World J Mens Health.
2017 Dec;35(3):178-185. 10.5534/wjmh.16032.
The Correlation between Body Mass Index and Routine Parameters in Men Over Fifty
- Affiliations
-
- 1Department of Urology, Gyeongsang National University Changwon Hospital, Changwon, Korea.
- 2Department of Urology, Gyeongsang National University Hospital, Jinju, Korea. hyunjs@gnu.ac.kr
- 3Department of Urology, Gyeongsang National University School of Medicine, Jinju, Korea.
- 4Department of Urology, CHA Gangnam Medical Center, CHA University, Seoul, Korea.
- 5Department of Urology, Seonam University Myongji Hospital, Goyang, Korea.
- 6Department of Urology, CHA Bundang Medical Center, CHA University, Seongnam, Korea.
- 7Department of Urology, Yonsei University Wonju College of Medicine, Wonju, Korea.
- 8Department of Urology, Dongguk University College of Medicine, Gyeongju, Korea.
- 9Korea Prostate Health Council. Inc., Seoul, Korea.
- KMID: 2398567
- DOI: http://doi.org/10.5534/wjmh.16032
Abstract
- PURPOSE
This study aimed to investigate the relationships between body mass index (BMI) and prostate-specific antigen (PSA) levels, international prostate symptom score (IPSS), quality of life (QoL), and prostate volume (PV).
MATERIALS AND METHODS
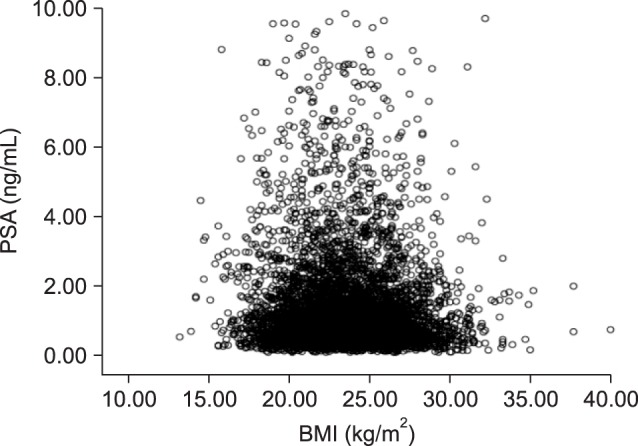
Height, weight, PSA levels, PV, and IPSS were analyzed in 15,435 patients who underwent a prostate examination between 2001 and 2014. Patients aged <50 years or with a PSA level ≥10 ng/mL were excluded. The relationships between BMI and PSA, IPSS, QoL, and PV were analyzed by a scatter plot, one-way analysis of variance, and the Pearson correlation coefficient.
RESULTS
The mean age was 71.95±7.63 years, the mean BMI was 23.59±3.08 kg/m2, the mean PSA level was 1.45±1.45 ng/mL, the mean IPSS was 15.53±8.31, the mean QoL score was 3.48±1.25, and the mean PV was 29.72±14.02 mL. PSA, IPSS, and QoL showed a tendency to decrease with increasing BMI, and there were statistically significant differences for each parameter (p≤0.001). PV showed a significant tendency to increase with BMI (p < 0.001). In the correlation analysis, BMI showed a statistically significant correlation (p < 0.001) with PSA, IPSS, and QoL, although the correlations were very weak. In contrast, BMI showed a significant correlation with PV (p < 0.001), with a meaningful Pearson correlation coefficient of 0.124.
CONCLUSIONS
Higher BMI was associated with lower PSA levels and higher IPSS and QoL scores. Meanwhile, PV increased with BMI. Although obese individuals had a greater PV, obesity did not aggravate lower urinary tract symptoms.
Keyword
MeSH Terms
Figure
Reference
-
1. Parikh NI, Pencina MJ, Wang TJ, Lanier KJ, Fox CS, D'Agostino RB, et al. Increasing trends in incidence of overweight and obesity over 5 decades. Am J Med. 2007; 120:242–250. PMID: 17349447.
Article2. Guh DP, Zhang W, Bansback N, Amarsi Z, Birmingham CL, Anis AH. The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health. 2009; 9:88. PMID: 19320986.
Article3. Faith MS, Butryn M, Wadden TA, Fabricatore A, Nguyen AM, Heymsfield SB. Evidence for prospective associations among depression and obesity in population-based studies. Obes Rev. 2011; 12:e438–e453. PMID: 21414128.
Article4. Ananthapavan J, Sacks G, Moodie M, Carter R. Economics of obesity: learning from the past to contribute to a better future. Int J Environ Res Public Health. 2014; 11:4007–4025. PMID: 24736685.5. Stamey TA, Yang N, Hay AR, McNeal JE, Freiha FS, Redwine E. Prostate-specific antigen as a serum marker for adenocarcinoma of the prostate. N Engl J Med. 1987; 317:909–916. PMID: 2442609.
Article6. Oesterling JE, Chan DW, Epstein JI, Kimball AW Jr, Bruzek DJ, Rock RC, et al. Prostate specific antigen in the preoperative and postoperative evaluation of localized prostatic cancer treated with radical prostatectomy. J Urol. 1988; 139:766–772. PMID: 2451037.
Article7. Krumholtz JS, Carvalhal GF, Ramos CG, Smith DS, Thorson P, Yan Y, et al. Prostate-specific antigen cutoff of 2.6 ng/mL for prostate cancer screening is associated with favorable pathologic tumor features. Urology. 2002; 60:469–473. discussion 473-4. PMID: 12350486.
Article8. Thompson IM, Pauler DK, Goodman PJ, Tangen CM, Lucia MS, Parnes HL, et al. Prevalence of prostate cancer among men with a prostate-specific antigen level < or =4.0 ng per milliliter. N Engl J Med. 2004; 350:2239–2246. PMID: 15163773.9. Freedland SJ, Wen J, Wuerstle M, Shah A, Lai D, Moalej B, et al. Obesity is a significant risk factor for prostate cancer at the time of biopsy. Urology. 2008; 72:1102–1105. PMID: 18722650.
Article10. Pietrzyk B, Olszanecka-Glinianowicz M, Owczarek A, Gabryelewicz T, Almgren-Rachtan A, Prajsner A, et al. Depressive symptoms in patients diagnosed with benign prostatic hyperplasia. Int Urol Nephrol. 2015; 47:431–440. PMID: 25673555.
Article11. Parsons JK, Bergstrom J, Silberstein J, Barrett-Connor E. Prevalence and characteristics of lower urinary tract symptoms in men aged > or = 80 years. Urology. 2008; 72:318–321. PMID: 18554695.12. Zhao S, Chen C, Chen Z, Xia M, Tang J, Shao S, et al. Relationship between metabolic syndrome and predictors for clinical benign prostatic hyperplasia progression and international prostate symptom score in patients with moderate to severe lower urinary tract symptoms. Urol J. 2016; 13:2717–2726. PMID: 27351328.13. Kim GW, Doo SW, Yang WJ, Song YS. Effects of obesity on prostate volume and lower urinary tract symptoms in Korean men. Korean J Urol. 2010; 51:344–347. PMID: 20495698.
Article14. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: The Evidence Report. National Institutes of Health. Obes Res. 1998; 6(Suppl 2):51S–209S. PMID: 9813653.15. Thompson IM, Leach R, Troyer D, Pollock B, Naylor S, Higgins B. Relationship of body mass index and prostate specific antigen in a population-based study. Urol Oncol. 2004; 22:127–131. PMID: 15082010.
Article16. Fowke JH, Motley SS, Cookson MS, Concepcion R, Chang SS, Wills ML, et al. The association between body size, prostate volume and prostate-specific antigen. Prostate Cancer Prostatic Dis. 2007; 10:137–142. PMID: 17179979.
Article17. Lee RK, Chung D, Chughtai B, Te AE, Kaplan SA. Central obesity as measured by waist circumference is predictive of severity of lower urinary tract symptoms. BJU Int. 2012; 110:540–545. PMID: 22243806.
Article18. Jeong IG, Hwang SS, Kim HK, Ahn H, Kim CS. The association of metabolic syndrome and its components with serum prostate-specific antigen levels in a Korean-screened population. Cancer Epidemiol Biomarkers Prev. 2010; 19:371–380. PMID: 20086117.
Article19. Werny DM, Thompson T, Saraiya M, Freedman D, Kottiri BJ, German RR, et al. Obesity is negatively associated with prostate-specific antigen in U.S. men, 2001-2004. Cancer Epidemiol Biomarkers Prev. 2007; 16:70–76. PMID: 17179487.
Article20. Freedland SJ, Platz EA, Presti JC Jr, Aronson WJ, Amling CL, Kane CJ, et al. Obesity, serum prostate specific antigen and prostate size: implications for prostate cancer detection. J Urol. 2006; 175:500–504. discussion 504. PMID: 16406980.
Article21. Bañez LL, Hamilton RJ, Partin AW, Vollmer RT, Sun L, Rodriguez C, et al. Obesity-related plasma hemodilution and PSA concentration among men with prostate cancer. JAMA. 2007; 298:2275–2280. PMID: 18029831.
Article22. Wright ME, Chang SC, Schatzkin A, Albanes D, Kipnis V, Mouw T, et al. Prospective study of adiposity and weight change in relation to prostate cancer incidence and mortality. Cancer. 2007; 109:675–684. PMID: 17211863.
Article23. Hekal IA, Ibrahiem EI. Obesity-PSA relationship: a new formula. Prostate Cancer Prostatic Dis. 2010; 13:186–190. PMID: 20029402.
Article24. Haidinger G, Temml C, Schatzl G, Brössner C, Roehlich M, Schmidbauer CP, et al. Risk factors for lower urinary tract symptoms in elderly men. For the Prostate Study Group of the Austrian Society of Urology. Eur Urol. 2000; 37:413–420. PMID: 10765071.25. Yee CH, So WY, Yip SK, Wu E, Yau P, Ng CF. Effect of weight reduction on the severity of lower urinary tract symptoms in obese male patients with benign prostatic hyperplasia: a randomized controlled trial. Korean J Urol. 2015; 56:240–246. discussion 246-7. PMID: 25763129.
Article26. Cyrus A, Kabir A, Goodarzi D, Talaei A, Moradi A, Rafiee M, et al. Impact of metabolic syndrome on response to medical treatment of benign prostatic hyperplasia. Korean J Urol. 2014; 55:814–820. PMID: 25512816.
Article27. Boyle P, Robertson C, Mazzetta C, Keech M, Hobbs R, Fourcade R, et al. The relationship between lower urinary tract symptoms and health status: the UREPIK study. BJU Int. 2003; 92:575–580. PMID: 14511037.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Difference of the Obesity Index, Blood Pressure and Serum Lipids in Abdominal and Non Abdominal in Men and Women
- Testicular Volume of Korean Young Adult Men as Measured by Ultrasonography: Relationship with Body Mass Index
- The Accuracy of Self-Reported Weight and Height
- The Relationship Between Intraocular Pressure and Health Parameters
- Effects of changes in lifestyle and biological parameters on blood lipid levels in middle aged men