J Adv Prosthodont.
2017 Dec;9(6):476-481. 10.4047/jap.2017.9.6.476.
Oral health-related quality of life in patients with implant treatment
- Affiliations
-
- 1Department of Oral Implantology, Osaka Dental University, Hirakata, Japan. arai-k@cc.osaka-dent.ac.jp
- KMID: 2398053
- DOI: http://doi.org/10.4047/jap.2017.9.6.476
Abstract
- PURPOSE
Patient-reported outcomes are increasingly commonly used as a method of evaluating treatments. This cross-sectional study aimed to evaluate implant treatment from the perspective of patient-reported outcomes.
MATERIALS AND METHODS
Subjects were 804 patients who visited the Department of Oral Implantology at Osaka Dental University. The participants were categorized into a pre-implant group and a post-implant group. They were further categorized into five subgroups based on the number of occlusal supports provided by the remaining teeth according to the Eichner classification. The participants answered a basic questionnaire and the General Oral Health Assessment Index (GOHAI) questionnaire, an oral health-related quality of life (QOL) scale. GOHAI scores were compared according to the number of occlusal supports within each group and between the two groups.
RESULTS
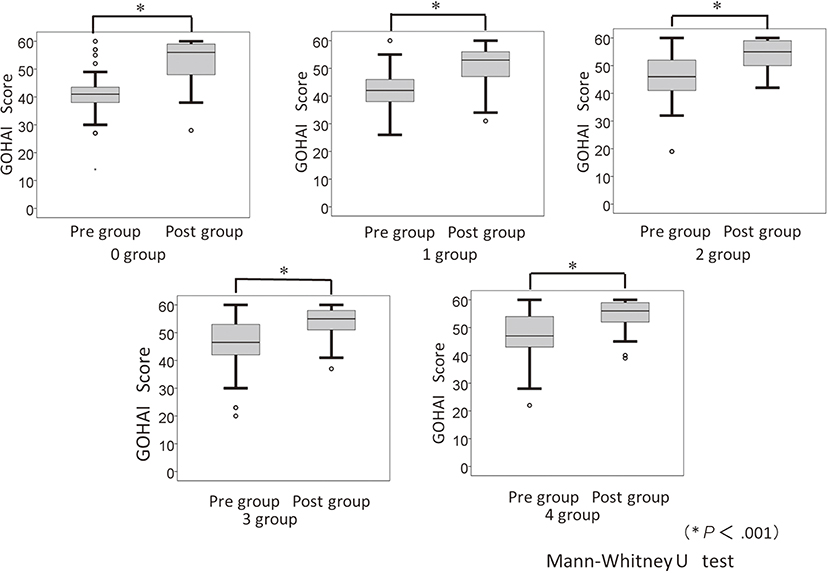
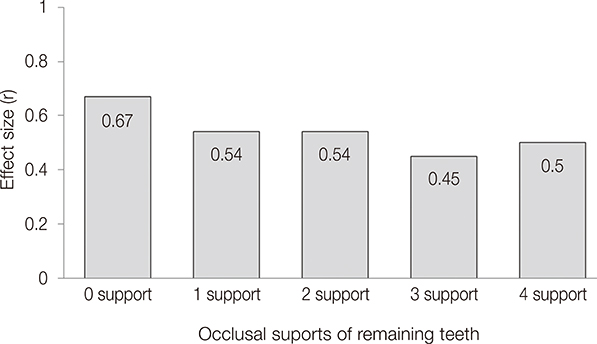
The results revealed a significant difference in terms of the number of occlusal supports within the pre-implant group; GOHAI scores decreased as the number of occlusal supports decreased (P < .001). However, no significant difference was observed in GOHAI scores in terms of the number of occlusal supports in the post-implant group (P>.05). GOHAI scores significantly improved in both pre- and post-implant groups in all occlusal support subgroups (P < .001).
CONCLUSION
GOHAI scores decrease as occlusal support is lost. However, implant treatment performed in areas of loss improves the GOHAI score when occlusal support is restored.
Keyword
MeSH Terms
Figure
Reference
-
1. Slade GD, Spencer AJ. Development and evaluation of the Oral Health Impact Profile. Community Dent Health. 1994; 11:3–11.2. Okamoto S, Suzuki H, Kanyama M, Arakawa H, Sonoyama W, Kuboki T, Yamashita A. Reliability and validity evaluation of an oral-health-related quality of life questionnaire for patients with missing teeth. Japan Prosthodontic Soc J Jpn Prosthodont Soc. 1999; 43:698–705.3. Atchison KA, Dolan TA. Development of the Geriatric Oral Health Assessment Index. J Dent Educ. 1990; 54:680–687.4. Naito M, Suzukamo Y, Nakayama T, Hamajima N, Fukuhara S. Linguistic adaptation and validation of the General Oral Health Assessment Index (GOHAI) in an elderly Japanese population. J Public Health Dent. 2006; 66:273–275.5. Nakai N, Sadamori S, Kawamura M, Sasahara H, Hamada T. Bilinguals' Responses to Oral Health Impact Profile (OHIP) Written in English and in Japanese. J Jpn Prosthodont Soc. 2004; 48:163–172.6. Nogawa T, Takayama Y, Kato T, Yamazaki Y, Moriya S, Kitagawa Y, Yokoyama A. A study of factors associated with the short-form oral health impact profile (OHIP-14) in community-dwelling older adults. Ann Jpn Prosthodont Soc. 2015; 7:37–45.7. Ikebe K, Watkins CA, Ettinger RL, Sajima H, Nokubi T. Application of short-form oral health impact profile on elderly Japanese. Gerodontology. 2004; 21:167–176.8. Shiina M, Kono M, Sato Y, Muraoka M, Kitagawa N. Evaluation of new complete denture treatment by dentists and patients. Nihon Hotetsu Shika Gakkai Zasshi. 2008; 52:301–310.9. Cakir O, Kazancioglu HO, Celik G, Deger S, Ak G. Evaluation of the efficacy of mandibular conventional and implant prostheses in a group of Turkish patients: a quality of life study. J Prosthodont. 2014; 23:390–396.10. Swelem AA, Gurevich KG, Fabrikant EG, Hassan MH, Aqou S. Oral health-related quality of life in partially edentulous patients treated with removable, fixed, fixed-removable, and implant-supported prostheses. Int J Prosthodont. 2014; 27:338–347.11. Bramanti E, Matacena G, Cecchetti F, Arcuri C, Cicciù M. Oral health-related quality of life in partially edentulous patients before and after implant therapy: a 2-year longitudinal study. Oral Implantol (Rome). 2013; 6:37–42.12. Mizumoto A, Takeuchi O. Basics and considerations for reporting effect sizes in research papers. Engl Lang Edu Soc. 2008; 31:57–66.13. Padilha DM, Hilgert JB, Hugo FN, Bós AJ, Ferrucci L. Number of teeth and mortality risk in the Baltimore Longitudinal Study of Aging. J Gerontol A Biol Sci Med Sci. 2008; 63:739–744.14. Hung HC, Joshipura KJ, Colditz G, Manson JE, Rimm EB, Speizer FE, Willett WC. The association between tooth loss and coronary heart disease in men and women. J Public Health Dent. 2004; 64:209–215.15. Nakanishi N, Fukuda H, Takatorige T, Tatara K. Relationship between self-assessed masticatory disability and 9-year mortality in a cohort of community-residing elderly people. J Am Geriatr Soc. 2005; 53:54–58.16. Aida J, Kondo K, Hirai H, Nakade M, Yamamoto T, Hanibuchi T, Osaka K, Sheiham A, Tsakos G, Watt RG. Association between dental status and incident disability in an older Japanese population. J Am Geriatr Soc. 2012; 60:338–343.17. Shimazaki Y, Soh I, Saito T, Yamashita Y, Koga T, Miyazaki H, Takehara T. Influence of dentition status on physical disability, mental impairment, and mortality in institutionalized elderly people. J Dent Res. 2001; 80:340–345.18. Yamamoto T, Kondo K, Hirai H, Nakade M, Aida J, Hirata Y. Association between self-reported dental health status and onset of dementia: a 4-year prospective cohort study of older Japanese adults from the Aichi Gerontological Evaluation Study (AGES) Project. Psychosom Med. 2012; 74:241–248.19. Ministry of Health, Labour, and Welfare. 2011 Survey of Dental Diseases. http://www.mhlw.go.jp/toukei/list/dl/62-17c23-1.20. Hosoi T, Tojo T, Tsurumoto A, Kondou A. A survey of the quality of life and making a questionnaire for complete denture wearers. Jpn Soc Gerodontology. 2002; 16:336–343.21. Hugo FN, Hilgert JB, de Sousa Mda L, Cury JA. Oral status and its association with general quality of life in older independent-living south-Brazilians. Community Dent Oral Epidemiol. 2009; 37:231–240.22. Nogawa T, Takayama Y, Kato T, Yamazaki Y, Moriya S, Kitagawa Y, Yokoyama A. A study of factors associated with the short-form oral health impact PROfile (OHIP-14) in community-dwelling older adults. Ann Jpn Prosthodont Soc. 2015; 7:37–45.23. Fukuda H. Dark side of quality of life assessment in oncology clinical trials. J Clin Oncol. 2013; 12:440–449.24. Yoshida M, Nakamoto T, Sato Y, Akagawa Y. The influence of the extent of missing teeth on the satisfaction of daily living for elderly people a questionnaire for the elderly at kure city in Hiroshima prefecture. Jpn J Gerodontology. 1997; 11:174–180.25. Morisaki N, Miura H, Hara S, Yamasaki K. Relationship between Decline of Swallowing Function and Health-related QOLamong Frail Elderly Persons. Jpn J Gerodontology. 2013; 28:20–26.26. Hashimoto C, Yoshihara A, Miyazaki H. The factors associated with appetite and chewing difficulty in community-dwelling elderly people. J Dent Health. 2014; 64:284–290.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Structural equation modeling for association between patient satisfaction and quality of life after implant surgery
- Effects of oral health-related self-efficacy on oral health-related quality of life in male high school students
- The effects of toothache experience and oral health behavior on Health-Related Quality of Life in Korean adults -using the second edition of the 8th National Health Nutrition Survey (2019-2020)
- Effect of Oral Health-Related Quality of Life on School Life Satisfaction in High School Students
- The Relationships between Orthodontic Treatment, Oral Health-Related Quality of Life, and Happiness of among Some High School Students