Imaging Sci Dent.
2016 Sep;46(3):173-178. 10.5624/isd.2016.46.3.173.
The effectiveness of optical coherence tomography for evaluating peri-implant tissue: A pilot study
- Affiliations
-
- 1Department of Oral Implantology and Regenerative Dental Medicine, Graduate School of Medical and Dental Sciences, Tokyo Medical and Dental University, Tokyo, Japan. mshiota.impl@tmd.ac.jp
- 2Department of Oral Surgery, Jichii Medical University Hospital, Tochigi, Japan.
- 3Division of Oral and Dental Surgery, Department of Advanced Medicine, National Hospital for Geriatric Medicine, National Center for Geriatrics and Gerontology, Obu, Japan.
- KMID: 2408249
- DOI: http://doi.org/10.5624/isd.2016.46.3.173
Abstract
- PURPOSE
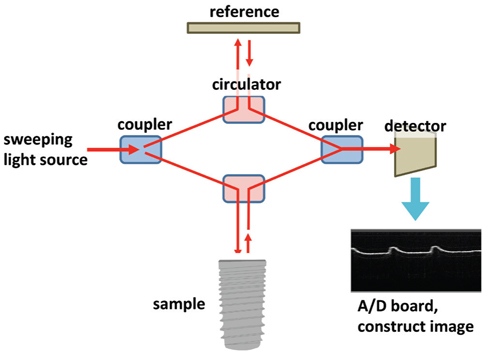
Optical coherence tomography (OCT) has been investigated as a novel diagnostic imaging tool. The utilisation of this equipment has been evaluated through several studies in the field of dentistry. The aim of this preliminary study was to determine through basic experiments the effectiveness of OCT in implant dentistry.
MATERIALS AND METHODS
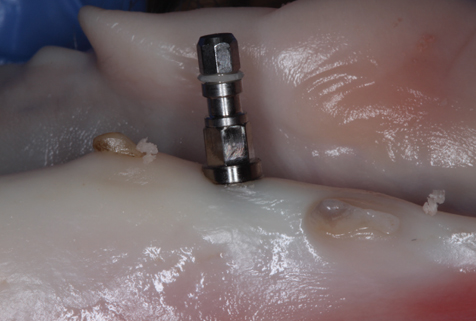
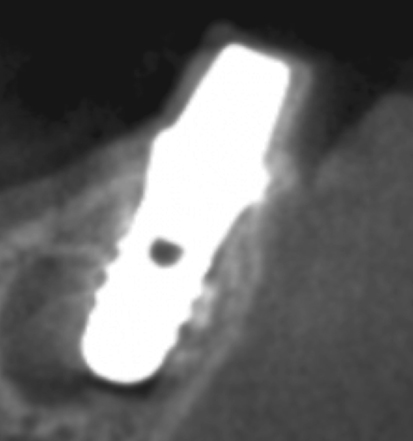
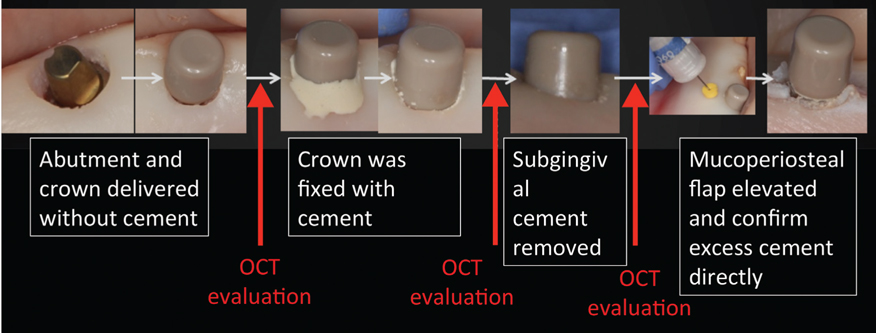
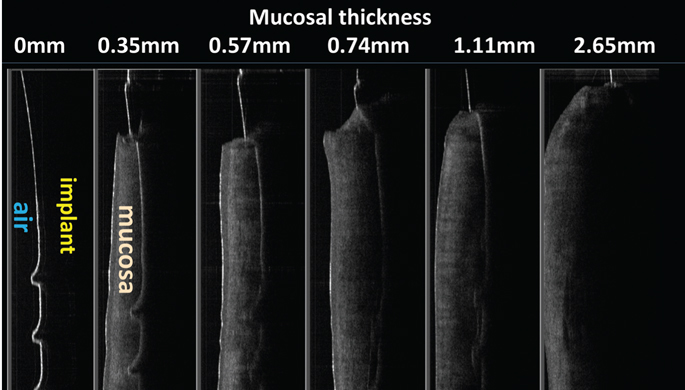
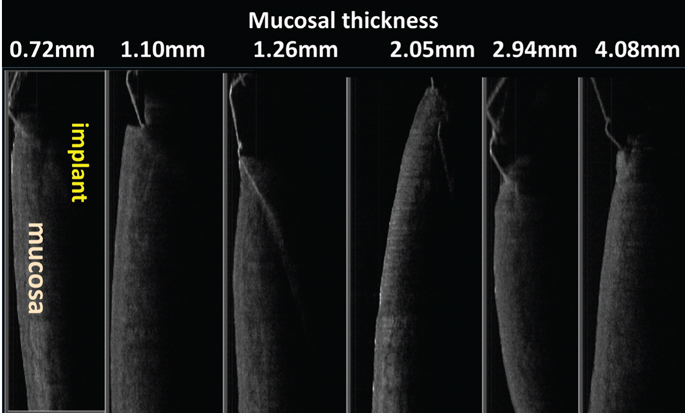
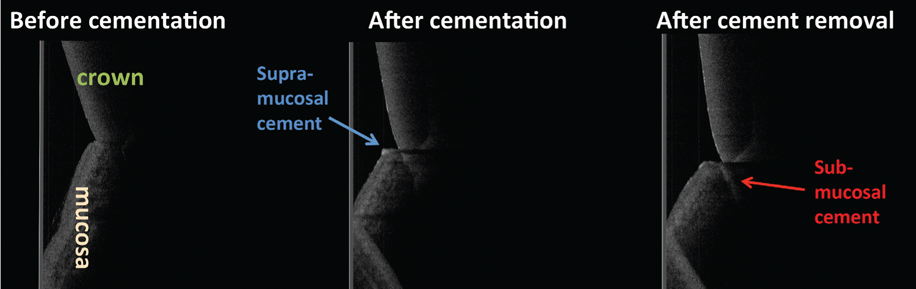
To assess detection ability, we captured OCT images of implants in each of the following situations: (1) implants covered with mucosae of various thicknesses that were harvested from the mandibles of pigs; (2) implants installed in the mandibles of pigs; and (3) implants with abutments and crowns fixed with temporary cement. The OCT images were captured before cementation, after cementation, and after removing the excess submucosal cement.
RESULTS
If the thickness of the mucosa covering the implant body was less than 1 mm, the images of the implants were clearly detected by OCT. In the implants were installed in pigs' mandibles, it was difficult to capture clear images of the implant and alveolar bone in most of the samples. Remnants of excess cement around the implants were visible in most samples that had a mucosa thickness of less than 3 mm.
CONCLUSION
Currently, OCT imaging of implants is limited. Cement remnants at the submucosal area can be detected in some cases, which can be helpful in preventing peri-implant diseases. Still, though there are some restrictions to its application, OCT could have potential as an effective diagnostic instrument in the field of implant dentistry as well.
MeSH Terms
Figure
Reference
-
1. Fujimoto JG. Optical coherence tomography for ultrahigh resolution in vivo imaging. Nat Biotechnol. 2003; 21:1361–1367.
Article2. Huang D, Swanson EA, Lin CP, Schuman JS, Stinson WG, Chang W, et al. Optical coherence tomography. Science. 1991; 254:1178–1181.
Article3. Wada I, Shimada Y, Ikeda M, Sadr A, Nakashima S, Tagami J, et al. Clinical assessment of non carious cervical lesion using swept-source optical coherence tomography. J Biophotonics. 2015; 8:846–854.
Article4. Nakagawa H, Sadr A, Shimada Y, Tagami J, Sumi Y. Validation of swept source optical coherence tomography (SS-OCT) for the diagnosis of smooth surface caries in vitro. J Dent. 2013; 41:80–89.
Article5. Albrektsson T, Brånemark PI, Hansson HA, Lindström J. Osseointegrated titanium implants. Requirements for ensuring a long-lasting, direct bone-to-implant anchorage in man. Acta Orthop Scand. 1981; 52:155–170.6. Albrektsson T, Zarb G, Worthington P, Eriksson AR. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986; 1:11–25.7. van Steenberghe D, Lekholm U, Bolender C, Folmer T, Henry P, Herrmann I, et al. Applicability of osseointegrated oral implants in the rehabilitation of partial edentulism: a prospective multicenter study on 558 fixtures. Int J Oral Maxillofac Implants. 1990; 5:272–281.8. Buser D, Mericske-Stern R, Bernard JP, Behneke A, Behneke N, Hirt HP, et al. Long-term evaluation of non-submerged ITI implants. Part 1: 8-year life table analysis of a prospective multi-center study with 2359 implants. Clin Oral Implants Res. 1997; 8:161–172.
Article9. Heitz-Mayfield LJ, Needleman I, Salvi GE, Pjetursson BE. Consensus statements and clinical recommendations for prevention and management of biologic and technical implant complications. Int J Oral Maxillofac Implants. 2014; 29:Suppl. 346–350.
Article10. Lang NP, Berglundh T. Periimplant diseases: where are we now? - Consensus of the Seventh European Workshop on Periodontology. J Clin Periodontol. 2011; 38:Suppl 11. 178–181.
Article11. Pan Y, Lavelle JP, Bastacky SI, Meyers S, Pirtskhalaishvili G, Zeidel ML, et al. Detection of tumorigenesis in rat bladders with optical coherence tomography. Med Phys. 2001; 28:2432–2440.
Article12. Chen SF, Lu CW, Tsai MT, Wang YM, Yang C, Chiang CP. Oral cancer diagnosis with optical coherence tomography. Conf Proc IEEE Eng Med Biol Soc. 2005; 7:7227–7229.13. Wilder-Smith P, Krasieva T, Jung WG, Zhang J, Chen Z, Osann K, et al. Noninvasive imaging of oral premalignancy and malignancy. J Biomed Opt. 2005; 10:051601.
Article14. Wismeijer D, Brägger U, Evans C, Kapos T, Kelly JR, Millen C, et al. Consensus statements and recommended clinical procedures regarding restorative materials and techniques for implant dentistry. Int J Oral Maxillofac Implants. 2014; 29:Suppl. 137–140.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Quantitative measurement of peri-implant bone defects using optical coherence tomography
- Optical Imaging and Its Clinical Application in Otorhinolaryngology
- Availability of Optical Coherence Tomography in Diagnosis and Classification of Choroidal Neovascularization
- Influence of soft tissue and bone thickness on the dimensional change of peri-implant soft tissues: A clinical follow-up study
- Optical Coherence Tomography in the Evalution of Fitering Bleb after Trabeculectomy