Anesth Pain Med.
2017 Oct;12(4):357-362. 10.17085/apm.2017.12.4.357.
Effect of needle approach to the axillary artery on transarterial axillary brachial plexus block quality
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Gachon University Gil Medical Center, Incheon, Korea. mikeum2@gilhospital.com
- 2Department of Anesthesiology and Pain Medicine, Younsei University College of Medicine, Seoul, Korea.
- KMID: 2405855
- DOI: http://doi.org/10.17085/apm.2017.12.4.357
Abstract
- BACKGROUND
The authors sought to determine whether a shallow needle approach to the axillary artery would improve complete sensory blocks of median, radial, and ulnar nerves as compared with a perpendicular approach when transarterial axillary block is performed using a scalp vein needle (23G, 3/4').
METHODS
Fifty-four patients were allocated equally to a perpendicular group (the PA group) or a shallow approach group (SA group). Sensory and motor scores were evaluated and compared in the two groups at 5-minute intervals for 20 minutes after block. The main outcome variables were rates of blockage of median, radial, and ulnar nerves.
RESULTS
Excellent block rates (defined as completion of surgery using brachial plexus block alone) were obtained in both groups (SA group 77.8% vs. PA group 70.3%, P = 0.755). However, the rate of blockage of all three nerves was significantly higher in the SA group (74% vs. 40.7%, P = 0.013). Furthermore, the rate of complete sensory block of the radial nerve at 20 minutes was significantly greater in the SA group (85.2% vs. 59.3%, P = 0.033).
CONCLUSIONS
A shallow needle approach to the axillary artery resulted in a significantly higher median, radial, and ulnar nerve block rate at 20 minutes after LA injection than a perpendicular approach.
MeSH Terms
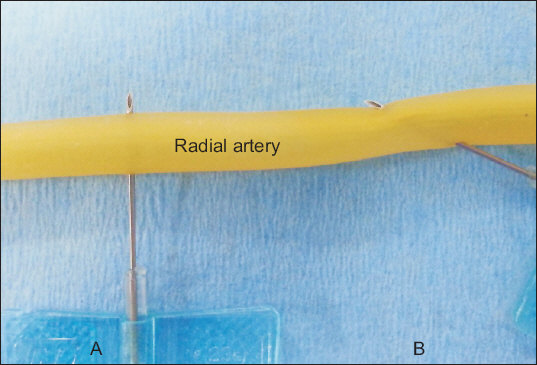
Figure
Reference
-
1. Sites BD, Beach ML, Spence BC, Wiley CW, Shiffrin J, Hartman GS, et al. Ultrasound guidance improves the success rate of a perivascular axillary plexus block. Acta Anaesthesiol Scand. 2006; 50:678–84. DOI: 10.1111/j.1399-6576.2006.01042.x. PMID: 16987361.2. Aantaa R, Kirvelä O, Lahdenperä A, Nieminen S. Transarterial brachial plexus anesthesia for hand surgery:a retrospective analysis of 346 cases. J Clin Anesth. 1994; 6:189–92. DOI: 10.1016/0952-8180(94)90057-4.3. English LA, Holmes JM, Burkard JF, Vacchiano CA, Shin A, Pellegrini J, et al. Effect of needle size on success of transarterial axillary block. AANA J. 2004; 72:57–60. PMID: 15098518.4. Vester-Andersen T, Broby-Johansen U, Bro-Rasmussen F. Perivascular axillary block VI:the distribution of gelatine solution injected into the axillary neurovascular sheath of cadavers. Acta Anaesthesiol Scand. 1986; 30:18–22. DOI: 10.1111/j.1399-6576.1986.tb02359.x. PMID: 3962570.5. Lee MG, Kim HS, Lee DC, Jung WS, Chang YJ. A comparison of general anesthesia versus axillary brachial plexus block for hand and wrist surgery in the view of patient satisfaction. Anesth Pain Med. 2014; 9:19–23.6. Sia S, Lepri A, Marchi M. Axillary block by “selective” injections at the nerves involved in surgery using a peripheral nerve stimulator:a comparison with a “standard” triple-injection technique. Reg Anesth Pain Med. 2010; 35:22–7. DOI: 10.1097/AAP.0b013e3181c6f395. PMID: 20052813.7. Retzl G, Kapral S, Greher M, Mauritz W. Ultrasonographic findings of the axillary part of the brachial plexus. Anesth Analg. 2001; 92:1271–5. DOI: 10.1097/00000539-200105000-00037. PMID: 11323361.8. Sharma R. Scalp vein set;simple and useful adjunct for pediatric nerve blocks. Paediatr Anaesth. 2010; 20:197–8. DOI: 10.1111/j.1460-9592.2009.03251.x. PMID: 20078817.9. Turan A, Kul Z, Ozyğit T, Gözü A, Ozsoy Z. Use of the scalp vein infusion set for irrigation in infections of the hand. Plast Reconstr Surg. 2004; 114:1004–5. DOI: 10.1097/01.PRS.0000138697.49718.35. PMID: 15468412.10. Danda RS, Kamath J, Jayasheelan N, Kumar P. Role of guided ultrasound in the treatment of de quervain tenosynovitis by local steroid infiltration. J Hand Microsurg. 2016; 8:34–7. DOI: 10.1055/s-0036-1581123. PMID: 27616825. PMCID: PMC5016983.11. Han JH, Kim YJ, Kim JH, Kim DY, Lee GY, Kim CH. Topographic pattern of the brachial plexus at the axillary fossa through real-time ultrasonography in Koreans. Korean J Anesthesiol. 2014; 67:310–6. DOI: 10.4097/kjae.2014.67.5.310. PMID: 25473459. PMCID: PMC4252342.12. Nowakowski P, Bieryło A. Ultrasound guided axillary brachial plexus plexus block. Part 2 - technical issues. Anaesthesiol Intensive Ther. 2015; 47:417–24. DOI: 10.5603/AIT.2015.0053. PMID: 26401747.13. Cho S, Kim YJ, Kim JH, Baik HJ. Double-injection perivascular ultrasound-guided axillary brachial plexus block according to needle positioning:12 versus 6 o'clock position of the axillary artery. Korean J Anesthesiol. 2014; 66:112–9. DOI: 10.4097/kjae.2014.66.2.112. PMID: 24624268. PMCID: PMC3948437.14. Roy M, Nadeau MJ, Côté D, Levesque S, Dion N, Nicole PC, et al. Comparison of a single- or double-injection technique for ultrasound-guided supraclavicular block:a prospective, randomized, blinded controlled study. Reg Anesth Pain Med. 2012; 37:55–9. DOI: 10.1097/AAP.0b013e3182367b97. PMID: 22030724.15. Wong MH, George A, Varma M. Ultrasound-guided perivascular axillary brachial plexus block:not so simple. Reg Anesth Pain Med. 2013; 38:167. DOI: 10.1097/AAP.0b013e31827b6750. PMID: 23423132.16. Ay S, Akinci M, Sayin M, Bektas U, Tekdemir I, Elhan A. The axillary sheath and single-injection axillary block. Clin Anat. 2007; 20:57–63. DOI: 10.1002/ca.20270. PMID: 16372345.17. Franco CD, Rahman A, Voronov G, Kerns JM, Beck RJ, Buckenmaier CC 3rd. Gross anatomy of the brachial plexus sheath in human cadavers. Reg Anesth Pain Med. 2008; 33:64–9. DOI: 10.1016/j.rapm.2007.09.003. PMID: 18155059.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Axillary and Supraclavicular Approach in Ultrasound-Guided Brachial Plexus Block
- Brachial Plexus Injury Following Axillary Brachial Plexus Block Using a Transarterial Approach: A case report
- Erratum: Effect of needle approach to the axillary artery on transarterial axillary brachial plexus block quality
- Axillary Brachial Plexus Block with Peripheral Nerve Stimulator
- Proximal Median Neuropathy Caused by Axillary Brachial Plexus Block