Investig Clin Urol.
2018 Mar;59(2):133-140. 10.4111/icu.2018.59.2.133.
Short-term outcomes of the transvaginal minimal mesh procedure for pelvic organ prolapse
- Affiliations
-
- 1Department of Urology, Juntendo University School of Medicine, Tokyo, Japan. shorie@juntendo.ac.jp
- 2Department of Urology, Yotsuya Medical Cube, Tokyo, Japan.
- 3Department of Urology, Juntendo University Urayasu Hospital, Chiba, Japan.
- KMID: 2404983
- DOI: http://doi.org/10.4111/icu.2018.59.2.133
Abstract
- PURPOSE
This study aimed to evaluate the clinical outcomes and complications of transvaginal minimal mesh repair without using commercially available kits for treatment of pelvic organ prolapse (POP).
MATERIALS AND METHODS
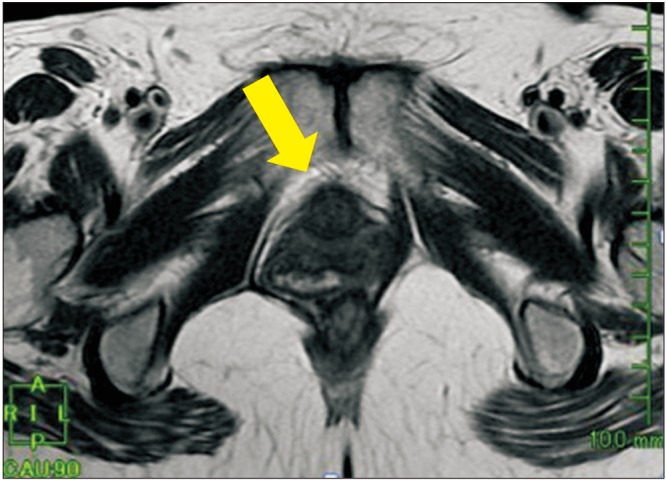
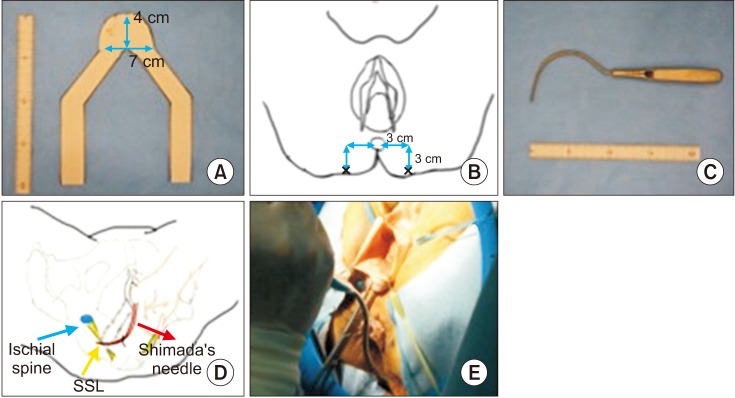
This retrospective cohort study involved 91 women who underwent surgical management of POP with originally designed small mesh between July 2014 and August 2015. This mesh is 56% smaller than the mesh widely used in Japan, and it has only two arms delivered into each right and left sacrospinous ligament. The main study outcome was the anatomic cure rate defined as recurrence of POP quantification (POP-Q) stage II or more. We also assessed changes in the overactive bladder symptom score (OABSS) and prolapse quality of life questionnaire (P-QOL) and evaluated adverse events. Finally, we compared patient backgrounds between the patients with and without recurrence.
RESULTS
Prolapse recurred in 10 of 91 patients (11.0%), and all patients with recurrence were diagnosed as POP-Q stage II. As adverse events, only mesh erosion occurred in two (2.2%) and pelvic pain in one (1.1%) of the 91 patients. The OABSS and P-QOL were significantly improved by the operation. When we compared patient backgrounds between the patients with and without recurrence, body mass index was the only factor influencing affecting recurrence.
CONCLUSIONS
Transvaginal minimal mesh repair resulted in successful outcomes with low mesh-related complications and anatomic recurrence at one year. Furthermore, significant improvement in QOL was offered by this procedure. Our minimal mesh technique should be considered as one treatment option for the management of POP.
MeSH Terms
Figure
Reference
-
1. Rogo-Gupta L, Rodriguez LV, Litwin MS, Herzog TJ, Neugut AI, Lu YS, et al. Trends in surgical mesh use for pelvic organ prolapse from 2000 to 2010. Obstet Gynecol. 2012; 120:1105–1115. PMID: 23090529.
Article2. Altman D, Väyrynen T, Engh ME, Axelsen S, Falconer C. Nordic Transvaginal Mesh Group. Anterior colporrhaphy versus transvaginal mesh for pelvic-organ prolapse. N Engl J Med. 2011; 364:1826–1836. PMID: 21561348.
Article3. Maher C, Baessler K. Surgical management of anterior vaginal wall prolapse: an evidencebased literature review. Int Urogynecol J Pelvic Floor Dysfunct. 2006; 17:195–201. PMID: 15915320.
Article4. Takeyama M. Basic procedures in tension-free vaginal mesh operation for pelvic organ prolapse. Int J Urol. 2011; 18:555–556. PMID: 21711397.
Article5. Diwadkar GB, Barber MD, Feiner B, Maher C, Jelovsek JE. Complication and reoperation rates after apical vaginal prolapse surgical repair: a systematic review. Obstet Gynecol. 2009; 113:367–373. PMID: 19155908.6. Marcus-Braun N, Bourret A, von Theobald P. Persistent pelvic pain following transvaginal mesh surgery: a cause for mesh removal. Eur J Obstet Gynecol Reprod Biol. 2012; 162:224–228. PMID: 22464208.
Article7. Hiltunen R, Nieminen K, Takala T, Heiskanen E, Merikari M, Niemi K, et al. Low-weight polypropylene mesh for anterior vaginal wall prolapse: a randomized controlled trial. Obstet Gynecol. 2007; 110:455–462. PMID: 17666627.8. Jacquetin B, Hinoul P, Gauld J, Fatton B, Rosenthal C, Clavé H, et al. Total transvaginal mesh (TVM) technique for treatment of pelvic organ prolapse: a 5-year prospective follow-up study. Int Urogynecol J. 2013; 24:1679–1686. PMID: 23563891.
Article9. Miller D, Lucente V, Babin E, Beach P, Jones P, Robinson D. Prospective clinical assessment of the transvaginal mesh technique for treatment of pelvic organ prolapse-5-year results. Female Pelvic Med Reconstr Surg. 2011; 17:139–143. PMID: 22453786.
Article10. Nieminen K, Hiltunen R, Takala T, Heiskanen E, Merikari M, Niemi K, et al. Outcomes after anterior vaginal wall repair with mesh: a randomized, controlled trial with a 3 year follow-up. Am J Obstet Gynecol. 2010; 203:235.e1–235.e8. PMID: 20494332.
Article11. Sivaslioglu AA, Unlubilgin E, Dolen I. A randomized comparison of polypropylene mesh surgery with site-specific surgery in the treatment of cystocoele. Int Urogynecol J Pelvic Floor Dysfunct. 2008; 19:467–471. PMID: 17901910.
Article12. Takahashi S, Obinata D, Sakuma T, Nagane Y, Sato K, Mochida J, et al. Tension-free vaginal mesh procedure for pelvic organ prolapse: a single-center experience of 310 cases with 1-year follow up. Int J Urol. 2010; 17:353–358. PMID: 20202001.
Article13. Altman D, Mikkola TS, Bek KM, Rahkola-Soisalo P, Gunnarsson J, Engh ME, et al. Pelvic organ prolapse repair using the Uphold™ Vaginal Support System: a 1-year multicenter study. Int Urogynecol J. 2016; 27:1337–1345. PMID: 26874525.
Article14. Rooney K, Kenton K, Mueller ER, FitzGerald MP, Brubaker L. Advanced anterior vaginal wall prolapse is highly correlated with apical prolapse. Am J Obstet Gynecol. 2006; 195:1837–1840. PMID: 17132485.
Article15. Summers A, Winkel LA, Hussain HK, DeLancey JO. The relationship between anterior and apical compartment support. Am J Obstet Gynecol. 2006; 194:1438–1443. PMID: 16579933.
Article16. Kim MS, Lee GH, Na ED, Jang JH, Kim HC. The association of pelvic organ prolapse severity and improvement in overactive bladder symptoms after surgery for pelvic organ prolapse. Obstet Gynecol Sci. 2016; 59:214–219. PMID: 27200312.
Article17. Lee DM, Ryu YW, Lee YT, Ahn SH, Han JH, Yum SH. A predictive factor in overactive bladder symptoms improvement after combined anterior vaginal wall prolapse repair: a pilot study. Korean J Urol. 2012; 53:405–409. PMID: 22741049.
Article18. Sekiguchi Y, Kinjo M, Maeda Y, Kubota Y. Reinforcement of suspensory ligaments under local anesthesia cures pelvic organ prolapse: 12-month results. Int Urogynecol J. 2014; 25:783–789. PMID: 24318563.
Article19. Abed H, Rahn DD, Lowenstein L, Balk EM, Clemons JL, Rogers RG. Systematic Review Group of the Society of Gynecologic Surgeons. Incidence and management of graft erosion, wound granulation, and dyspareunia following vaginal prolapse repair with graft materials: a systematic review. Int Urogynecol J. 2011; 22:789–798. PMID: 21424785.
Article20. Collinet P, Belot F, Debodinance P, Ha Duc E, Lucot JP, Cosson M. Transvaginal mesh technique for pelvic organ prolapse repair: mesh exposure management and risk factors. Int Urogynecol J Pelvic Floor Dysfunct. 2006; 17:315–320. PMID: 16228121.
Article21. Cespedes RD. Anterior approach bilateral sacrospinous ligament fixation for vaginal vault prolapse. Urology. 2000; 56(6 Suppl 1):70–75. PMID: 11114566.
Article22. Long CY, Lo TS, Wang CL, Wu CH, Liu CM, Su JH. Risk factors of surgical failure following transvaginal mesh repair for the treatment of pelvic organ prolapse. Eur J Obstet Gynecol Reprod Biol. 2012; 161:224–227. PMID: 22326614.
Article23. Dietz HP, Simpson JM. Levator trauma is associated with pelvic organ prolapse. BJOG. 2008; 115:979–984. PMID: 18503571.
Article24. Wong V, Shek K, Rane A, Goh J, Krause H, Dietz HP. Is levator avulsion a predictor of cystocele recurrence following anterior vaginal mesh placement? Ultrasound Obstet Gynecol. 2013; 42:230–234. PMID: 23404827.
Article25. Giri A, Hartmann KE, Hellwege JN, Velez Edwards DR, Edwards TL. Obesity and pelvic organ prolapse: a systematic review and meta-analysis of observational studies. Am J Obstet Gynecol. 2017; 217:11–26.e3. PMID: 28188775.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Outcome of posterior transvaginal mesh kit
- Vaginal Approaches Using Synthetic Mesh to Treat Pelvic Organ Prolapse
- The role of mesh and graft in pelvic reconstructive surgery
- Management of Pelvic Organ Prolapse
- Current surgical management of pelvic organ prolapse: Strategies for the improvement of surgical outcomes