Ann Surg Treat Res.
2018 Apr;94(4):209-215. 10.4174/astr.2018.94.4.209.
Feasibility and oncologic safety of low ligation of inferior mesenteric artery with D3 dissection in cT3N0M0 sigmoid colon cancer
- Affiliations
-
- 1Department of Surgery, Chungnam National University Hospital, Daejeon, Korea. jkim@cnu.ac.kr
- KMID: 2407751
- DOI: http://doi.org/10.4174/astr.2018.94.4.209
Abstract
- PURPOSE
There is no standard consensus for the ligation level of the inferior mesenteric artery during radical resection of sigmoid colon cancer. Especially, there is little research about low ligation combined with D3 dissection. The study was performed to compare feasibility and oncologic safety between low ligation with D3 dissection to high ligation in intermediately advanced sigmoid colon cancer.
METHODS
From January 2008 to December 2013, 134 patients who underwent radical surgery for cT3N0M0 sigmoid colon cancer were evaluated retrospectively. Clinicopathologic factors and oncologic outcomes of high ligation (HL, n = 51) and low ligation (LL, n = 83) groups were compared.
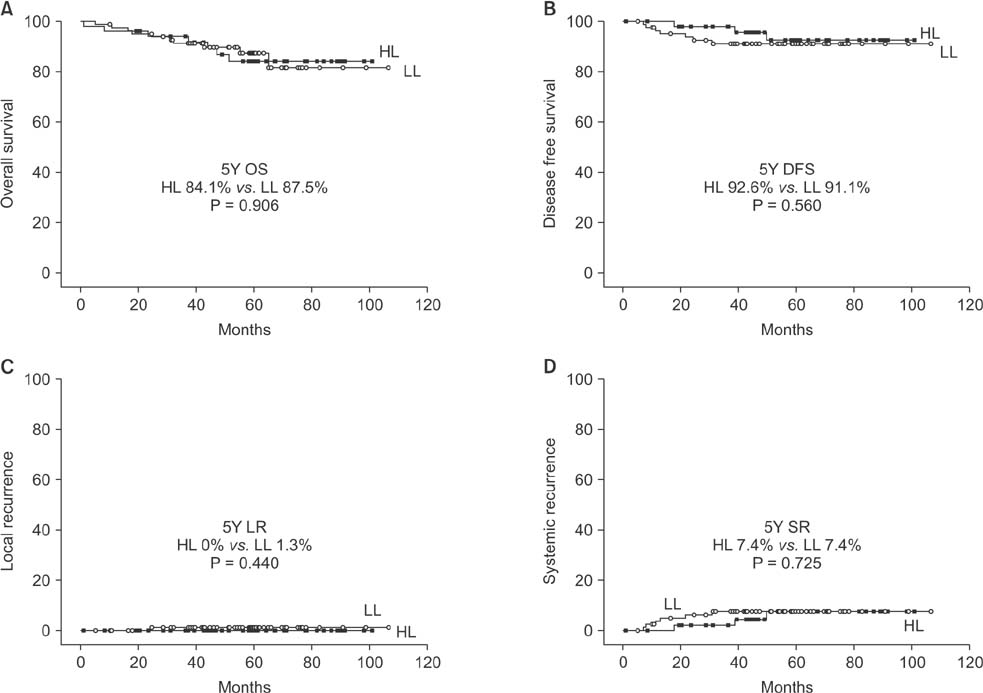
RESULTS
The mean operative time was significantly shorter in LL, and there was no difference in complications, distal margin or number of retrieved lymph node. The tumor size was significantly larger in HL, but there was no difference in number of metastatic lymph node, pT or pN stage. There was no difference in overall survival, disease-free survival, or local and systemic recurrence.
CONCLUSION
In cT3N0M0 sigmoid colon cancers, we suggest that low ligation with D3 dissection can be performed with feasibility and oncological safety.
Keyword
MeSH Terms
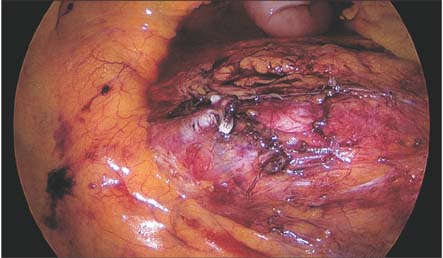
Figure
Cited by 1 articles
-
Colonic hypoperfusion following ligation of the inferior mesenteric artery in rectosigmoid colon cancer patients
Gyung Mo Son, Tae Un Kim, Byung-Soo Park, Hyuk Jae Jung, Sang Su Lee, Ji-Uk Yoon, Jun Woo Lee
Ann Surg Treat Res. 2019;97(2):74-82. doi: 10.4174/astr.2019.97.2.74.
Reference
-
1. Kanemitsu Y, Hirai T, Komori K, Kato T. Survival benefit of high ligation of the inferior mesenteric artery in sigmoid colon or rectal cancer surgery. Br J Surg. 2006; 93:609–615.
Article2. Chin CC, Yeh CY, Tang R, Changchien CR, Huang WS, Wang JY. The oncologic benefit of high ligation of the inferior mesenteric artery in the surgical treatment of rectal or sigmoid colon cancer. Int J Colorectal Dis. 2008; 23:783–788.
Article3. Chen SC, Song XM, Chen ZH, Li MZ, He YL, Zhan WH. Role of different ligation of the inferior mesenteric artery in sigmoid colon or rectal cancer surgery: a meta-analysis. Zhonghua Wei Chang Wai Ke Za Zhi. 2010; 13:674–677.4. Hida J, Okuno K. High ligation of the inferior mesenteric artery in rectal cancer surgery. Surg Today. 2013; 43:8–19.
Article5. Pezim ME, Nicholls RJ. Survival after high or low ligation of the inferior mesenteric artery during curative surgery for rectal cancer. Ann Surg. 1984; 200:729–733.
Article6. Surtees P, Ritchie JK, Phillips RK. High versus low ligation of the inferior mesenteric artery in rectal cancer. Br J Surg. 1990; 77:618–621.
Article7. Corder AP, Karanjia ND, Williams JD, Heald RJ. Flush aortic tie versus selective preservation of the ascending left colic artery in low anterior resection for rectal carcinoma. Br J Surg. 1992; 79:680–682.
Article8. Kawamura YJ, Umetani N, Sunami E, Watanabe T, Masaki T, Muto T. Effect of high ligation on the long-term result of patients with operable colon cancer, particularly those with limited nodal involvement. Eur J Surg. 2000; 166:803–807.
Article9. Yasuda K, Kawai K, Ishihara S, Murono K, Otani K, Nishikawa T, et al. Level of arterial ligation in sigmoid colon and rectal cancer surgery. World J Surg Oncol. 2016; 14:99.
Article10. Slanetz CA Jr, Grimson R. Effect of high and intermediate ligation on survival and recurrence rates following curative resection of colorectal cancer. Dis Colon Rectum. 1997; 40:1205–1218.
Article11. Lange MM, Buunen M, van de Velde CJ, Lange JF. Level of arterial ligation in rectal cancer surgery: low tie preferred over high tie. A review. Dis Colon Rectum. 2008; 51:1139–1145.
Article12. Komen N, Slieker J, de Kort P, de Wilt JH, van der Harst E, Coene PP, et al. High tie versus low tie in rectal surgery: comparison of anastomotic perfusion. Int J Colorectal Dis. 2011; 26:1075–1078.
Article13. Liang JT, Huang KC, Lai HS, Lee PH, Sun CT. Oncologic results of laparoscopic D3 lymphadenectomy for male sigmoid and upper rectal cancer with clinically positive lymph nodes. Ann Surg Oncol. 2007; 14:1980–1990.
Article14. Sekimoto M, Takemasa I, Mizushima T, Ikeda M, Yamamoto H, Doki Y, et al. Laparoscopic lymph node dissection around the inferior mesenteric artery with preservation of the left colic artery. Surg Endosc. 2011; 25:861–866.
Article15. Goh N, Fong SS, How KY, Wong KY, Loong TH, Tay GT. Apical lymph node dissection of the inferior mesenteric artery. Colorectal Dis. 2016; 18:O206–O209.
Article16. Kobayashi M, Okamoto K, Namikawa T, Okabayashi T, Araki K. Laparoscopic lymph node dissection around the inferior mesenteric artery for cancer in the lower sigmoid colon and rectum: is D3 lymph node dissection with preservation of the left colic artery feasible. Surg Endosc. 2006; 20:563–569.17. Titu LV, Tweedle E, Rooney PS. High tie of the inferior mesenteric artery in curative surgery for left colonic and rectal cancers: a systematic review. Dig Surg. 2008; 25:148–157.
Article18. Kawamura YJ, Sakuragi M, Togashi K, Okada M, Nagai H, Konishi F. Distribution of lymph node metastasis in T1 sigmoid colon carcinoma: should we ligate the inferior mesenteric artery? Scand J Gastroenterol. 2005; 40:858–861.
Article19. Hall NR, Finan PJ, Stephenson BM, Lowndes RH, Young HL. High tie of the inferior mesenteric artery in distal colorectal resections: a safe vascular procedure. Int J Colorectal Dis. 1995; 10:29–32.
Article20. Rutegard M, Hemmingsson O, Matthiessen P, Rutegard J. High tie in anterior resection for rectal cancer confers no increased risk of anastomotic leakage. Br J Surg. 2012; 99:127–132.21. Buunen M, Lange MM, Ditzel M, Kleinrensink GJ, van de Velde CJ, Lange JF. Level of arterial ligation in total mesorectal excision (TME): an anatomical study. Int J Colorectal Dis. 2009; 24:1317–1320.
Article22. Bonnet S, Berger A, Hentati N, Abid B, Chevallier JM, Wind P, et al. High tie versus low tie vascular ligation of the inferior mesenteric artery in colorectal cancer surgery: impact on the gain in colon length and implications on the feasibility of anastomoses. Dis Colon Rectum. 2012; 55:515–521.23. Nano M, Dal Corso H, Ferronato M, Solej M, Hornung JP, Dei Poli M. Ligation of the inferior mesenteric artery in the surgery of rectal cancer: anatomical considerations. Dig Surg. 2004; 21:123–126.
Article24. Linhares GK, Martins JL, Fontanezzi F, Patricio Fdos R, Montero EF. Do lesions of the enteric nervous system occur following intestinal ischemia/reperfusion? Acta Cir Bras. 2007; 22:120–124.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Oncologic and Anastomotic Safety of Low Ligation of the Inferior Mesenteric Artery With Additional Lymph Node Retrieval: A Case-Control Study
- Operative safety and oncologic outcomes in rectal cancer based on the level of inferior mesenteric artery ligation: a stratified analysis of a large Korean cohort
- IMA-origin Lymph Node Metastasis in Left Colon Cancer
- Right sided descending and sigmoid colon: its embryological basis and clinical implications
- The Accessory Left Colic Artery Arising from the Superior Mesenteric Artery: A Case Report