J Gastric Cancer.
2017 Dec;17(4):319-330. 10.5230/jgc.2017.17.e36.
Extensive Lymph Node Dissection Improves Survival among American Patients with Gastric Adenocarcinoma Treated Surgically: Analysis of the National Cancer Database
- Affiliations
-
- 1Department of General Surgery, University of Illinois Hospital and Health Sciences System, Chicago, IL, USA. snaffouj@uic.edu
- 2Department of Surgical Oncology, Edward Cancer Center, Naperville, IL, USA.
- 3Division of Surgical Oncology, University of Illinois Hospital and Health Sciences System, Chicago, IL, USA.
- KMID: 2398798
- DOI: http://doi.org/10.5230/jgc.2017.17.e36
Abstract
- INTRODUCTION
The extent of lymphadenectomy in the surgical treatment of gastric cancer is a topic of controversy among surgeons. This study was conducted to analyze the American National Cancer Database (NCDB) and conclude the optimal extent of lymphadenectomy for gastric adenocarcinoma.
METHODS
The NCDB for gastric cancer was utilized. Patients who received at least a partial gastrectomy were included. Patients with metastatic disease, unknown TNM stages, R1/R2 resection, or treated with a palliative intent were excluded. Joinpoint regression was used to identify the extent of lymphadenectomy that reflects the optimal survival. Cox regression analysis and Bayesian information criterion were used to identify significant survival predictors. Kaplan-Meier was applied to study overall survival and stage migration.
RESULTS
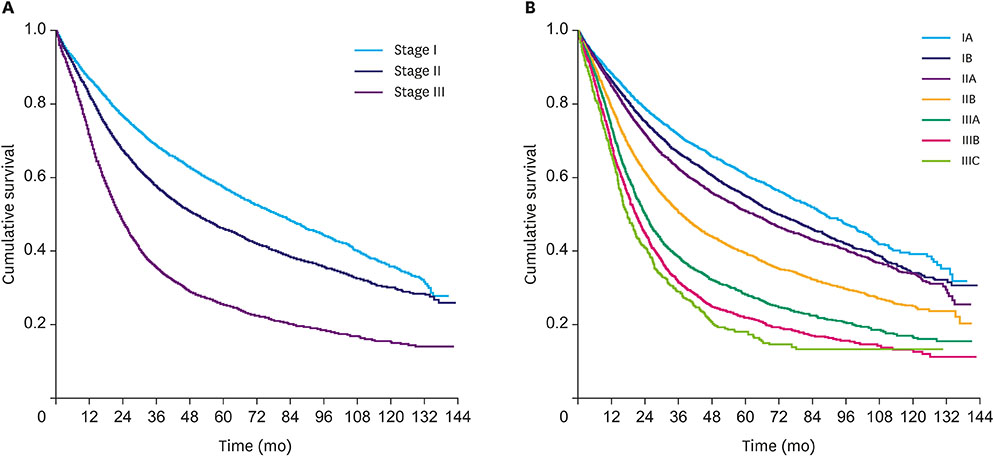
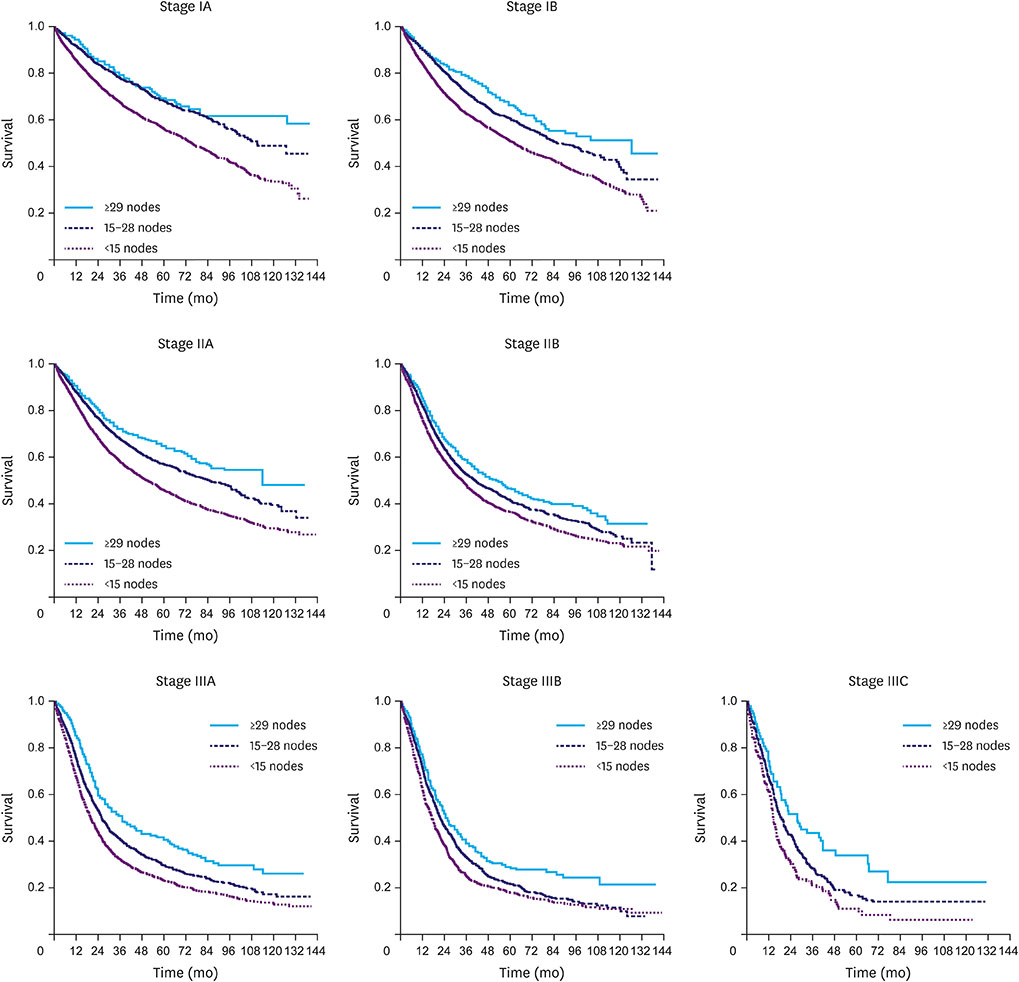
40,281 patients of 168,377 met the inclusion criteria. Joinpoint analysis showed that dissection of 29 nodes provides the optimal median survival for the overall population. Regression analysis reported the cutoff ≥29 to have a better fit in the prognostic model than that of ≥15. Dissection of ≥29 nodes in the higher stages provides a comparable overall survival to the immediately lower stage. Nonetheless, the retrieval of ≥15 nodes proved to be adequate for staging without a significant stage migration compared to ≥29 nodes.
CONCLUSION
The extent of lymphadenectomy in gastric adenocarcinoma is a marker of improved resection which reflects in a longer overall survival. Our analysis concludes that the dissection of ≥15 nodes is adequate for staging. However, the dissection of 29 nodes might be needed to provide a significantly improved survival.
Keyword
MeSH Terms
Figure
Reference
-
1. Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011; 61:69–90.2. Lin Y, Ueda J, Kikuchi S, Totsuka Y, Wei WQ, Qiao YL, et al. Comparative epidemiology of gastric cancer between Japan and China. World J Gastroenterol. 2011; 17:4421–4428.3. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin. 2016; 66:7–30.4. International Agency for Research on Cancer. World Health Organization. GLOBOCAN 2012: estimated cancer incidence, mortality and prevalence worldwide in 2012 [Internet]. Lyon: International Agency for Research on Cancer;2014. cited 2017 Oct 20. Available from: http://globocan.iarc.fr.5. Jung KW, Won YJ, Kong HJ, Oh CM, Seo HG, Lee JS. Prediction of cancer incidence and mortality in Korea, 2013. Cancer Res Treat. 2013; 45:15–21.6. Wu CW, Hsiung CA, Lo SS, Hsieh MC, Chen JH, Li AF, et al. Nodal dissection for patients with gastric cancer: a randomised controlled trial. Lancet Oncol. 2006; 7:309–315.7. Maruyama K, Okabayashi K, Kinoshita T. Progress in gastric cancer surgery in Japan and its limits of radicality. World J Surg. 1987; 11:418–425.8. de Aretxabala X, Konishi K, Yonemura Y, Ueno K, Yagi M, Noguchi M, et al. Node dissection in gastric cancer. Br J Surg. 1987; 74:770–773.9. Cuschieri A, Fayers P, Fielding J, Craven J, Bancewicz J, Joypaul V, et al. Postoperative morbidity and mortality after D1 and D2 resections for gastric cancer: preliminary results of the MRC randomised controlled surgical trial. The Surgical Cooperative Group. Lancet. 1996; 347:995–999.10. Bonenkamp JJ, Songun I, Hermans J, Sasako M, Welvaart K, Plukker JT, et al. Randomised comparison of morbidity after D1 and D2 dissection for gastric cancer in 996 Dutch patients. Lancet. 1995; 345:745–748.11. National Comprehensive Cancer Network (US). NCCN Clinical Practice Guidelines in Oncology. Gastric Cancer, Version 3. 2016. Fort Washington (PA): National Comprehensive Cancer Network;2016.12. Wang J, Dang P, Raut CP, Pandalai PK, Maduekwe UN, Rattner DW, et al. Comparison of a lymph node ratio-based staging system with the 7th AJCC system for gastric cancer: analysis of 18,043 patients from the SEER database. Ann Surg. 2012; 255:478–485.13. Bunt AM, Hermans J, Smit VT, van de Velde CJ, Fleuren GJ, Bruijn JA. Surgical/pathologic-stage migration confounds comparisons of gastric cancer survival rates between Japan and Western countries. J Clin Oncol. 1995; 13:19–25.14. Putchakayala K, Difronzo LA. D2 lymph node dissection improves staging in patients with gastric adenocarcinoma. Am Surg. 2011; 77:1326–1329.15. American Cancer Society. Survival Rates for Stomach Cancer, by Stage. Atlanta (GA): American Cancer Society;2016.16. Lee HK, Yang HK, Kim WH, Lee KU, Choe KJ, Kim JP. Influence of the number of lymph nodes examined on staging of gastric cancer. Br J Surg. 2001; 88:1408–1412.17. Siewert JR, Böttcher K, Stein HJ, Roder JD. Relevant prognostic factors in gastric cancer: ten-year results of the German Gastric Cancer Study. Ann Surg. 1998; 228:449–461.18. Yu W, Choi GS, Chung HY. Randomized clinical trial of splenectomy versus splenic preservation in patients with proximal gastric cancer. Br J Surg. 2006; 93:559–563.19. Biffi R, Chiappa A, Luca F, Pozzi S, Lo Faso F, Cenciarelli S, et al. Extended lymph node dissection without routine spleno-pancreatectomy for treatment of gastric cancer: low morbidity and mortality rates in a single center series of 250 patients. J Surg Oncol. 2006; 93:394–400.20. Uyama I, Ogiwara H, Takahara T, Kikuchi K, Iida S, Kubota T, et al. Spleen- and pancreas-preserving total gastrectomy with superextended lymphadenectomy including dissection of the para-aortic lymph nodes for gastric cancer. J Surg Oncol. 1996; 63:268–270.21. Karpeh MS, Leon L, Klimstra D, Brennan MF. Lymph node staging in gastric cancer: is location more important than Number? An analysis of 1,038 patients. Ann Surg. 2000; 232:362–371.22. Washington K. 7th edition of the AJCC cancer staging manual: stomach. Ann Surg Oncol. 2010; 17:3077–3079.23. Woo Y, Goldner B, Ituarte P, Lee B, Melstrom L, Son T, et al. Lymphadenectomy with optimum of 29 lymph nodes retrieved associated with improved survival in advanced gastric cancer: a 25,000-patient international database study. J Am Coll Surg. 2017; 224:546–555.24. National Cancer Institute (US). Joinpoint Regression Program, Version 4.4.0.0 (Jan 4, 2017). Rockville (MD): National Cancer Institute;2017.25. Degiuli M, Sasako M, Ponti A, Vendrame A, Tomatis M, Mazza C, et al. Randomized clinical trial comparing survival after D1 or D2 gastrectomy for gastric cancer. Br J Surg. 2014; 101:23–31.26. Reid-Lombardo KM, Gay G, Patel-Parekh L, Ajani JA, Donohue JH. Gastric Patient Care Evaluation Group from the Commission on Cancer. Treatment of gastric adenocarcinoma may differ among hospital types in the United States, a report from the National Cancer Data Base. J Gastrointest Surg. 2007; 11:410–419.27. Mullaney PJ, Wadley MS, Hyde C, Wyatt J, Lawrence G, Hallissey MT, et al. Appraisal of compliance with the UICC/AJCC staging system in the staging of gastric cancer. Br J Surg. 2002; 89:1405–1408.28. Birkmeyer JD, Siewers AE, Finlayson EV, Stukel TA, Lucas FL, Batista I, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002; 346:1128–1137.29. Smith DL, Elting LS, Learn PA, Raut CP, Mansfield PF. Factors influencing the volume-outcome relationship in gastrectomies: a population-based study. Ann Surg Oncol. 2007; 14:1846–1852.30. Schmidt B, Yoon SS. D1 versus D2 lymphadenectomy for gastric cancer. J Surg Oncol. 2013; 107:259–264.31. Sano T, Sasako M, Yamamoto S, Nashimoto A, Kurita A, Hiratsuka M, et al. Gastric cancer surgery: morbidity and mortality results from a prospective randomized controlled trial comparing D2 and extended para-aortic lymphadenectomy--Japan Clinical Oncology Group study 9501. J Clin Oncol. 2004; 22:2767–2773.32. Park DJ, Lee HJ, Kim HH, Yang HK, Lee KU, Choe KJ. Predictors of operative morbidity and mortality in gastric cancer surgery. Br J Surg. 2005; 92:1099–1102.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Advantages of Splenic Hilar Lymph Node Dissection in Proximal Gastric Cancer Surgery
- Individualized Surgery for Gastric Cancer
- Endoscopic Submucosal Dissection in the Treatment of Patients With Papillary Early Gastric Cancer
- Risk Factors Affecting Lymph Node Metastasis and Recurrence in Early Gastric Cancer
- Prognostic Significance of the Extent of Lymph Node Dissection in Gastric Cancer