J Dent Anesth Pain Med.
2018 Apr;18(2):89-95. 10.17245/jdapm.2018.18.2.89.
Structural damage to periodontal tissues at varying rate of anesthetic injection
- Affiliations
-
- 1Medical firm Vital EBB, Ekaterinburg, Russia.
- 2Institute of Immunology and Physiology of the Ural Branch of the RAS, Ekaterinburg, Russia. a.sarapultsev@gmail.com
- 3Federal State Autonomous Educational Institution of Higher Professional Education, Ural Federal University named after the first President of Russia B. N. Yeltsin, Ekaterinburg, Russia.
- KMID: 2410141
- DOI: http://doi.org/10.17245/jdapm.2018.18.2.89
Abstract
- BACKGROUND
Incorrect administration of an anesthetic during local anesthesia is one of the most important causes of pain symptoms in patients scheduled for dental procedures. The current study assessed the severity of damage to periodontal tissue following different rates of anesthetic administration.
METHODS
The research was conducted on 50 outbred male rats with a body mass of 180-240 g. The anesthetic used was 1% articaine.
RESULTS
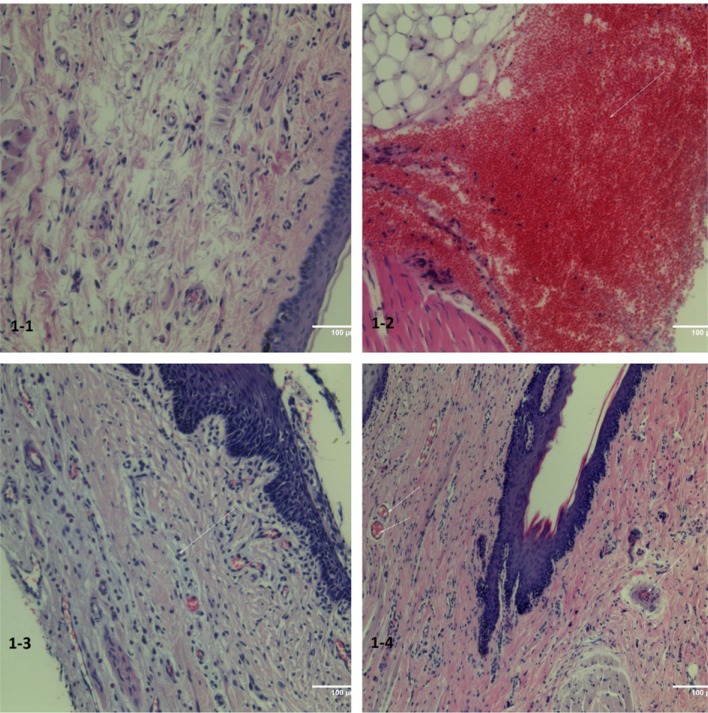
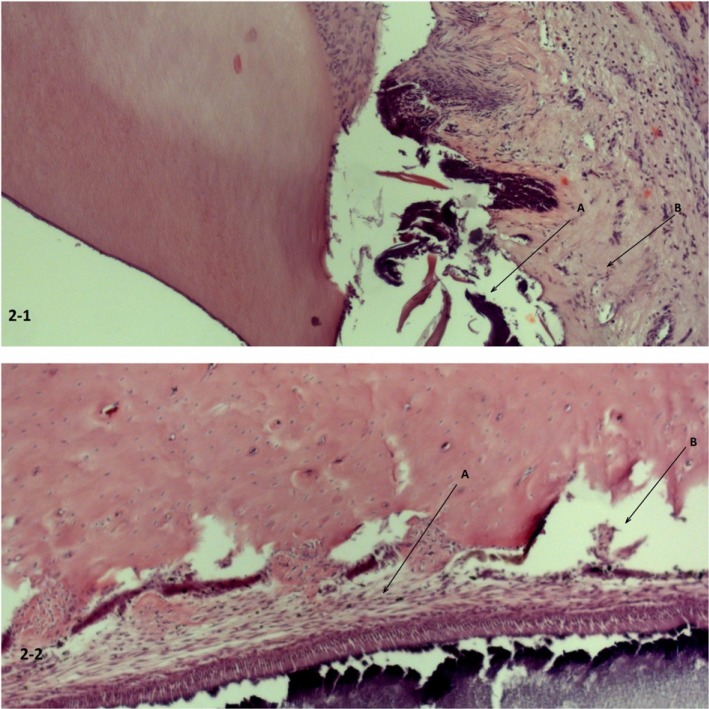
The results showed that administration of the anesthetic at a rapid pace caused structural damage to the periodontal tissue. Further, signs of impaired microcirculation were noted at all rates of administration. Biochemical studies demonstrated changes in the level of glucose and enzymes with the rapid introduction of the anesthetic, indicating severe systemic stress response of the body.
CONCLUSIONS
Injection of local anesthetic at any rate of introduction induces vascular congestion in the microcirculatory bloodstream and exudative reactions. Rapid introduction of an anesthetic causes progression of structural changes in the gingival tissue.
MeSH Terms
Figure
Reference
-
1. Milgrom P, Coldwell SE, Getz T, Weinstein P, Ramsay DS. Four dimensions of fear of dental injections. J Am Dent Assoc. 1997; 128:756–762. PMID: 9188235.
Article2. Abrahamsson KH, Berggren U, Hallberg L, Carlsson SG. Dental phobic patients' view of dental anxiety and experiences in dental care: a qualitative study. Scand J Caring Sci. 2002; 16:188–196. PMID: 12000673.
Article3. Weinstein P, Shimono T, Domoto P, Wohlers K, Matsumura S, Ohmura M, et al. Dental fear in Japan: Okayama Prefecture school study of adolescents and adults. Anesth Prog. 1992; 39:215–220. PMID: 8250343.4. Tzafalia M, Sixou JL. Administration of anesthetic solutions using a metal syringes. An ex vivo study. Anesth Prog. 2011; 58:61–65. PMID: 21679041.5. Saijo M, Ito E, Ichinohe T, Kaneko Y. Lack of pain reduction by a vibrating local anesthetic attachment: a pilot study. Anesth Prog. 2005; 52:62–64. PMID: 16048153.
Article6. Jacobs S, Haas DA, Meechan JG, May S. Injection pain: comparison of the three mandibular block techniques and modulation by nitrous oxide. J Am Dent Assoc. 2003; 134:869–876. PMID: 12892444.7. Flanagan T, Wahl MJ, Schmitt MM, Wahl JA. Size doesn't matter: needle gauge and injection pain. Gen Dent. 2007; 55:216–217. PMID: 17511363.8. Meechan JG, Howlett PC, Smith BD. Factors influencing the discomfort of intraoral needle penetration. Anesth Prog. 2005; 52:91–94. PMID: 16252738.
Article9. Nakanishi O, Haas D, Ishikawa T, Kameyama S, Nishi M. Efficacy of mandibular topical anesthesia varies with the site of administration. Anesth Prog. 1996; 43:14–19. PMID: 10323120.10. Kaufman E, Epstein JB, Naveh E, Gorsky M, Gross A, Cohen G. A survey of pain, pressure, and discomfort induced by commonly used oral local anesthesia injections. Anesth Prog. 2005; 52:122–127. PMID: 16596910.
Article11. Meechan JG. Pain control in local analgesia. Eur Arch Paediatr Dent. 2009; 10:71–76. PMID: 19627670.
Article12. Primosch RE, Brooks R. Influence of anesthetic flow rate delivered by the Wand Local Anesthetic System on pain response to palatal injections. Am J Dent. 2002; 15:15–20. PMID: 12074223.13. Kudo M. Initial injection pressure for dental local anesthesia: effects on pain and anxiety. Anesth Prog. 2005; 52:95–101. PMID: 16252739.
Article14. Pashley EL, Nelson R, Pashley DH. Pressures created by dental injections. J Dent Res. 1981; 60:1742–1748. PMID: 6944338.
Article15. Sumer M, Misir F, Koyuturk AE. Comparison of the Wand with a conventional technique. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006; 101:e106–e109. PMID: 16731373.
Article16. Versloot J, Veerkamp JS, Hoogstraten J. Computerized anesthesia delivery system vs. traditional syringe: comparing pain and pain-related behavior in children. Eur J Oral Sci. 2005; 113:488–493. PMID: 16324138.
Article17. Meechan JG. Differences between men and women regarding attitudes toward dental local anesthesia among junior students at a United Kingdom dental school. Anesth Prog. 2005; 52:50–55. PMID: 16048151.
Article18. Rankin JA, Harris MB. Comparison of stress and coping in male and female dentists. J Dent Pract Adm. 1990; 7:166–172. PMID: 2084220.19. Hochman MN, Friedman MJ, Williams W, Hochman CB. Interstitial tissue pressure associated with dental injections: a clinical study. Quintessence Int. 2006; 37:469–476. PMID: 16752703.20. Walmsley AD, Lloyd JM, Harrington E. Pressures produced in vitro during intraligamentary anaesthesia. Br Dent J. 1989; 167:341–344. PMID: 2590570.
Article21. Clark JD, Gebhart GF, Gonder JC, Keeling ME, Kohn DF. The 1996 Guide for the care and use of laboratory animals. ILAR J. 1997; 38:41–48. PMID: 11528046.
Article22. Flecknell PA. Laboratory animal anesthesia. London: Academic Press;1987.23. Swindle MM, Adams RJ. Experimental surgery and physiology: induced animal models of human disease. Baltimore: Williams & Wilkins;1988.24. Baart JA, Brand HS. Microprocessor-Aided Local Anaesthesia. Local Anaesthesia in Dentistry. 2Ed. Springer International Publishing;2017. p. 113–123.25. Lillie RD. HJ Conn's Biological Stains. 4th ed. Baltimore: Williams and Wilkins;1977.26. Bancroft JD, Stevens A. Theory and Practice of Histological Techniques. 4th ed. New York: Churchill Livingstone;1996.27. Pratt DS, Kaplan MM. Evaluation of abnormal liver enzyme results in asymptomatic patients. N Engl J Med. 2000; 342:1266–1271. PMID: 10781624.28. De Ritis F, Coltorti M, Giusti G. An enzymic test for the diagnosis of viral hepatitis: the transaminase serum activities. 1957. Clin Chim Acta. 2006; 369:148–152. PMID: 16781697.29. Selye H. Stress in health and disease. Boston: Butterworths;1976.30. Cioffi GA, Chernow B, Glahn RP, Terezhalmy GT, Lake CR. The hemodynamic and plasma catecholamine responses to routine restorative dental care. J Am Dent Assoc. 1985; 111:67–70. PMID: 3861687.
Article31. Jastak JT, Yagiela JA. Vasoconstrictors and local anesthesia: a review and rationale for use. J Am Dent Assoc. 1983; 107:623–630. PMID: 6355236.
Article32. American Gastroenterological Association. American Gastroenterological Association medical position statement: evaluation of liver chemistry tests. Gastroenterology. 2002; 123:1364–1366. PMID: 12360497.33. Selye H. The story of the adaptation syndrome. Am J Med Sci. 1952; 224:711.
Article34. Grizuk SF. Oral and Maxillofacial Surgery. Moscow: Geotar-Media;2010. [In Russian].35. Sisk AL. Vasoconstrictors in local anesthesia for dentistry. Anesth Prog. 1992; 39:187–193. PMID: 8250339.36. Ibragimov ZI, Semkin VA, Didikin SS, Titova GP. Features of the morphological changes of skeletal muscles after intramuscular administration of anesthetics. Alfavit stomatologii. 2007; 1:42–44. [In Russian].37. Zoryan EV, Rabinovich SA. Vasoconstrictive agents in composition of local anesthetics: significance and problems. Clin Dent. 2006; 3:24–28. [In Russian].38. Rabinovich SA, Kuznetzov GI, Moscowez ON, Zoryan EV. Int Dent Rev. 2008; 1:14–15. [In Russian].
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effectiveness of anterior middle superior alveolar injection using a computer-controlled local anesthetic delivery system for maxillary periodontal flap surgery
- Comparison of pain intensity of anterior middle superior alveolar injection with infiltration anesthetic technique in maxillary periodontal surgery
- Biological Characteristics of Human Periodontal Ligament Cells
- Waiting for innovations in periodontal disease diagnosis
- Reply on "Relationship between maternal periodontal disease and Apgar score of newborns"