Kosin Med J.
2017 Dec;32(2):269-276. 10.7180/kmj.2017.32.2.269.
Imaging of F-18 FDG PET/CT and follow up of bilateral invasive adrenal diffuse large B cell lymphoma mimicking adrenocortical carcinoma
- Affiliations
-
- 1Department of Nuclear Medicine, Inje University Haeundae Paik Hospital, Busan, Korea. Shimhk80@naver.com
- 2Department of Pathology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 2400273
- DOI: http://doi.org/10.7180/kmj.2017.32.2.269
Abstract
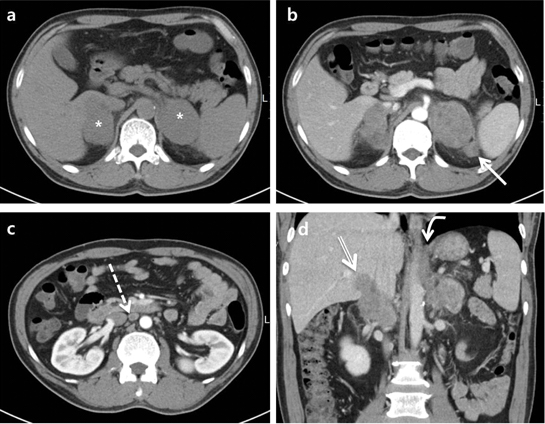
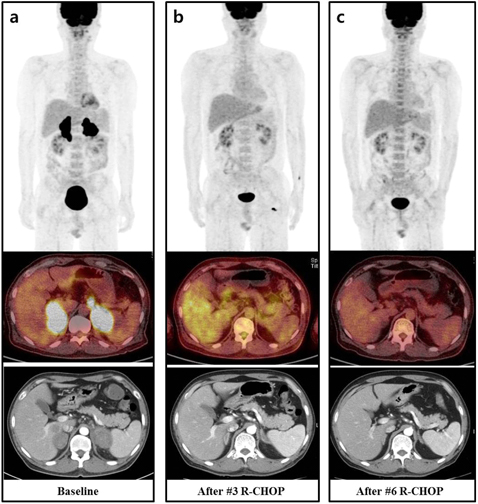
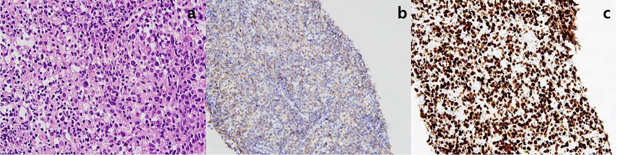
- The incidence of malignant adrenal tumors, including primary adrenal lymphoma (PAL) and adrenocortical carcinoma (ACC), is rather low. Early differentiation between ACC and PAL is necessary because the therapeutic strategies for the two differ and the prognosis of each disease is poor. Unfortunately, there is no pathognomonic characteristic of PAL, so radiologists have difficulty in differentiating it from ACC. To our knowledge, there have been only two case reports on ACC that was evaluated and followed up using F-18 FDG PET/CT. The previously reported cases were simple, involving only the bilateral adrenal glands. Here, we report on a 52-year-old man diagnosed with PAL that radiologically mimicked ACC. He had findings of heterogeneous enhancement on CT, several adjacent lymphadenopathies with internal necrosis, and abutting hepatic and bilateral crural invasion. After pathological confirmation, we monitored his prognosis using F-18 FDG PET/CT after three cycles of rituximab-CHOP and again after six cycles of treatment.
MeSH Terms
Figure
Reference
-
1. Luton JP, Cerdas S, Billaud L, Thomas G, Guilhaume B, Bertagna X, et al. Clinical features of adrenocortical carcinoma, prognostic factors, and the effect of mitotane therapy. N Engl J Med. 1990; 322:1195–1201.
Article2. Kim KM, Yoon DH, Lee SG, Lim SN, Sug LJ, Huh J, et al. A case of primary adrenal diffuse large B-cell lymphoma achieving complete remission with rituximab-CHOP chemotherapy. J Korean Med Sci. 2009; 24:525–528.
Article3. Wang J, Sun NC, Renslo R, Chuang CC, Tabbarah HJ, Barajas L, et al. Clinically silent primary adrenal lymphoma: a case report and review of the literature. Am J Hematol. 1998; 58:130–136.
Article4. Grigg AP, Connors JM. Primary adrenal lymphoma. Clin Lymphoma. 2003; 4:154–160.
Article5. Kuyama A, Takeuchi M, Munemasa M, Tsutsui K, Aga N, Goda Y, et al. Successful treatment of primary adrenal non-Hodgkin's lymphoma associated with adrenal insufficiency. Leuk Lymphoma. 2000; 38:203–205.
Article6. Ozimek A, Diebold J, Linke R, Heyn J, Hallfeldt K, Mussack T. Bilateral primary adrenal non-Hodgkin's lymphoma and primary adrenocortical carcinoma--review of the literature preoperative differentiation of adrenal tumors. Endocr J. 2008; 55:625–638.
Article7. Dong A, Cui Y, Wang Y, Zuo C, Bai Y. (18)F-FDG PET/CT of adrenal lesions. AJR Am J Roentgenol. 2014; 203:245–252.
Article8. Bharwani N, Rockall AG, Sahdev A, Gueorguiev M, Drake W, Grossman AB, et al. Adrenocortical carcinoma: the range of appearances on CT and MRI. AJR Am J Roentgenol. 2011; 196:W706–W714.
Article9. Lyon SM, Lee MJ. Imaging the non-hyperfunctioning adrenal mass. Imaging. 2002; 14:137–146.
Article10. Deandreis D, Leboulleux S, Caramella C, Schlumberger M, Baudin E. FDG PET in the management of patients with adrenal masses and adrenocortical carcinoma. Horm Cancer. 2011; 2:354–362.
Article11. Paling MR, Williamson BR. Adrenal involvement in non-Hodgkin lymphoma. AJR Am J Roentgenol. 1983; 141:303–305.
Article12. Rashidi A, Fisher SI. Primary adrenal lymphoma: a systematic review. Ann Hematol. 2013; 92:1583–1593.
Article13. Parameswaran R, Chan DKH, Michelle PLM, Wang S. Primary Adrenal Diffuse Large B-cell Lymphoma: A Mini Review. World J Endoc Surg. 2015; 7:65–68.
Article14. Kumar R, Xiu Y, Mavi A, El-Haddad G, Zhuang H, Alavi A. FDG-PET imaging in primary bilateral adrenal lymphoma: a case report and review of the literature. Clin Nucl Med. 2005; 30:222–230.
Article15. Leboulleux S, Dromain C, Bonniaud G, Aupérin A, Caillou B, Lumbroso J, et al. Diagnostic and prognostic value of 18-fluorodeoxyglucose positron emission tomography in adrenocortical carcinoma: a prospective comparison with computed tomography. J Clin Endocrinol Metab. 2006; 91:920–925.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Primary Hepatosplenic B-cell Lymphoma: Iinitial Diagnosis and Assessment of Therapeutic Response with F-18 FDG PET/CT
- Peritoneal Lymphomatosis Imaged by F-18 FDG PET/CT
- Unusual Presentation of Bilateral Adrenocortical Carcinoma Mimicking Adrenal Metastasis
- Diffuse Bone Marrow Uptake of 99mTc-MIBI in A Case of Intravascular Large B-cell Lymphoma
- F-18 FDG PET/CT Findings of Subcutaneous Panniculitis - Like T- Cell Lymphoma : A Case Report