J Breast Cancer.
2015 Sep;18(3):296-300. 10.4048/jbc.2015.18.3.296.
Multifocal Bilateral Breast Cancer and Breast Follicular Lymphoma: A Simple Coincidence?
- Affiliations
-
- 1First Department of Surgery, Laiko Hospital, University of Athens, Athens, Greece. amichalinos@hotmail.com
- 2Department of Haematology, Laiko Hospital, University of Athens, Athens, Greece.
- 3First Department of Pathology, University of Athens, Athens, Greece.
- KMID: 2407579
- DOI: http://doi.org/10.4048/jbc.2015.18.3.296
Abstract
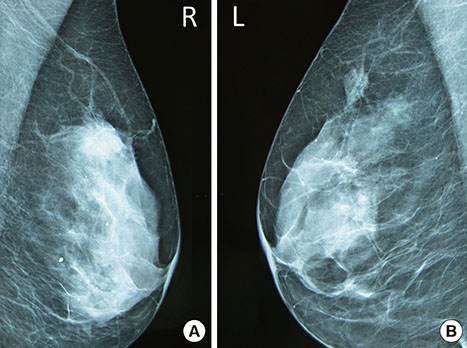
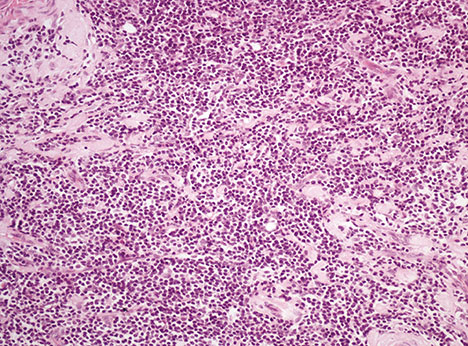
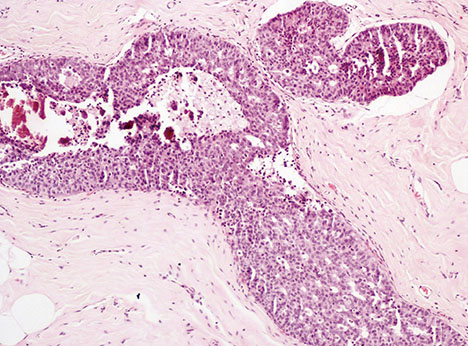
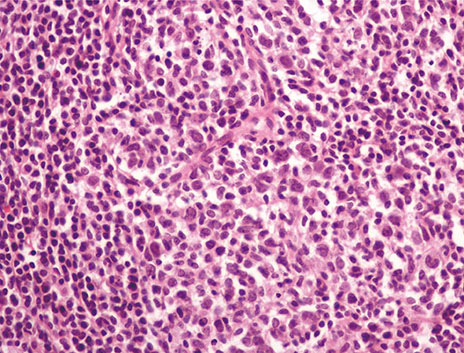
- Breast cancer coexisting with lymphoma is a rare condition with various diagnostic and therapeutic implications. In this report, we describe the case of a 55-year-old Caucasian woman who presented with simultaneous ductal carcinoma in situ of the right breast, and follicular lymphoma involving an inguinal lymph node and the left breast. The patient underwent local excision and radiotherapy for the ductal carcinoma in situ, while a watch and wait strategy was adopted for the lymphoma. Two years later, the patient presented with multifocal ductal carcinoma of the left breast and reappearance of the lymphoma in the left axillary lymph nodes. She underwent bilateral mastectomy, left sentinel node biopsy, and chemotherapy. Synchronous follicular lymphoma and bilateral metachronous breast carcinoma has not been described previously. Diagnosis is based on tissue histology after excision or a needle biopsy. Treatment for these two diseases is distinct, and a multidisciplinary approach should be adopted.
Keyword
MeSH Terms
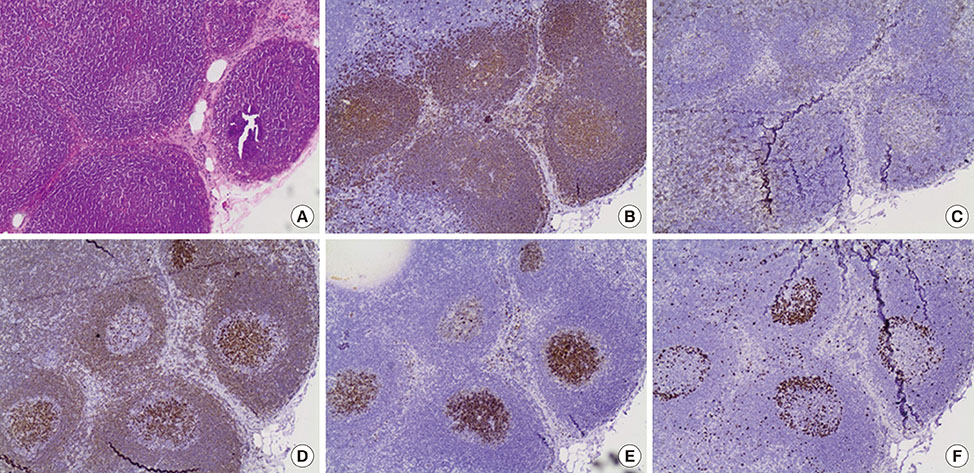
Figure
Reference
-
1. Laudenschlager MD, Tyler KL, Geis MC, Koch MR, Graham DB. A rare case of synchronous invasive ductal carcinoma of the breast and follicular lymphoma. S D Med. 2010; 63:123–125.2. Cuff KE, Dettrick AJ, Chern B. Synchronous breast cancer and lymphoma: a case series and a review of the literature. J Clin Pathol. 2010; 63:555–557.
Article3. Cox J, Lunt L, Webb L. Synchronous presentation of breast carcinoma and lymphoma in the axillary nodes. Breast. 2006; 15:246–252.
Article4. Barranger E, Marpeau O, Uzan S, Antoine M. Axillary sentinel node involvement by breast cancer coexisting with B-cell follicular lymphoma in nonsentinel nodes. Breast J. 2005; 11:227–228.
Article5. Cohen PL, Brooks JJ. Lymphomas of the breast: a clinicopathologic and immunohistochemical study of primary and secondary cases. Cancer. 1991; 67:1359–1369.
Article6. Cheung KJ, Tam W, Chuang E, Osborne MP. Concurrent invasive ductal carcinoma and chronic lymphocytic leukemia manifesting as a collision tumor in breast. Breast J. 2007; 13:413–417.
Article7. Wiseman C, Liao KT. Primary lymphoma of the breast. Cancer. 1972; 29:1705–1712.
Article8. Tamaoki M, Nio Y, Tsuboi K, Nio M, Tamaoki M, Maruyama R. A rare case of non-invasive ductal carcinoma of the breast coexisting with follicular lymphoma: a case report with a review of the literature. Oncol Lett. 2014; 7:1001–1006.
Article9. Arana S, Vasquez-Del-Aguila J, Espinosa M, Peg V, Rubio IT. Lymphatic mapping could not be impaired in the presence of breast carcinoma and coexisting small lymphocytic lymphoma. Am J Case Rep. 2013; 14:322–325.
Article10. Miles EF, Jacimore LL. Synchronous bilateral breast carcinoma and axillary non-Hodgkin lymphoma: a case report and review of the literature. Case Rep Oncol Med. 2012; 2012:685919.
Article11. Garg NK, Bagul NB, Rubin G, Shah EF. Primary lymphoma of the breast involving both axillae with bilateral breast carcinoma. World J Surg Oncol. 2008; 6:52.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Incidentally detected insitu ductal carcinoma with mastitis
- Concurrent Invasive Ductal Carcinoma of the Breast and Malignant Follicular Lymphoma, Initially Suspected to Be Metastatic Breast Cancer: A Case Report
- Breast Lymphoma: A Report of 2 Cases
- Primary Follicular Lymphoma in a Male Breast: A Case Report
- Bilateral breast carcinoma