J Korean Neurosurg Soc.
2018 Mar;61(2):258-266. 10.3340/jkns.2017.0188.
Sacral Insufficiency Fractures: How to Classify?
- Affiliations
-
- 1Hannover Region Public Health Department, Hannover Region, Hannover, Germany. gesabakker@gmx.de
- 2Department for Radiology and Neuroradiology, KRH Nordstadt, Hannover, Germany.
- 3Institute for Medical Statistics, Computer Science and Epidemiology IMSIE, University of Cologne, Cologne, Germany.
- 4Department of Traumatology and Orthopedics, KRH Nordstadt, Hannover, Germany.
- KMID: 2408028
- DOI: http://doi.org/10.3340/jkns.2017.0188
Abstract
OBJECTIVE
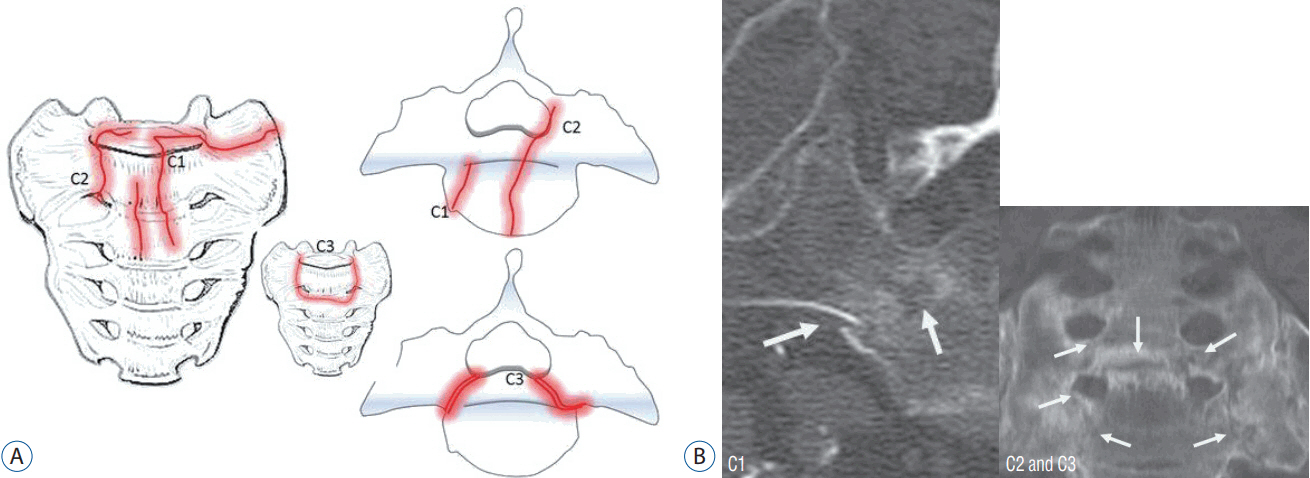
The diagnosis of insufficiency fractures of the sacrum in an elder population increases annually. Fractures show very different morphology. We aimed to classify sacral insufficiency fractures according to the position of cortical break and possible need for intervention.
METHODS
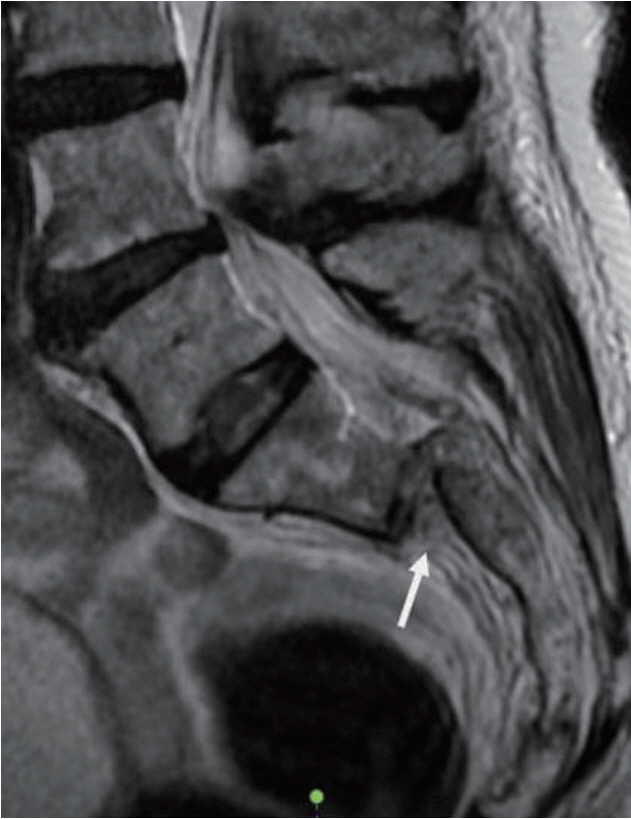
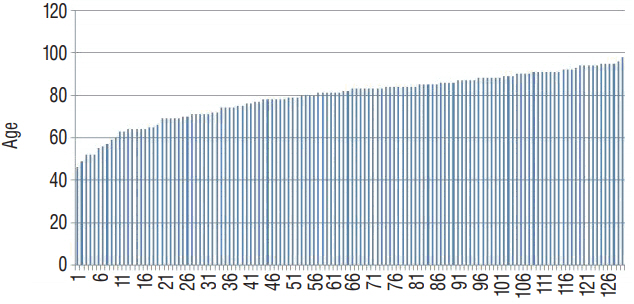
Between January 1, 2008 and December 31, 2014, all patients with a proven fracture of the sacrum following a low-energy or an even unnoticed trauma were prospectively registered : 117 females and 13 males. All patients had a computer tomography of the pelvic ring, two patients had a magnetic resonance imaging additionally : localization and involvement of the fracture lines into the sacroiliac joint, neural foramina or the spinal canal were identified.
RESULTS
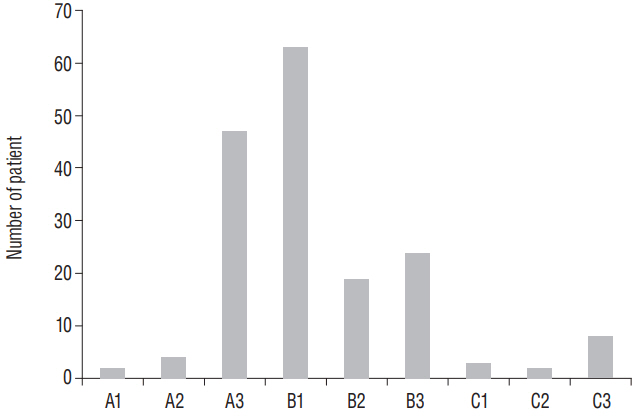
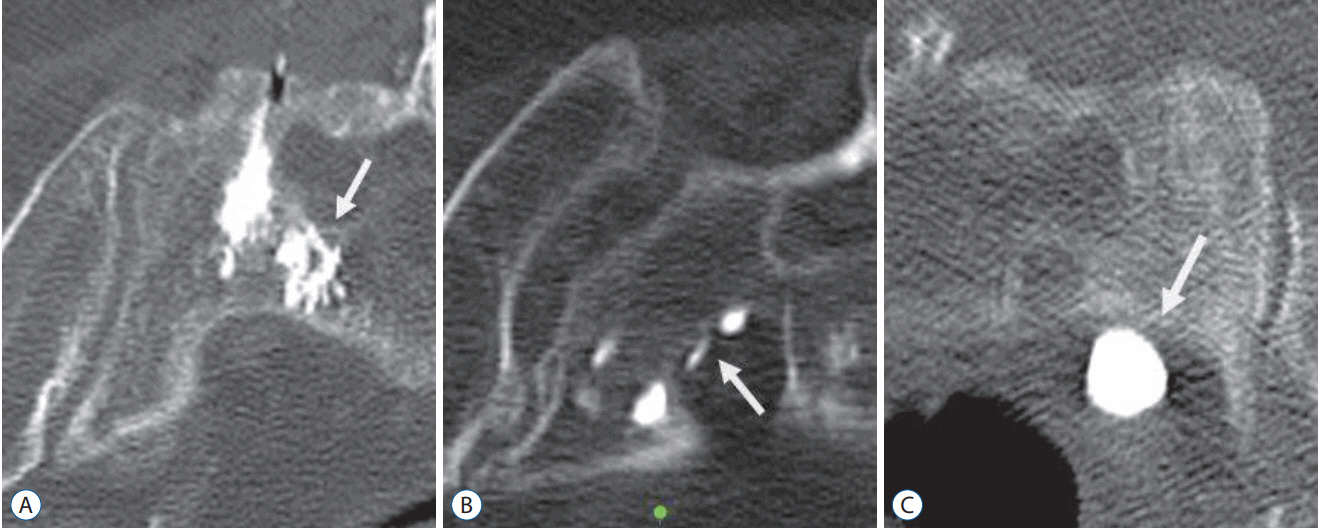
Patients were aged between 46 and 98 years (mean, 79.8 years). Seventy-seven patients had an unilateral fracture of the sacral ala, 41 bilateral ala fractures and 12 patients showed a fracture of the sacral corpus : a total of 171 fractures were analyzed. The first group A included fractures of the sacral ala which were assessed to have no or less mechanical importance (n=53) : fractures with no cortical disruption ("bone bruise") (A1; n=2), cortical deformation of the anterior cortical bone (A2; n=4), and fracture of the anterolateral rim of ala (A3; n=47). Complete fractures of the sacral ala (B; n=106) : parallel to the sacroiliac joint (B1; n=63), into the sacroiliac joint (B2; n=19), and involvement of the sacral foramina respectively the spinal canal (B3; n=24). Central fractures involving the sacral corpus (C; n=12) : fracture limited to the corpus or finishing into one ala (C1; n=3), unidirectional including the neural foramina or the spinal canal or both (C2; n=2), and horizontal fractures of the corpus with bilateral sagittal completion (C3; n=8). Sixty-eight fractures proceeded into the sacroiliac joint, 34 fractures showed an injury of foramina or canal.
CONCLUSION
The new classification allowes the differentiation of fractures of less mechanical importance and a risk assessment for possible polymethyl methacrylate leaks during sacroplasty in the direction of the neurological structures. In addition, identification of instable fractures in need for laminectomy and surgical stabilization is possible.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Albertsen AM, Egund N, Jurik AG. Fatigue fracture of the sacral bone associated with septic arthritis of the symphysis pubis. Skeletal Radiol. 24:605–607. 1995.
Article2. Alnaib M, Waters S, Shanshal Y, Caplan N, Jones S, St Clair Gibson A, et al. Combined pubic rami and sacral osteoporotic fractures: a prospective study. J Orthop Traumatol. 13:97–103. 2012.
Article3. Aretxabala I, Fraiz E, Pérez-Ruiz F, Ríos G, Calabozo M, Alonso-Ruiz A. Sacral insufficiency fractures. High association with pubic rami fractures. Clin Rheumatol. 19:399–401. 2000.
Article4. Bayley E, Srinivas S, Boszczyk BM. Clinical outcomes of sacroplasty in sacral insufficiency fractures: a review of the literature. Eur Spine J. 18:1266–1271. 2009.
Article5. Choi KC, Shin SH, Lee DC, Shim HK, Park CK. Effects of percutaneous sacroplasty on pain and morbility in sacral insufficiency fracture. J Korean Neurosurg Soc. 60:60–66. 2017.
Article6. Connolly LP, Drubach LA, Connolly SA, Treves ST. Young athletes with low back pain: skeletal scintigraphy of conditions other than pars interarticularis stress. Clin Nucl Med. 29:689–693. 2004.
Article7. Cooper KL, Beabout JW, Swee RG. Insufficiency fractures of the sacrum. Radiology. 156:15–20. 1985.
Article8. Denis F, Davis S, Comfort T. Sacral fractures: an important problem. Retrospective analysis of 236 cases. Clin Orthop Relat Res. 227:67–81. 1988.9. Finiels H, Finiels PJ, Jacquot JM, Strubel D. Fractures of the sacrum caused by bone insufficiency. Meta-analysis of 508 cases. Presse Med. 26:1568–1573. 1997.10. Fujii M, Abe K, Hayashi K, Kosuda S, Yano F, Watanabe S, et al. Honda sign and variants in patients suspected of having a sacral insufficiency fracture. Clin Nucl Med. 30:165–169. 2005.
Article11. Gotis-Graham I, McGuigan L, Diamond T, Portek I, Quinn R, Sturgess A, et al. Sacral insufficiency fractures in the elderly. J Bone Joint Surg Br. 76:882–886. 1994.
Article12. Guilbeau JC, Arrivé L, Maruice F, Nahum H. Spontaneous fracture of the sacrum due to “insufficiency”. An overlooked cause of low lumbago in elderly women. J Radiol. 67:741–744. 1986.13. Hak DJ, Baran S, Stahel P. Sacral fractures: current strategies in diagnosis and management. Orthopedics. 32:752–757. 2009.
Article14. Hatgis J, Granville M, Jacobson RE, Berti A. Sacral insufficiency fractures: recognation and treatment in patients with current lumbar vertebral compression fractures. Cureus. 9:e1008. 2017.15. Heo DH, Park CK. Percutaneus sacroplasty for non-neoplastic osteoporotic sacral insufficiency fractures. Pain Physician. 20:89–94. 2017.16. Isler B. Lumbosacral lesions associated with pelvic ring injuries. J Orthop Trauma. 4:1–6. 1990.
Article17. Judet R, Judet J, Letournel E. Fractures of the acetabulum: classification and surgical approaches for open reduction. Preliminary report. J Bone Joint Surg Am. 46:1615–1646. 1964.18. Linstrom NJ, Heiserman JE, Kortman KE, Crawford NR, Baek S, Anderson RL, et al. Anatomical and biomechanical analyses of the unique and consistent locations of sacral insuffiency fractures. Spine (Phila Pa 1976). 34:309–315. 2009.
Article19. Longhino V, Bonora C, Sansone V. The management of sacral stress fractures: current concepts. Clin Cases Miner Bone Metab. 8:19–23. 2011.20. Lourie H. Spontaneous osteoporotic fracture of the sacrum. An unrecognized syndrome of the elderly. JAMA. 248:715–717. 1982.
Article21. Majo NM, Helms CA. Sacral stress fractures in long-distance runners. AJR Am J Roentgenol. 174:727–729. 2000.
Article22. Richards AM, Coleman NW, Knight TA, Belkoff SM, Mears SC. Bone density and cortical thickness in normal, osteopenic, and osteoporotic sacra. J Osteoporos. 2010:504078. 2010.
Article23. Rommens PM, Hofmann A. Comprehensive classification of fragility fractures of the pelvic ring: recommendations for surgical treatment. Injury. 44:1733–1744. 2013.
Article24. Rommens PM, Wagner D, Hofmann A. Surgical management of osteoporotic pelvic fractures: a new challenge. Eur J Trauma Emerg Surg. 38:499–509. 2012.
Article25. Rousière M, Kahan A, Job-Deslandre C. Postpartal sacral fracture without osteoporosis. Joint Bone Spine. 68:71–73. 2001.
Article26. Roy-Camille R, Saillant G, Gagna G, Mazel C. Transverse fracture of the upper sacrum. Suicidal jumper’s fracture. Spine (Phila Pa 1976). 10:838–845. 1985.27. Schindler OS, Watura R, Cobby M. Sacral insufficiency fractures. J Orthop Surg (Hong Kong). 15:339–346. 2007.
Article28. Strange-Vognsen HH, Lebech A. An unusual type of fracture in the upper sacrum. J Orthop Trauma. 5:200–203. 1991.
Article29. Tile M. Acute pelvic fractures: I. Causation and classification. J Am Acad Orthop Surg. 4:143–151. 1996.
Article30. Tötterman A, Glott T, Madsen JE, Røise O. Unstable sacral fractures: associated injuries and morbidity at 1 year. Spine (Phila Pa 1976). 31:E628–E635. 2006.31. Weber M, Hasler P, Gerber H. Insufficiency fractures of the sacrum. Twenty cases and review of the literature. Spine (Phila Pa 1976). 18:2507–2512. 1993.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of S1 Radiculopathy in Sacral Insufficiency Fracture without Fracture Line
- MR Findings of Sacral Insufficiency Fractures in Osteoporotic Patients: Two Cases Report
- Sacral Insufficiency Fracture, Usually Overlooked Cause of Lumbosacral Pain
- Sequential Sacral Insufficiency Fracture After Unilateral Pubic Fractures: A Case Report
- Usefulness of Kyphoplasty in Sacral Insufficiency Fracture: A Case Report