Investig Clin Urol.
2018 Jan;59(1):38-43. 10.4111/icu.2018.59.1.38.
Can feeling of incomplete bladder emptying reflect significant postvoid residual urine? Is it reliable as a symptom solely?
- Affiliations
-
- 1Urology Clinic, Denizli State Hospital, Denizli, Turkey. yusufozlu35@hotmail.com
- 2Urology Clinic, Özel Sağlık Hospital, Denizli, Turkey.
- 3Department of Urology, Pamukkale University School of Medicine, Denizli, Turkey.
- 4Urology Clinic, Acıpayam State Hospital, Denizli, Turkey.
- KMID: 2399263
- DOI: http://doi.org/10.4111/icu.2018.59.1.38
Abstract
- PURPOSE
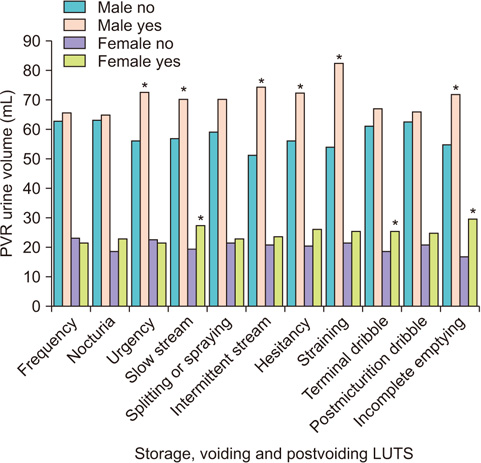
The main objective of this study was to reveal the relationship between lower urinary tract symptoms (LUTS) and post-void residual (PVR) urine volume.
MATERIALS AND METHODS
Between October 2014 and February 2015, older than 40 years patients were included in this study. Volunteers filled out a questionnaire consisted of demographic characteristics, comorbidities, medications, history of surgery and LUTS. Volunteers were undergone PVR measurement with transabdominal ultrasonography. The relationship between symptoms, demographic characteristics and PVR were analyzed.
RESULTS
A total of 939 patients (756 men and 183 women) were enrolled in this study. There was a positive correlation between the sensation of incomplete bladder emptying and PVR volume in all age groups of women (p=0.0001). However such a relationship was found only over the age of 60 in the subgroup analysis of men (p=0.001). PVR volume increased in men by age (0.65 mL per year of age, p=0.011). In men, voiding symptoms and urgency were associated with a high PVR volume. In women, storage and voiding symptoms (except slow stream and terminal dribble) did not correlate with PVR volume.
CONCLUSIONS
Our study showed that all men over the age of 60 years and all women with the complaint of feeling of incomplete emptying should undergone PVR measurement. Women with the complaint of poor stream and men mainly with voiding symptoms are other candidates in whom PVR measurement would be considered as an important tool in the clinical management and follow-up.
MeSH Terms
Figure
Reference
-
1. Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn. 2002; 21:167–178.
Article2. Nitti VW. Urodynamics and video-urodynamic evaluation of the lower urinary tract. In : Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Campell-Walsh urology tenth edition. 10th ed. Philedelphia, PA: Elsevier Saunders;2012. p. 1847–1855.3. Stern JA, Hsieh YC, Schaeffer AJ. Residual urine in an elderly female population: novel implications for oral estrogen replacement and impact on recurrent urinary tract infection. J Urol. 2004; 171:768–770.
Article4. Truzzi JC, Almeida FM, Nunes EC, Sadi MV. Residual urinary volume and urinary tract infection--when are they linked? J Urol. 2008; 180:182–185.
Article5. Kaplan SA, Wein AJ, Staskin DR, Roehrborn CG, Steers WD. Urinary retention and post-void residual urine in men: separating truth from tradition. J Urol. 2008; 180:47–54.
Article6. Rule AD, Jacobson DJ, McGree ME, Girman CJ, Lieber MM, Jacobsen SJ. Longitudinal changes in post-void residual and voided volume among community dwelling men. J Urol. 2005; 174:1317–1321. discussion 1321-2; author reply 1322.
Article7. Negro CL, Muir GH. Chronic urinary retention in men: how we define it, and how does it affect treatment outcome. BJU Int. 2012; 110:1590–1594.
Article8. Kelly CE. Evaluation of voiding dysfunction and measurement of bladder volume. Rev Urol. 2004; 6:Suppl 1. S32–S37.9. Abdelwahab HA, Abdalla HM, Sherief MH, Ibrahim MB, Shamaa MA. The reliability and reproducibility of ultrasonography for measuring the residual urine volume in men with lower urinary tract symptoms. Arab J Urol. 2014; 12:285–289.
Article10. Cayetano-Alcaraz AA, Herrera-Cáceres JO, García-Mora A. The relationship between the sensation of incomplete voiding and a high postvoid residual volume. Actas Urol Esp. 2016; 40:309–316.
Article11. Zumrutbas AE, Bozkurt AI, Tas E, Acar CI, Alkis O, Coban K, et al. Prevalence of lower urinary tract symptoms, overactive bladder and urinary incontinence in western Turkey: results of a population-based survey. Int J Urol. 2014; 21:1027–1033.
Article12. Dietz HP, Haylen BT. Symptoms of voiding dysfunction: what do they really mean? Int Urogynecol J Pelvic Floor Dysfunct. 2005; 16:52–55. discussion 55.
Article13. Jeffery ST, Doumouchtsis SK, Vlachos IS, Fynes MM. Are voiding symptoms really associated with abnormal urodynamic voiding parameters in women? Int J Urol. 2008; 15:1044–1048.
Article14. Groutz A, Gordon D, Lessing JB, Wolman I, Jaffa A, David MP. Prevalence and characteristics of voiding difficulties in women: are subjective symptoms substantiated by objective urodynamic data? Urology. 1999; 54:268–272.
Article15. Lowenstein L, Anderson C, Kenton K, Dooley Y, Brubaker L. Obstructive voiding symptoms are not predictive of elevated postvoid residual urine volumes. Int Urogynecol J Pelvic Floor Dysfunct. 2008; 19:801–804.
Article16. Al-Zahrani AA, Gajewski JB. Association of symptoms with urodynamic findings in men with overactive bladder syndrome. BJU Int. 2012; 110:E891–E895.
Article17. Chung SD, Liao CH, Chen YC, Kuo HC. Urgency severity scale could predict urodynamic detrusor overactivity in patients with overactive bladder syndrome. Neurourol Urodyn. 2011; 30:1300–1304.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Usefulness of Residual Urine Fraction and Maximal Flow Rate for Predicting Outcome after Transurethral Resection of Prostate in Benign Prostatic Hyperplasia
- Clinical Factors Associated With the Feeling of Incomplete Bladder Emptying in Women With Little Postvoided Residue
- Ovarian Cystadenoma Mistaken as Postvoid Residual Urine by Portable Ultrasound Scanning
- Definition and symptoms of underactive bladder
- Preoperative Detrusor Contractile Strength Measurement in the BPH Patients with Residual Urine