Ann Hepatobiliary Pancreat Surg.
2018 Feb;22(1):52-57. 10.14701/ahbps.2018.22.1.52.
Clinical patterns of postcholecystectomy syndrome
- Affiliations
-
- 1King Abdullah International Medical Research Center/King Saud bin Abdulaziz University for Health Sciences, Jeddah, Saudi Arabia. shirah007@ksau-hs.edu.sa
- 2Department of General Surgery, Al Ansar General Hospital, Medina, Saudi Arabia.
- 3Department of Medicine, Al Ansar General Hospital, Medina, Saudi Arabia.
- 4King Abdulaziz Medical City/King Saud bin Abdulaziz University for Health Sciences, Jeddah, Saudi Arabia.
- KMID: 2409080
- DOI: http://doi.org/10.14701/ahbps.2018.22.1.52
Abstract
- BACKGROUNDS/AIMS
Postcholecystectomy syndrome represents a heterogeneous group of symptoms and findings in patients who have previously undergone cholecystectomy. It is rare and under-reported in Saudi Arabia. It can be attributed to many complications such as bile duct injury, biliary leak, retained common bile duct stones, recurrent bile duct stones, and bile duct strictures. In this study, we aimed to analyze the causes and evaluate the approach to postcholecystectomy syndrome in our local Saudi Arabian community because of the vast number of cases encountered in our hospital for gallbladder clinical conditions and its related complications.
METHODS
A prospective cohort database analysis of 272 patients who were diagnosed and treated for postcholecystectomy syndrome between January 2000 and December 2013 were reviewed.
RESULTS
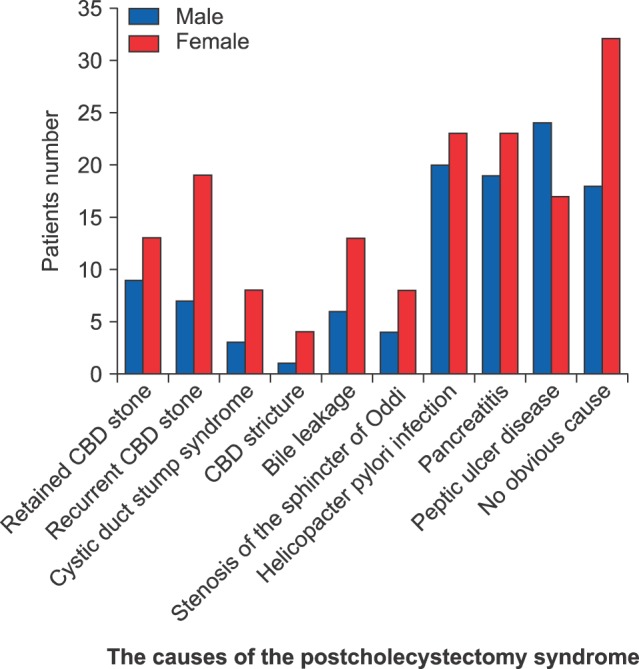
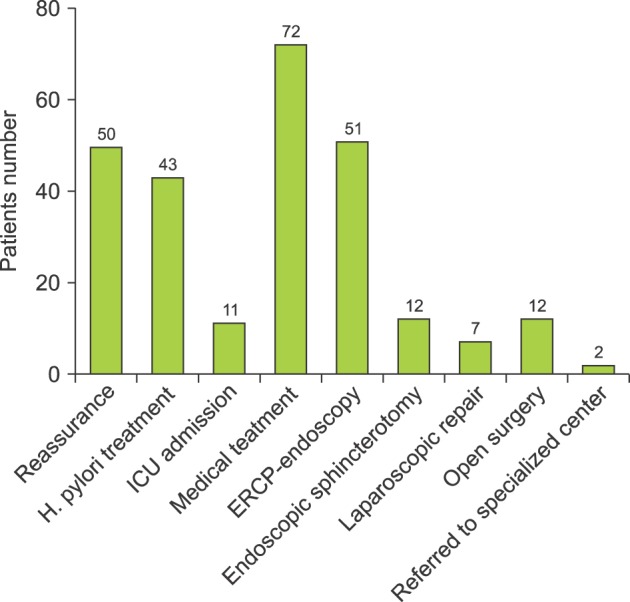
The incidence rate of postcholecystectomy syndrome was 19.8%. The male to female ratio was 1:1.45. The mean age was 37.41±7.12 years. The most common causes were as follows: No obvious cause in 50 (18.4%) patients, Helicobacter pylori infection in 43 (15.8%), pancreatitis in 42 (15.4%), peptic ulcer disease in 41 (15.1%), recurrent common bile duct (CBD) stone in 26 (9.6%), retained CBD stone in 22 (8.1%), bile leakage in 19 (7%), stenosis of the sphincter of Oddi in 12 (4.4%), cystic duct stump syndrome in 11 (4%), and CBD Stricture in 5 (1.8%). The mortality rate was 0%.
CONCLUSIONS
Any clinical presentation of postcholecystectomy should not be underestimated and be thoroughly investigated. Multidisciplinary collaboration is crucial for the best outcome and a safe approach for all the patients.
Keyword
MeSH Terms
-
Bile
Bile Ducts
Cholecystectomy
Cholecystectomy, Laparoscopic
Cohort Studies
Common Bile Duct
Constriction, Pathologic
Cooperative Behavior
Cystic Duct
Female
Gallbladder
Gallstones
Helicobacter pylori
Humans
Incidence
Jaundice
Male
Mortality
Pancreatitis
Peptic Ulcer
Postcholecystectomy Syndrome*
Prospective Studies
Saudi Arabia
Sphincter of Oddi
Figure
Cited by 1 articles
-
담낭 신생물성 용종 예측을 위한 현행 수술 적응증과 수술 전 영상의 역할
Ik Hyun Jo, Chang Nyol Paik, Hong Geun Ahn, Dong Do You, Jae Hyun Han, Hyun A Kim
Korean J Gastroenterol. 2025;85(1):52-63. doi: 10.4166/kjg.2024.130.
Reference
-
1. Schofer JM. Biliary causes of postcholecystectomy syndrome. J Emerg Med. 2010; 39:406–410. PMID: 18722735.
Article2. Jaunoo SS, Mohandas S, Almond LM. Postcholecystectomy syndrome (PCS). Int J Surg. 2010; 8:15–17. PMID: 19857610.
Article3. Redwan AA. Multidisciplinary approaches for management of postcholecystectomy problems (surgery, endoscopy, and percutaneous approaches). Surg Laparosc Endosc Percutan Tech. 2009; 19:459–469. PMID: 20027088.
Article4. Madacsy L, Dubravcsik Z, Szepes A. Postcholecystectomy syndrome: from pathophysiology to differential diagnosis - a critical review. Pancreat Disord Ther. 2015; 5:162.
Article5. Girometti R, Brondani G, Cereser L, Como G, Del Pin M, Bazzocchi M, et al. Post-cholecystectomy syndrome: spectrum of biliary findings at magnetic resonance cholangiopancreatography. Br J Radiol. 2010; 83:351–361. PMID: 20335441.
Article6. Terhaar OA, Abbas S, Thornton FJ, Duke D, O'Kelly P, Abdullah K, et al. Imaging patients with “post-cholecystectomy syndrome”: an algorithmic approach. Clin Radiol. 2005; 60:78–84. PMID: 15642297.
Article7. Wani NA, Khan NA, Shah AI, Khan AQ. Post-cholecystectomy Mirizzi's syndrome: magnetic resonance cholangiopancreatography demonstration. Saudi J Gastroenterol. 2010; 16:295–298. PMID: 20871198.
Article8. Coté GA, Ansstas M, Shah S, Keswani RN, Alkade S, Jonnalagadda SS, et al. Findings at endoscopic retrograde cholangiopancreatography after endoscopic treatment of postcholecystectomy bile leaks. Surg Endosc. 2010; 24:1752–1756. PMID: 20041266.
Article9. Pinkas H, Brady PG. Biliary leaks after laparoscopic cholecystectomy: time to stent or time to drain. Hepatobiliary Pancreat Dis Int. 2008; 7:628–632. PMID: 19073409.10. Topazian M, Hong-Curtis J, Li J, Wells C. Improved predictors of outcome in postcholecystectomy pain. J Clin Gastroenterol. 2004; 38:692–696. PMID: 15319654.
Article11. Walsh RM, Ponsky JL, Dumot J. Retained gallbladder/cystic duct remnant calculi as a cause of postcholecystectomy pain. Surg Endosc. 2002; 16:981–984. PMID: 12163968.
Article12. Sakai Y, Tsuyuguchi T, Ishihara T, Sugiyama H, Miyakawa K, Yukisawa S, et al. The usefulness of endoscopic transpapillary procedure in post-cholecystectomy bile duct stricture and post-cholecystectomy bile leakage. Hepatogastroenterology. 2009; 56:978–983. PMID: 19760924.13. Berger H, Weinzierl M, Neville ES, Pratschke E. Percutaneous transcatheter occlusion of cystic duct stump in postcholecystectomy bile leakage. Gastrointest Radiol. 1989; 14:334–336. PMID: 2806820.
Article14. Shaw C, O'Hanlon DM, Fenlon HM, McEntee GP. Cystic duct remnant and the ‘post-cholecystectomy syndrome’. Hepatogastroenterology. 2004; 51:36–38. PMID: 15011827.15. Lum YW, House MG, Hayanga AJ, Schweitzer M. Postcholecystectomy syndrome in the laparoscopic era. J Laparoendosc Adv Surg Tech A. 2006; 16:482–485. PMID: 17004873.
Article16. Zhou PH, Liu FL, Yao LQ, Qin XY. Endoscopic diagnosis and treatment of post-cholecystectomy syndrome. Hepatobiliary Pancreat Dis Int. 2003; 2:117–120. PMID: 14607662.17. Kalaitzakis E, Ambrose T, Phillips-Hughes J, Collier J, Chapman RW. Management of patients with biliary sphincter of Oddi disorder without sphincter of Oddi manometry. BMC Gastroenterol. 2010; 10:124. PMID: 20969779.
Article18. Phillips MR, Joseph M, Dellon ES, Grimm I, Farrell TM, Rupp CC. Surgical and endoscopic management of remnant cystic duct lithiasis after cholecystectomy--a case series. J Gastrointest Surg. 2014; 18:1278–1283. PMID: 24810238.
Article19. Filip M, Saftoiu A, Popescu C, Gheonea DI, Iordache S, Sandulescu L, et al. Postcholecystectomy syndrome - an algorithmic approach. J Gastrointestin Liver Dis. 2009; 18:67–71. PMID: 19337637.20. Rogy MA, Függer R, Herbst F, Schulz F. Reoperation after cholecystectomy. The role of the cystic duct stump. HPB Surg. 1991; 4:129–134. PMID: 1931779.21. Marie MA. Seroprevalence of Helicobacter pylori infection in large series of patients in an urban area of Saudi Arabia. Korean J Gastroenterol. 2008; 52:226–229. PMID: 19077524.22. Ayoola AE, Ageely HM, Gadour MO, Pathak VP. Prevalence of Helicobacter pylori infection among patients with dyspepsia in South-Western Saudi Arabia. Saudi Med J. 2004; 25:1433–1438. PMID: 15494817.23. Khan MA, Ghazi HO. Helicobacter pylori infection in asymptomatic subjects in Makkah, Saudi Arabia. J Pak Med Assoc. 2007; 57:114–117. PMID: 17432012.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The most frequent symptoms of postcholecystectomy syndrome for cholelithiasis patients older than 40 years of age
- Successful removal of remnant cystic duct stump stone using single-operator cholangioscopy-guided electrohydraulic lithotripsy: two case reports
- Endoscopic Retrograde Cholangiopancreatography in the Evaluation of Postcholecystectomy Patients
- Laparoscopic Removal of a Retained Gallbladder with Remnant Cystic Duct Calculi
- Laparoscopic Resection for the Treatment of Symptomatic Remnant Huge Cystic Duct with Stone after Laparoscopic Cholecystectomy