J Clin Neurol.
2018 Apr;14(2):200-205. 10.3988/jcn.2018.14.2.200.
Optical Coherence Tomography versus Visual Evoked Potentials for Detecting Visual Pathway Abnormalities in Patients with Neuromyelitis Optica Spectrum Disorder
- Affiliations
-
- 1Department of Neurology, Dongguk University Ilsan Hospital, Goyang, Korea.
- 2Department of Neurology, Research Institute and Hospital of National Cancer Center, Goyang, Korea.
- 3Department of Ophthalmology, Dongguk University Ilsan Hospital, Goyang, Korea.
- 4Department of Occupational and Environmental Medicine, Dongguk University Ilsan Hospital, Goyang, Korea.
- 5Department of Neurology, Ilsan Paik Hospital, Inje University College of Medicine, Goyang, Korea. joongyangcho@gmail.com
- KMID: 2407947
- DOI: http://doi.org/10.3988/jcn.2018.14.2.200
Abstract
- BACKGROUND AND PURPOSE
Optical coherence tomography (OCT) and visual evoked potentials (VEPs) can be used to detect optic neuritis (ON). However, the comparative sensitivities of OCT and VEPs for detecting ON in neuromyelitis optica spectrum disorder (NMOSD) are unclear, and so we assessed these sensitivities.
METHODS
This cross-sectional study included 73 patients with aquaporin-4 antibody-seropositive NMOSD, and 101 eyes with ON. The clinical characteristics, visual acuity (VA), Expanded Disability Status Scale (EDSS) scores, OCT peripapillary retinal nerve fiber layer (RNFL) thickness, and VEPs of the patients were evaluated.
RESULTS
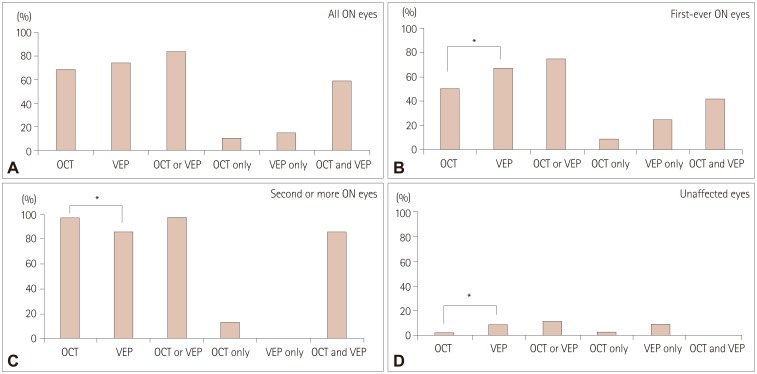
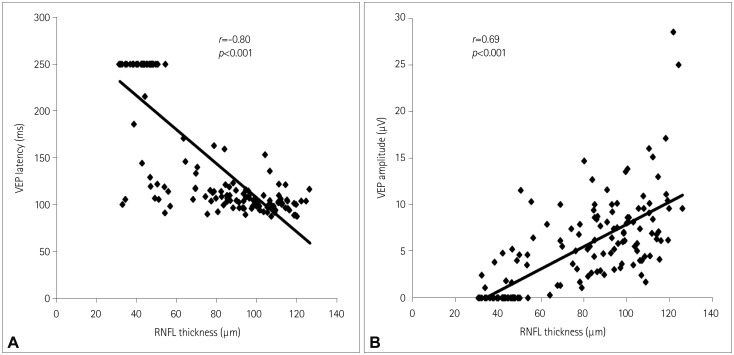
OCT and VEPs were abnormal in 68% and 73% of eyes with a history of ON, respectively, and in 2% and 9% of eyes without ON. Test sensitivities were influenced by the number of ON episodes: the OCT RNFL thickness and VEPs were abnormal in 50% and 67% of the eyes with first-ever ON episode, respectively (p=0.041), with the combination of both tests detecting abnormalities in up to 75% of the eyes. The sensitivities of the OCT RNFL thickness and VEPs increased to 95% and 83%, respectively, after the second or subsequent ON episode (p=0.06), with the combination of both tests detecting abnormalities in 95% of cases. The OCT RNFL thickness and VEP latency/amplitude were correlated with EDSS scores and VA.
CONCLUSIONS
VEPs were superior for detecting subclinical or first-ever ON, while OCT was better for detecting eyes with multiple ON episodes. The correlations of OCT and VEPs with clinical disability measures indicate that these tests are potential markers of the disease burden in NMOSD.
Keyword
MeSH Terms
Figure
Reference
-
1. Pfueller CF, Paul F. Imaging the visual pathway in neuromyelitis optica. Mult Scler Int. 2011; 2011:869814. PMID: 22135746.
Article2. Wingerchuk DM, Banwell B, Bennett JL, Cabre P, Carroll W, Chitnis T, et al. International Panel for NMO Diagnosis. International consensus diagnostic criteria for neuromyelitis optica spectrum disorders. Neurology. 2015; 85:177–189. PMID: 26092914.
Article3. Filippi M, Rocca MA, Ciccarelli O, De Stefano N, Evangelou N, Kappos L, et al. MAGNIMS Study Group. MRI criteria for the diagnosis of multiple sclerosis: MAGNIMS consensus guidelines. Lancet Neurol. 2016; 15:292–303. PMID: 26822746.
Article4. Naismith RT, Tutlam NT, Xu J, Shepherd JB, Klawiter EC, Song SK, et al. Optical coherence tomography is less sensitive than visual evoked potentials in optic neuritis. Neurology. 2009; 73:46–52. PMID: 19564583.
Article5. Naismith RT, Tutlam NT, Xu J, Klawiter EC, Shepherd J, Trinkaus K, et al. Optical coherence tomography differs in neuromyelitis optica compared with multiple sclerosis. Neurology. 2009; 72:1077–1082. PMID: 19307541.
Article6. Costello F. Evaluating the use of optical coherence tomography in optic neuritis. Mult Scler Int. 2011; 2011:148394. PMID: 22096626.
Article7. Cettomai D, Pulicken M, Gordon-Lipkin E, Salter A, Frohman TC, Conger A, et al. Reproducibility of optical coherence tomography in multiple sclerosis. Arch Neurol. 2008; 65:1218–1222. PMID: 18779426.
Article8. Bennett JL, de Seze J, Lana-Peixoto M, Palace J, Waldman A, Schippling S, et al. GJCF-ICC&BR. Neuromyelitis optica and multiple sclerosis: seeing differences through optical coherence tomography. Mult Scler. 2015; 21:678–688. PMID: 25662342.
Article9. Di Maggio G, Santangelo R, Guerrieri S, Bianco M, Ferrari L, Medaglini S, et al. Optical coherence tomography and visual evoked potentials: which is more sensitive in multiple sclerosis? Mult Scler. 2014; 20:1342–1347. PMID: 24591532.
Article10. Weinstock-Guttman B, Baier M, Stockton R, Weinstock A, Justinger T, Munschauer F, et al. Pattern reversal visual evoked potentials as a measure of visual pathway pathology in multiple sclerosis. Mult Scler. 2003; 9:529–534. PMID: 14582782.11. MacFadyen DJ, Drance SM, Douglas GR, Airaksinen PJ, Mawson DK, Paty DW. The retinal nerve fiber layer, neuroretinal rim area, and visual evoked potentials in MS. Neurology. 1988; 38:1353–1358. PMID: 3412581.
Article12. Neto SP, Alvarenga RM, Vasconcelos CC, Alvarenga MP, Pinto LC, Pinto VL. Evaluation of pattern-reversal visual evoked potential in patients with neuromyelitis optica. Mult Scler. 2013; 19:173–178. PMID: 22641300.
Article13. Ringelstein M, Kleiter I, Ayzenberg I, Borisow N, Paul F, Ruprecht K, et al. Visual evoked potentials in neuromyelitis optica and its spectrum disorders. Mult Scler. 2014; 20:617–620. PMID: 24009163.
Article14. Costello F, Hodge W, Pan YI, Eggenberger E, Coupland S, Kardon RH. Tracking retinal nerve fiber layer loss after optic neuritis: a prospective study using optical coherence tomography. Mult Scler. 2008; 14:893–905. PMID: 18573837.
Article15. Frederiksen JL, Petrera J. Serial visual evoked potentials in 90 untreated patients with acute optic neuritis. Surv Ophthalmol. 1999; 44(Suppl 1):S54–S62. PMID: 10548117.
Article16. Petzold A, de Boer JF, Schippling S, Vermersch P, Kardon R, Green A, et al. Optical coherence tomography in multiple sclerosis: a systematic review and meta-analysis. Lancet Neurol. 2010; 9:921–932. PMID: 20723847.
Article17. Ratchford JN, Quigg ME, Conger A, Frohman T, Frohman E, Balcer LJ, et al. Optical coherence tomography helps differentiate neuromyelitis optica and MS optic neuropathies. Neurology. 2009; 73:302–308. PMID: 19636050.
Article18. de Seze J, Blanc F, Jeanjean L, Zéphir H, Labauge P, Bouyon M, et al. Optical coherence tomography in neuromyelitis optica. Arch Neurol. 2008; 65:920–923. PMID: 18625858.
Article19. Lange AP, Sadjadi R, Zhu F, Alkabie S, Costello F, Traboulsee AL. Spectral-domain optical coherence tomography of retinal nerve fiber layer thickness in NMO patients. J Neuroophthalmol. 2013; 33:213–219. PMID: 23863782.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Differential Diagnosis between Multiple Sclerosis and Neuromyelitis Optica Spectrum Disorder
- Visual Evoked Potentials for Detecting Visual Pathway Abnormality
- Postpartum Relapse of Neuromyelitis Optica Spectrum Disorder after a Long Period of Spontaneous Remission
- A Case of Neuromyelitis Optica
- Narcolepsy Followed by Intractable Vomiting Caused by Recurrent Brain Involvement in Neuromyelitis Optica Spectrum Disorder