Investig Clin Urol.
2017 Dec;58(Suppl 2):S61-S67. 10.4111/icu.2017.58.S2.S61.
Definition and symptoms of underactive bladder
- Affiliations
-
- 1Bristol Urological Institute, Southmead Hospital, Bristol, UK. Alan.uren@bui.ac.uk
- 2University of Bristol, Bristol, UK.
- KMID: 2397981
- DOI: http://doi.org/10.4111/icu.2017.58.S2.S61
Abstract
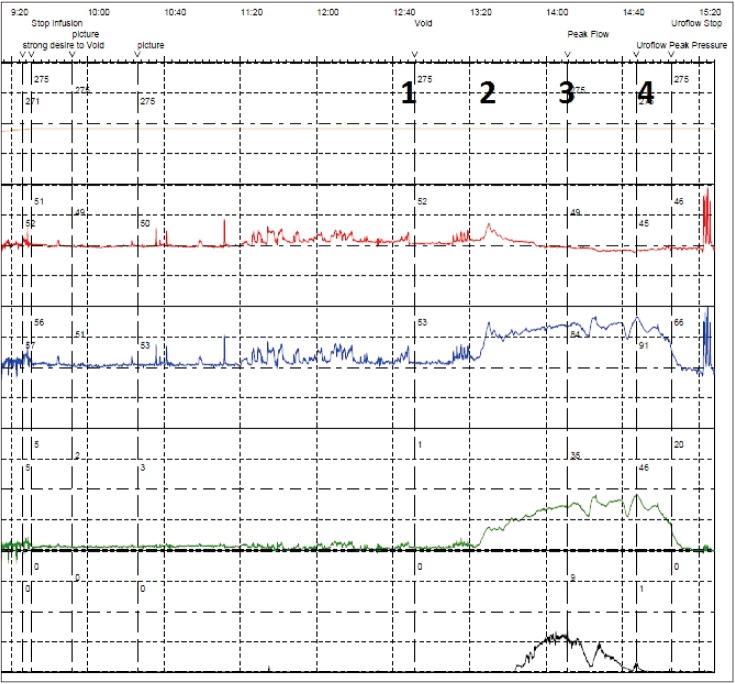
- Underactive bladder (UAB) is a symptom syndrome reflecting the urodynamic observation of detrusor underactivity (DU), a voiding contraction of reduced strength and/or duration, leading to prolonged or incomplete bladder emptying. An International Continence Society Working Group has described UAB as characterised by a slow urinary stream, hesitancy and straining to void, with or without a feeling of incomplete bladder emptying and dribbling, often with storage symptoms. Since DU often coexists with bladder outlet obstruction, or storage dysfunction (detrusor overactivity or incontinence), the exact contribution of the DU to the presenting complaints can be difficult to establish. The presence of voiding and post voiding lower urinary tract symptoms (LUTS) is implicitly expected in UAB, but a reduced sensation of fullness is reported by some patients, and storage LUTS are also an important factor in many affected patients. These may result from a postvoid residual, but often they do not. The storage LUTS are often the key driver in leading the patient to seek healthcare input. Nocturia is particularly common and bothersome, but what the role of DU is in all the range of influences on nocturia has not been established. Qualitative research has established a broad impact on everyday life as a result of these symptoms. In general, people appear to manage the voiding LUTS relatively well, but the storage LUTS may be problematic.
Keyword
MeSH Terms
Figure
Reference
-
1. Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Urology. 2003; 61:37–49. PMID: 12559262.
Article2. Wein AJ, Rovner ES. Definition and epidemiology of overactive bladder. Urology. 2002; 60(5 Suppl 1):7–12. discussion 12.
Article3. Chapple CR, Osman NI, Birder L, van Koeveringe GA, Oelke M, Nitti VW, et al. The underactive bladder: a new clinical concept? Eur Urol. 2015; 68:351–353. PMID: 25770481.
Article4. Osman NI, Chapple CR, Abrams P, Dmochowski R, Haab F, Nitti V, et al. Detrusor underactivity and the underactive bladder: a new clinical entity? A review of current terminology, definitions, epidemiology, aetiology, and diagnosis. Eur Urol. 2014; 65:389–398. PMID: 24184024.
Article5. Birder L, de Groat W, Mills I, Morrison J, Thor K, Drake M. Neural control of the lower urinary tract: peripheral and spinal mechanisms. Neurourol Urodyn. 2010; 29:128–139. PMID: 20025024.
Article6. Drake MJ, Fowler CJ, Griffiths D, Mayer E, Paton JFR, Birder L. Neural control of the lower urinary and gastrointestinal tracts: supraspinal CNS mechanisms. Neurourol Urodyn. 2010; 29:119–127. PMID: 20025025.
Article7. Drake MJ. The integrative physiology of the bladder. Ann R Coll Surg Engl. 2007; 89:580–585. PMID: 18201471.
Article8. Hoag N, Gani J. Underactive bladder: clinical features, urodynamic parameters, and treatment. Int Neurourol J. 2015; 19:185–189. PMID: 26620901.
Article9. Jeong SJ, Kim HJ, Lee YJ, Lee JK, Lee BK, Choo YM, et al. Prevalence and clinical features of detrusor underactivity among elderly with lower urinary tract symptoms: a comparison between men and women. Korean J Urol. 2012; 53:342–348. PMID: 22670194.
Article10. Resnick NM, Yalla SV. Detrusor hyperactivity with impaired contractile function. An unrecognized but common cause of incontinence in elderly patients. JAMA. 1987; 257:3076–3081. PMID: 3586227.
Article11. Miyazato M, Yoshimura N, Chancellor MB. The other bladder syndrome: underactive bladder. Rev Urol. 2013; 15:11–22. PMID: 23671401.12. van Koeveringe GA, Vahabi B, Andersson KE, Kirschner-Herrmans R, Oelke M. Detrusor underactivity: a plea for new approaches to a common bladder dysfunction. Neurourol Urodyn. 2011; 30:723–728. PMID: 21661020.
Article13. van Koeveringe GA, Rademakers KL, Birder LA, Korstanje C, Daneshgari F, Ruggieri MR, et al. Detrusor underactivity: pathophysiological considerations, models and proposals for future research. ICI-RS 2013. Neurourol Urodyn. 2014; 33:591–596. PMID: 24839258.
Article14. Smith PP. Aging and the underactive detrusor: a failure of activity or activation? Neurourol Urodyn. 2010; 29:408–412. PMID: 19760756.
Article15. Uren AD, Cotterill N, Harding C, Hillary C, Chapple C, Klaver M, et al. Qualitative exploration of the patient experience of underactive bladder. Eur Urol. 2017; 72:402–407. PMID: 28400168.
Article16. Gammie A, Kaper M, Dorrepaal C, Kos T, Abrams P. Signs and symptoms of detrusor underactivity: an analysis of clinical presentation and urodynamic tests from a large group of patients undergoing pressure flow studies. Eur Urol. 2016; 69:361–369. PMID: 26318706.
Article17. Fode M, Sønksen J. Towards a greater understanding of underactive bladder. Eur Urol. 2017; 72:408–409. PMID: 28456349.
Article18. Dewulf K, Abraham N, Lamb LE, Griebling TL, Yoshimura N, Tyagi P, et al. Addressing challenges in underactive bladder: recommendations and insights from the Congress on Underactive Bladder (CURE-UAB). Int Urol Nephrol. 2017; 49:777–785. PMID: 28233085.
Article19. Chapple CR, Osman NI. Crystallizing the definition of underactive bladder syndrome, a common but under-recognized clinical entity. Low Urin Tract Symptoms. 2015; 7:71–76. PMID: 26663685.
Article20. Wein A, Chapple C. Introduction and terminology. In : Chapple C, Wein A, Osman N, editors. Underactive bladder. Switzerland: Springer;2017. p. ix–xiii.21. Drake MJ. Should nocturia not be called a lower urinary tract symptom? Eur Urol. 2015; 67:289–290. PMID: 25277270.
Article22. Gulur DM, Mevcha AM, Drake MJ. Nocturia as a manifestation of systemic disease. BJU Int. 2011; 107:702–713. PMID: 21355977.
Article23. Coyne KS, Sexton CC, Kopp Z, Chapple CR, Kaplan SA, Aiyer LP, et al. Assessing patients' descriptions of lower urinary tract symptoms (LUTS) and perspectives on treatment outcomes: results of qualitative research. Int J Clin Pract. 2010; 64:1260–1278. PMID: 20579138.
Article24. Gannon K, Glover L, O'Neill M, Emberton M. Men and chronic illness: a qualitative study of LUTS. J Health Psychol. 2004; 9:411–420. PMID: 15117540.
Article25. Glover L, Gannon K, McLoughlin J, Emberton M. Men's experiences of having lower urinary tract symptoms: factors relating to bother. BJU Int. 2004; 94:563–567. PMID: 15329113.
Article26. Wareing M. Lower urinary tract symptoms: a hermeneutic phenomenological study into men’s lived experience. J Clin Nurs. 2005; 14:239–246. PMID: 15669933.
Article27. Coyne KS, Wein AJ, Tubaro A, Sexton CC, Thompson CL, Kopp ZS, et al. The burden of lower urinary tract symptoms: evaluating the effect of LUTS on health-related quality of life, anxiety and depression: EpiLUTS. BJU Int. 2009; 103(Suppl 3):4–11.
Article28. Osman N, Hillary C, Chapple C. Epidemiology of underactive bladder. In : Chapple C, Wein A, Osman N, editors. Underactive bladder. Switzerland: Springer;2017. p. 25–31.29. Abarbanel J, Marcus EL. Impaired detrusor contractility in community-dwelling elderly presenting with lower urinary tract symptoms. Urology. 2007; 69:436–440. PMID: 17382138.
Article30. Drake MJ, Kanai A, Bijos DA, Ikeda Y, Zabbarova I, Vahabi B, et al. The potential role of unregulated autonomous bladder micromotions in urinary storage and voiding dysfunction; overactive bladder and detrusor underactivity. BJU Int. 2017; 119:22–29. PMID: 27444952.
Article31. Cho MC, Ha SB, Park J, Son H, Oh SJ, Kim SW, et al. Impact of detrusor underactivity on surgical outcomes of laser prostatectomy: comparison in serial 12-month follow-up outcomes between potassium-titanyl-phosphate photoselective vaporization of the prostate (PVP) and holmium laser enucleation of the prostate (HoLEP). Urology. 2016; 91:158–166. PMID: 26879733.
Article32. Uren AD, Cotterill N, Harding C, Hillary C, Chapple C, Klaver M, et al. Qualitative development of a new patient reported outcome measure for underactive bladder. In : International Continence Society 2016 Tokyo; 2016 Sep 13-16; Tokyo, Japan. Available from: https://www.ics.org/Abstracts/Publish/326/000075.pdf.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Origin of Urgency Symptom in Underactive Bladder: Commentary on "Underactive Bladder: Clinical Features, Urodynamic Parameters, and Treatment" (Int Neurourol J 2015;19:185-9)
- Clinical implications of underactive bladder
- Underactive Bladder; Review of Progress and Impact From the International CURE-UAB Initiative
- Epidemiology of underactive bladder: Common but underresearched
- New therapeutic directions to treat underactive bladder