IRA was 78.9% in Group I and 75.7% in Group II. After PTCA, degree of residual stenosis was 25.5% in group I, 2) In the patients with treated by early thrombolysis with late PTCA(Group I), EDV change was from 85.7±13.4ml at discharge to 82.8±16.4ml at follow up, ESV change was 43.1±12.4ml to 39.5±15.4ml, EF change was 50.0±6.4% to 53.2±8.5%, and percent change in EDV, ESV and EF were −3.5±9.0%, −8.7±16.1% and 5.9±12.3%, respectively. 3) In the patients with thrombolysis alone(Group II), EDV change was from 79.1±16.4ml at discharge to 86.2±21.5ml at follow up, ESV change was 42.0±12.8ml to 46.1±18.4ml, EF change was 47.2±8.7% to 47.1±9.5%, and percent change in EDV, ESV and EF were 9.1±14.7%, 8.8±12.1% and 0.0±13.1%, respectively. 4) In Group I patients, significant lower percent change in EDV and ESV than group II patients(p=0.01).
CONCLUSION
Late mechanical reperfusion with PTCA of residual significant stenosis of infarct-related artery tend to reduce subsequent left ventricular dilatation.
MeSH Terms
Figure
Reference
-
References
1). Serruys PW, Simoons ML, Suryapranata H, Vermeer F, Wijns W, van den Brand M, Bar F, Zwaan C, Krauss XH, Remme WJ, Res J, Verheugt FWA, van Domberg R, Lubsen J, Hugenholtz PG. Preservation of global and regional left ventricular function after early thrombolysis in acute myocardial infarction. J Am Coll Cardiol. 7:729–742. 1986.
Article2). Gruppo Italiano per lo Studio della Streptochinasi nell'Infarcto miocardico(GISSI). Effectiveness of intravenous thrombolytic treatment in acute myocardial infarction. Lancet. 8478:397–401. 1986.3). Thompson PL, Aylward P, Federman J, Harris P, Hodge R, Latt N, Pitt A, Thompson A, Tonkin A. Coronary thrombolysis and myocardial salvage by tissue plasminogen activator given up to 4 hours after onset of myocardial infarction. National Heart Foundation of Australia Coronary Thrombolysis Group. Lancet. 8579:203–207. 1988.4). Second International Study of Infarct Survival Collaboratory Group. Randomized trial of intravenous streptokinase, oral aspirin, both, or neither among 17,187 cases of suspected myocardial infarction: ISIS-2. Lancet. 8607:349–360. 1988.5). Koshal A, Beanlands DS, Davies RA, Nair RC, Keon WJ. Urgent surgical reperfusion in acute evolving myocardial infarction. A randomized controlled study. Circulation. 78(suppl I):I–171-I-178. 1988.6). Kander NH, O'Neill WW, Topol EJ, Gallison L, Mileski R, Ellis SG. Long-term follow-up of patients treated with coronary angioplasty for acute myocardial infarction. Am Heart J. 118:228–233. 1989.
Article7). Sui CS, Nidorf SM, Galambos GS, Weyman AE, Picard MH. The effect of late patency of the infarct-relaled coronary artery on left ventricular morphology and regional function after thrombolysis. Am Heart J. 124:265–272. 1992.8). Tiefenbrunn AJ. Clinical benefits of thrombolytic therapy in acute myocardial infarction. Am J Cardiol. 69:3A–11A. 1992.
Article9). Hutchins GM, Bulkley BH. Infant expansion versus extension: two different complications of acute myocardial infarction. Am J Cardiol. 41:1127–1132. 1978.10). Weisman HF, Healy B. Myocardial infarct expansion, infarct extension, and reinfarction: physiologic concepts. Prog Cardiovasc Dis. 30:73–110. 1987.11). Pfeffer MA, Braunwald E. Ventricular remodeling after myocardial infarction: experimental observations and clinical implications. Circulation. 81:1161–1172. 1990.
Article12). Whittaker P, Boughner DR, Kloner RA. Role of collagen in acute myocardial infarct expansion. Circulation. 84:2123–2134. 1991.
Article13). Eaton LW, Weiss JL, Bulkley BH, Garrison JB, Weisfeldt ML. Regional cardiac dilatation after acute myocardial infarction: recognition by two dimentional echocardiography. N Engl J Med. 300:57–62. 1979.14). Gaudron P, Eillies C, Kugler I, Ertl G. Progressive left ventricular dysfunction and remodeling after myocardial infarction. Circulation. 87:755–763. 1993.
Article15). McKay RG, Pfeffer MA, Pasternak RC, et al. Left ventricular remodeling after myocardial infarction: a corollary to infarct expansion. Circulation. 74:693–702. 1986.
Article16). White HD, Norris RM, Brown MA, Brandt PWT, Whitlock RML, Wild CJ. Left ventricular end-systolic volume as the major determinant of survival after recovery from myocardial infarction. Circulation. 76:44–51. 1987.
Article17). Pfeffer JM, Pfeffer MA, Bwaunwald E. Influence of chronic captopril therapy on the infarcted left ventricle of the rat. Circ Res. 57:84–95. 1985.
Article18). Pfeffer MA, Lamas GA, Vaughan DE, Parisi AF, Braunwald E. Effect of captopril on progressive ventricular dilatation after anterior myocardial infarction. N Eng J Med. 319:80–86. 1988.
Article19). Sweet CS. Eminent SE, Stabillito II, Riberio LGT: Increased survival in rats with congestive heart failure treated with enalapril. J Cardiovasc Pharmacol. 10:636–642. 1987.20). Pfeffer MA, Pfeffer JM, Steinberg C, Finn P. Survival after an experimental myocardial infarction: benefitial effects of long term therapy with captopril. Circulation. 72:406–412. 1985.21). Jugdutt BI, Schwarz-Michorowski BL, Khan MI. Effect of long-term captopril therapy on left ventricular remodeling and function during healing of canine myocardial infarction. J Am Coll Cardiol. 19:713–721. 1992.
Article22). Jugdutt BI, Warnica JW. Intravenous nitroglycerin therapy to limit myocardial infarct size, expansion, and complications: effect of timing, dosage and infarct location. Circulation. 78:906–919. 1988.
Article23). Leung W-H, Lau C-P. Effect of severity of residual stenosis of the infarct-related coronary artery on left ventricular dilatation and function after acute myocardial infarction. J Am Coll Cardiol. 20:307–313. 1992.24). Kloner Robert A. Coronary Angioplasty: A Treatment Option for Left Ventricular Remodeling After Myocardial Infarction ? J Am Coll Cardol. 20(2):314–316. 1992.25). Brodie Bruce R, Stuckey Thomas D, Charles Hansen, Denise Muncy, Weintraub Richard A, Le-Bauer E Joseph, Kelly Thomas A, Katz Jeffrey D, Berry Jonathan J. Benefit of late Coronary Reperfusion in patients with Acute Myocardial Infarction and Persistent Ischemic Chest Pain. Am J Cardiol. 74:538–543. 1994.
Article26). Vladimir Dzavik, Beanlands Donald S, Davies Richard F, Danielle Leddy, Jean-Francois Marquis, Teo Koon K, Ruddy Terrence D, Burton Jeffrey R, Humen Dennis P. Effects of Late Percutaneous Transluminal Coronary Angioplasty of an Occluded Infarct-Related Coronary Artery on Left Ventricular Function in Patients with a Recent(<6 Weeks) Q-Wave Acute Myocardial Infarction (Total Occlusion Post-Myocardial Infarction Intervension Study [TOMIS]–A Pilot Study). Am J Cardiol. 73:856–861. 1994.27). Zijlstra F, de Boer MJ, Hoorntje JGA, Reiffers S, Reiber JHC, Suryapranata H. A comparison of immediate coronary angioplasty with intravenous streptokinase in acute myocardial infarction. N Engl J Med. 328:680–684. 1993.
Article28). Grines CL, Browne KF, Marco J, Rothbaum D, Stone GW, O'Keefe J, Overlie P, Donohue B, Chelliah N, Timmis GC, Vliestra RE, Strzelecki M, Puchrowicz-Ochoski S, O'Neil WW. A comparison of immediate angioplasty with thrombolytic therapy for acute myocardial infarction. N Engl J Med. 328:673–679. 1993.
Article29). Piero Zardini, Paolo Marino, Giorgio Golia, Maurizio Anselmi, Massimo Castelli. Ventricular Remodeling and Infarct Expansion. Am J Cardiol. 72:98G–106G. 1993.30). Hochmann JS, Choo H. Limitation of myocardial infarct expansion by reperfusion independent of myocardial salvage. Circulation. 75:299–306. 1987.
Article31). Hale SL, Kloner RA. Left ventricular topographic alterations in the completely healed rat infarct caused by early and late coronary artery reperfusion. Am Heart J. 116:1508–1513. 1988.
Article32). Califf RM, Topol EJ, Gersh BJ. From myocardial salvage to patient salvage in acute myocardial infarction: the role of reperfusion therapy. J Am Coll Cardiol. 14:1382–1388. 1989.
Article33). Topol EJ, Califf RM, George BS, Kereiakes DJ, Abbottsmith CW, Candela RJ, LEE KJ, Pitt B, Stack RS, O'Neil WW and the Throbolysis and Angioplasty in Myocardial Infarction(TAMI) Study Group. A multicenter randomized trial of intravenous recombinant tissue plasminogen activator and immediate angioplasty in acute myocardial infarction. N Eng J Med. 371:581–588. 1987.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Open Artery Hypothesis
- Relation Between Residual Stenosis of Infarct-related Artery and Left Ventricular Dilatation After Acute Myocardial Infarction
- Effects of Spontaneous Recanalization of Left Ventricular Function after Acute Myocardial Infarction
- The Effects of Abciximab on Left Ventricular Remodeling in Patient with Acute Myocardial Infarction Treated with Primary Percutaneous Coronary Intervention
- The Effects of Carvedilol on Ventricular Remodeling after Myocardial Infarction in Rats