J Korean Acad Nurs Adm.
2018 Mar;24(2):107-117. 10.11111/jkana.2018.24.2.107.
Effect of Crowding and Nurse Staffing on Time to Antibiotic Administration for Patients with Pneumonia in an Emergency Department
- Affiliations
-
- 1College of Nursing, Seoul National University, Korea.
- 2College of Nursing, Research Institute of Nursing Science, Seoul National University, Korea. sunghcho@snu.ac.kr
- KMID: 2408118
- DOI: http://doi.org/10.11111/jkana.2018.24.2.107
Abstract
- PURPOSE
This study was conducted to identify the effect of crowding and nurse staffing on time to antibiotic administration for pneumonia patients in an emergency department (ED).
METHODS
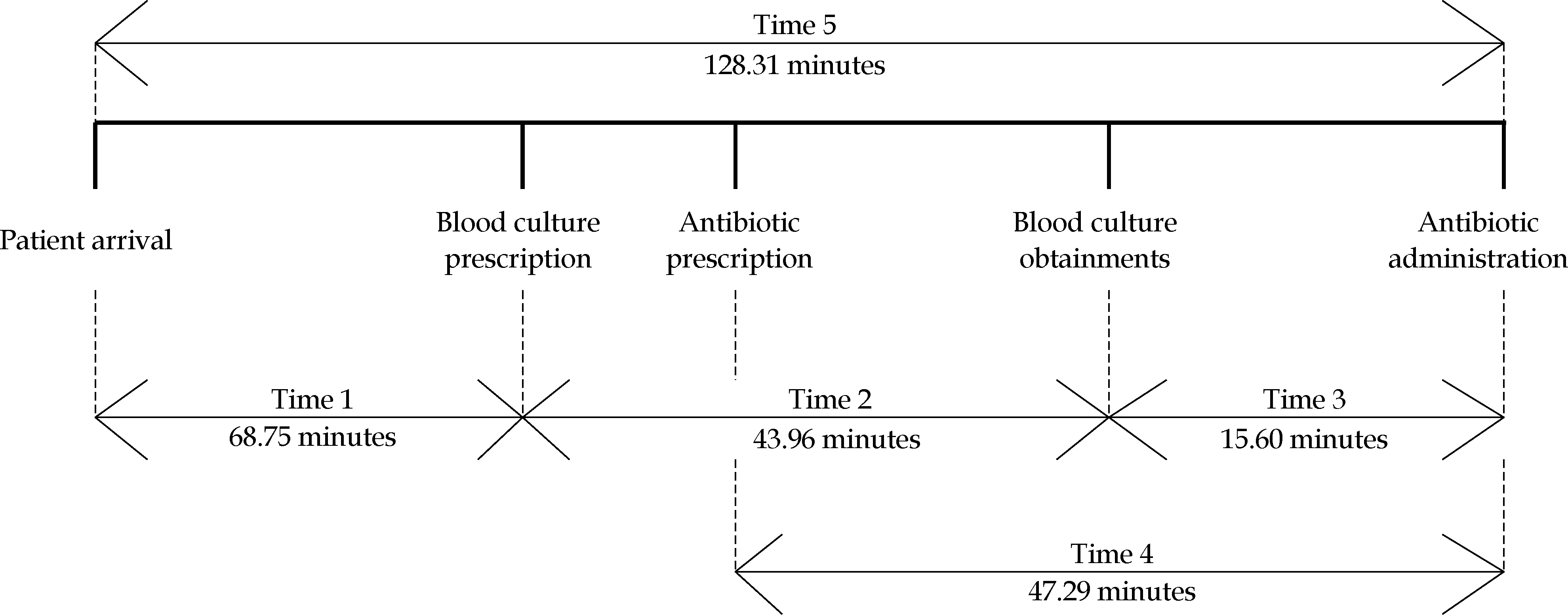
The sample included pneumonia patients visiting an ED from November 1, 2014 to February 28, 2015. Crowding was measured using ED occupancy rate, nurse staffing was measured as total length of stay per nurse and number of patients per nurse and the time duration was measured for the following processes: from patient arrival to prescription, from prescription to blood culture and antibiotic administration, and from blood culture to antibiotic administration. Data collected from the electronic medical records were analyzed using multivariate analyses.
RESULTS
The mean times from arrival to antibiotics administration, from prescription to antibiotic administration, and from blood culture to antibiotic administration were 128.31, 47.29, and 15.60 minutes, respectively. Crowding, nurse staffing, work experience of the nurse and severity of the patient influenced the time duration of each process from patient arrival to antibiotic administration.
CONCLUSION
The results reveal that crowding and nurse staffing affect length of time to antibiotic administration in pneumonia patients. Guidelines for safe nurse staffing in ED are required to improve patient outcomes.
Keyword
MeSH Terms
Figure
Reference
-
1. Moskop JC, Sklar DP, Geiderman JM, Schears RM, Bookman KJ. Emergency department crowding, Part 1-concept, causes, and moral consequences. Annals of Emergency Medicine. 2009; 53(5):605–611. https://doi.org/10.1016/j.annemergmed.2008.09.019.
Article2. Hoot NR, Aronsky D. Systematic review of emergency department crowding: Causes, effects, and solutions. Annals of Emergency Medicine. 2008; 52(2):126–136.e1. https://doi.org/10.1016/j.annemergmed.2008.03.014.
Article3. Crowding. Annals of Emergency Medicine. 2006; 47(6):585. https://doi.org/10.1016/j.annemergmed.2006.02.025.4. Hwang U, Richardson LD, Sonuyi TO, Morrison RS. The effect of emergency department crowding on the management of pain in older adults with hip fracture. Journal of the American Geriatrics Society. 2006; 54(2):270–275. https://doi.org/10.1111/j.1532-5415.2005.00587.x.
Article5. Boyle A, Abel G, Raut P, Austin R, Dhakshinamoorthy V, Ayya-muthu R, et al. Comparison of the International Crowding Measure in Emergency Departments (ICMED) and the National Emergency Department Overcrowding Score (NEDOCS) to measure emergency department crowding: Pilot study. Emergency Medicine Journal: EMJ. 2016; 33(5):307–312. https://doi.org/10.1136/emermed-2014-203616.
Article6. Jones SS, Allen TL, Flottemesch TJ, Welch SJ. An independent evaluation of four quantitative emergency department crowding scales. Academic Emergency Medicine. 2006; 13(11):1204–1211. https://doi.org/10.1197/j.aem.2006.05.021.
Article7. Pines JM, Griffey RT. What We have learned from a decade of ED crowding research. Academic Emergency Medicine. 2015; 22(8):985–987. https://doi.org/10.1111/acem.12716.
Article8. Korn R, Mansfield M. ED overcrowding: An assessment tool to monitor ED registered nurse workload that accounts for admitted patients residing in the emergency department. Journal of Emergency Nursing. 2008; 34(5):441–446. https://doi.org/10.1016/j.jen.2007.06.025.
Article9. Green LV, Soares J, Giglio JF, Green RA. Using queueing theory to increase the effectiveness of emergency department provider staffing. Academic Emergency Medicine. 2006; 13(1):61–68. https://doi.org/10.1197/j.aem.2005.07.034.
Article10. Pines JM, Hollander JE, Localio AR, Metlay JP. The association between emergency department crowding and hospital performance on antibiotic timing for pneumonia and percutaneous intervention for myocardial infarction. Academic Emergency Medicine. 2006; 13(8):873–878. https://doi.org/10.1197/j.aem.2006.03.568.
Article11. Kane RL, Shamliyan TA, Mueller C, Duval S, Wilt TJ. The association of registered nurse staffing levels and patient outcomes: Systematic review and meta-analysis. Medical Care. 2007; 45(12):1195–1204. https://doi.org/10.1097/MLR.0b013e3181468ca3.12. Hoxhaj S, Moseley MG, Reese CL. 2004 SAEM Annual Meeting Abstracts. Nurse staffing levels affect the number of emergency department patients who leave without treatment. Academic Emergency Medicine. 2004; 11(5):459–460.13. Kulstad EB, Sikka R, Sweis RT, Kelley KM, Rzechula KH. ED overcrowding is associated with an increased frequency of medication errors. The American Journal of Emergency Medicine. 2010; 28(3):304–309. https://doi.org/10.1016/j.ajem.2008.12.014.
Article14. National Emergency Medical Center (KR). 2017 Guideline for emergency medical institution evaluation [Internet]. National Emergency Medical Center;2017. [cited September 7, 2017]. Available from:. http://portal.nemc.or.kr/init.do?systemauth=06&sytmidno=29&menuflag=&linkurl=.15. National Emergency Medical Center (KR). 2016 Guideline for emergency medical institution evaluation [Internet]. National Emergency Medical Center;2016. [cited May 24, 2017]. Available from:. http://portal.nemc.or.kr/init.do?systemauth=06&sytmidno=29&menuflag=1161&linkurl=/board/new_notice_board.do.16. Health Insurance Review & Assessment Service (KR). 2017 Medical care expenses assessment plan [Internet]. Wonju: Health Insurance Review & Assessment Service;2017. [cited September 27, 2017]. Available from:. http://www.hira.or.kr/bbsDummy.do?pgmid=HIRAA020002000100&brdScnBltNo=4&brdBltNo=6313.17. Statistics Korea. Annual report on the cause of death statistics [Internet]. Deajeon: Statistics Korea;2015. [cited May 24, 2017]. Available from:. http://kostat.go.kr/portal/korea/kor_nw/2/6/2/index.board.18. Houck PM, Bratzler DW, Nsa W, Ma A, Bartlett JG. Timing of antibiotic administration and outcomes for Medicare patients hospitalized with community-acquired pneumonia. Archives of Internal Medicine. 2004; 164(6):637–644. https://doi.org/10.1001/archinte.164.6.637.
Article19. The Joint Commission. Specifications manual for Joint Commission National Quality Core Measures(2010A1) [Internet]. Illinois: The Joint Commission;2010. [cited May 24, 2017]. Available from:. https://manual.jointcommission.org/releases/archive/TJC2010B/Pneumonia.html.20. Fee C, Weber EJ, Maak CA, Bacchetti P. Effect of emergency department crowding on time to antibiotics in patients admitted with community-acquired pneumonia. Annals of Emergency Medicine. 2007; 50(5):501–509,509.e1. https://doi.org/10.1016/j.annemergmed.2007.08.003.
Article21. Pines JM, Locallo AR, Hollander JE, Baxt WG, Lee H, Phillips C, et al. The impact of emergency department crowding measures on time to antibiotics for patients with community-acquired pneumonia. Annals of Emergency Medicine. 2007; 50(5):510–516. https://doi.org/10.1016/j.annemergmed.2007.07.021.
Article22. Fee C, Weber EJ, Bacchetti P, Maak CA. Effect of emergency department crowding on pneumonia admission care components. The American Journal of Managed Care. 2011; 17(4):269–278.23. Wuerz RC, Milne LW, Eitel DR, Travers D, Gilboy N. Reliability and validity of a new five-level triage instrument. Academic Emergency Medicine. 2000; 7(3):236–242. https://doi.org/10.1111/j.1553-2712.2000.tb01066.x.
Article24. Ministry of Health and Welfare (KR). 2015 emergency department evaluation [Internet]. Sejong: Ministry of Health and Welfare;2015. [cited September 22, 2017]. Available from:. http://www.mohw.go.kr/front_new/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&CONT_SEQ=330291&page=1.25. Ministry of Health and Welfare (KR). Enforcement Rule of The Medical Service Act. Ordinance of the Ministry of Health and Welfare No. 484, March 7. 2017.26. Ministry of Health and Welfar (KR). Health Insurance Act Salary ․ Non-salary list table and salary relative value score. Ministry of Health and Welfare Notice No. 2017-59, March 29. 2017.27. California. AB-394 Health facilities: Nursing staff. Assembly Bill No. 394 Chapter 945. An act to add Section 2725.3 to the Business and Professions Code, and to add Section 1276.4 to the Health and Safety Code, relating to health care.28. Victoria, Australia. Safe Patient Care (Nurse to Patient and Midwife to Patient Ratios) Act 2015. No. 51 of 2015, Assented to 13 October. 2015.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Impact of emergency room occupancy on the timing of antibiotic administration in patients with septic shock who visited the emergency room
- Impact of Nurse Staffing Level and Oral Care on Hospital Acquired Pneumonia in Long-term Care Hospitals
- Competency of Nursing Performance and Job Satisfaction of Operating Room Nurse by Type of Nurse Staffing
- The Effects of Long-term Care Hospitals’ Nurse Staffing Level on Patient Outcomes: Differences according to Region
- The Association of Nurse Staffing Levels and Patient Outcome in Intensive Care Units