Cancer Res Treat.
2015 Oct;47(4):889-896. 10.4143/crt.2013.176.
Extra-cranial Malignant Rhabdoid Tumor in Children: A Single Institute Experience
- Affiliations
-
- 1Department of Pediatrics, Seoul National University Children's Hospital, Seoul, Korea. hyshin@snu.ac.kr
- 2Cancer Research Institute, Seoul National University College of Medicine, Seoul, Korea.
- 3Department of Pathology, Seoul National University College of Medicine, Seoul, Korea.
- 4Department of Radiation Oncology, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2403409
- DOI: http://doi.org/10.4143/crt.2013.176
Abstract
- PURPOSE
Malignant rhabdoid tumor (MRT) is a rare and highly aggressive tumor that affects young children. Due to its extreme rarity, most of the available data are based on retrospective case series. To add to the current knowledge of this disease, we reviewed the patients treated for extra-cranial MRT in our institute.
MATERIALS AND METHODS
A retrospective medical record review was conducted on children treated for pathologically confirmed extra-cranial MRT at Seoul National University Children's Hospital between January 2003 and May 2013.
RESULTS
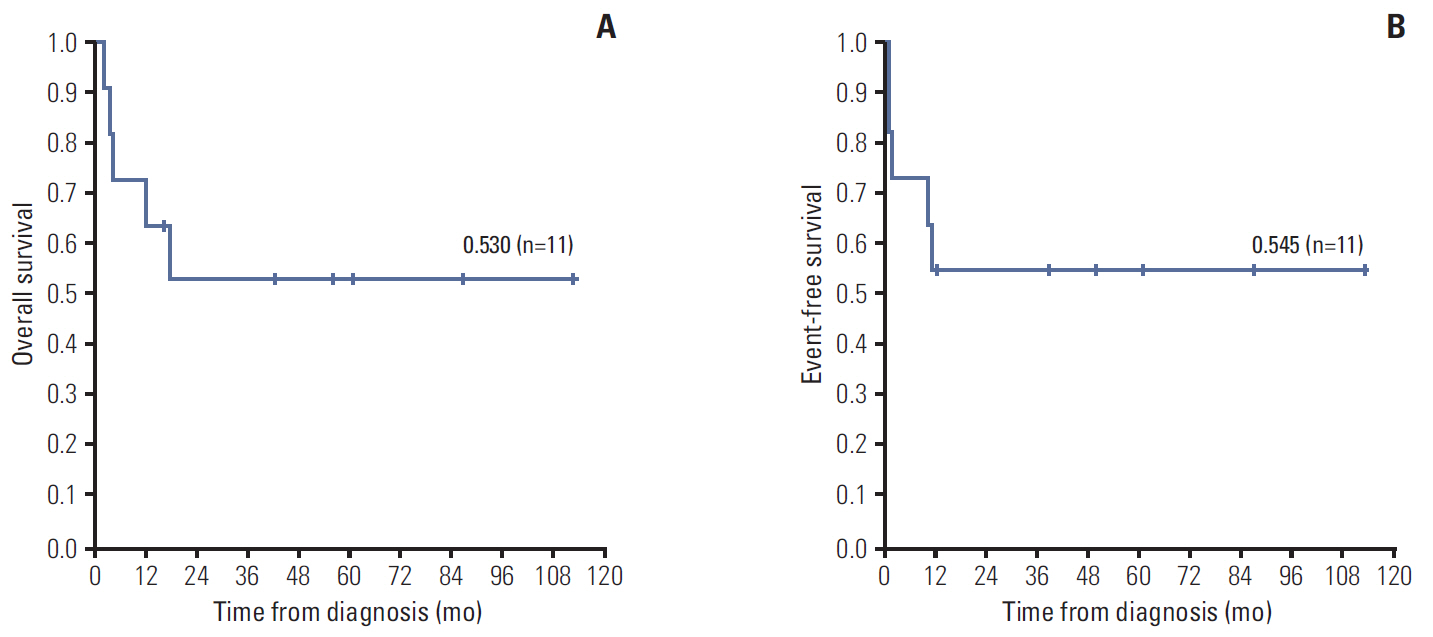
Eleven patients (7 boys, 4 girls) were diagnosed with extra-cranial MRT at a median age of 9 months old. INI1 staining was important in the pathological confirmation. Six patients (55%) had renal MRT and five (45%) had soft tissue MRT. Five patients (45%) had metastases at diagnosis. All patients underwent chemotherapy, eight patients (73%) underwent surgery, six patients (55%) received therapeutic radiotherapy, and four patients (36%) underwent high dose chemotherapy with autologous stem cell rescue (HDCT/ASCR) with melphalan, etoposide, and carboplatin. Five patients (45%) died of disease following progression (n=3) or relapse (n=2), however, there was no treatment related mortality. The overall survival of the cohort was 53.0% and the event-free survival was 54.5% with a median follow-up duration of 17.8 months (range, 2.3 to 112.3 months).
CONCLUSION
Extra-cranial MRT is still a highly aggressive tumor in young children. However, the improved survival of our cohort is promising and HDCT/ASCR with melphalan, etoposide, and carboplatin may be a promising treatment option.
MeSH Terms
Figure
Reference
-
References
1. Kerl K, Holsten T, Fruhwald MC. Rhabdoid tumors: clinical approaches and molecular targets for innovative therapy. Pediatr Hematol Oncol. 2013; 30:587–604.
Article2. Beckwith JB, Palmer NF. Histopathology and prognosis of Wilms tumors: results from the First National Wilms' Tumor Study. Cancer. 1978; 41:1937–48.3. Tsuneyoshi M, Daimaru Y, Hashimoto H, Enjoji M. Malignant soft tissue neoplasms with the histologic features of renal rhabdoid tumors: an ultrastructural and immunohistochemical study. Hum Pathol. 1985; 16:1235–42.
Article4. Rorke LB, Packer RJ, Biegel JA. Central nervous system atypical teratoid/rhabdoid tumors of infancy and childhood: definition of an entity. J Neurosurg. 1996; 85:56–65.
Article5. Biegel JA, Zhou JY, Rorke LB, Stenstrom C, Wainwright LM, Fogelgren B. Germ-line and acquired mutations of INI1 in atypical teratoid and rhabdoid tumors. Cancer Res. 1999; 59:74.6. Oda Y, Tsuneyoshi M. Extrarenal rhabdoid tumors of soft tissue: clinicopathological and molecular genetic review and distinction from other soft-tissue sarcomas with rhabdoid features. Pathol Int. 2006; 56:287–95.
Article7. Hoot AC, Russo P, Judkins AR, Perlman EJ, Biegel JA. Immunohistochemical analysis of hSNF5/INI1 distinguishes renal and extra-renal malignant rhabdoid tumors from other pediatric soft tissue tumors. Am J Surg Pathol. 2004; 28:1485–91.
Article8. Versteege I, Sevenet N, Lange J, Rousseau-Merck MF, Ambros P, Handgretinger R, et al. Truncating mutations of hSNF5/INI1 in aggressive paediatric cancer. Nature. 1998; 394:203–6.
Article9. Morgenstern DA, Gibson S, Brown T, Sebire NJ, Anderson J. Clinical and pathological features of paediatric malignant rhabdoid tumours. Pediatr Blood Cancer. 2010; 54:29–34.
Article10. Madigan CE, Armenian SH, Malogolowkin MH, Mascarenhas L. Extracranial malignant rhabdoid tumors in childhood: the Childrens Hospital Los Angeles experience. Cancer. 2007; 110:2061–6.11. Sultan I, Qaddoumi I, Rodriguez-Galindo C, Nassan AA, Ghandour K, Al-Hussaini M. Age, stage, and radiotherapy, but not primary tumor site, affects the outcome of patients with malignant rhabdoid tumors. Pediatr Blood Cancer. 2010; 54:35–40.
Article12. Reinhard H, Reinert J, Beier R, Furtwangler R, Alkasser M, Rutkowski S, et al. Rhabdoid tumors in children: prognostic factors in 70 patients diagnosed in Germany. Oncol Rep. 2008; 19:819–23.
Article13. Horazdovsky R, Manivel JC, Cheng EY. Surgery and actinomycin improve survival in malignant rhabdoid tumor. Sarcoma. 2013; 2013:315170.
Article14. Kato M, Koh K, Oshima K, Oguma E, Uchida H, Kishimoto H, et al. Long-term survivor of relapsed stage IV malignant rhabdoid tumor of the kidney. Pediatr Int. 2013; 55:245–8.
Article15. Wagner L, Hill DA, Fuller C, Pedrosa M, Bhakta M, Perry A, et al. Treatment of metastatic rhabdoid tumor of the kidney. J Pediatr Hematol Oncol. 2002; 24:385–8.
Article16. Yamamoto M, Suzuki N, Hatakeyama N, Mizue N, Hori T, Kuroiwa Y, et al. Treatment of stage IV malignant rhabdoid tumor of the kidney (MRTK) with ICE and VDCy: a case report. J Pediatr Hematol Oncol. 2006; 28:286–9.17. Koga Y, Matsuzaki A, Suminoe A, Hatano M, Saito Y, Kinoshita Y, et al. Long-term survival after autologous peripheral blood stem cell transplantation in two patients with malignant rhabdoid tumor of the kidney. Pediatr Blood Cancer. 2009; 52:888–90.
Article18. Tomlinson GE, Breslow NE, Dome J, Guthrie KA, Norkool P, Li S, et al. Rhabdoid tumor of the kidney in the National Wilms' Tumor Study: age at diagnosis as a prognostic factor. J Clin Oncol. 2005; 23:7641–5.
Article19. Sajedi M, Wolff JE, Egeler RM, Pinto A, Hughes R, Anderson RA, et al. Congenital extrarenal non-central nervous system malignant rhabdoid tumor. J Pediatr Hematol Oncol. 2002; 24:316–20.
Article20. Green DM, Breslow NE, Beckwith JB, Finklestein JZ, Grundy PE, Thomas PR, et al. Comparison between single-dose and divided-dose administration of dactinomycin and doxorubicin for patients with Wilms' tumor: a report from the National Wilms' Tumor Study Group. J Clin Oncol. 1998; 16:237–45.
Article