Ann Hepatobiliary Pancreat Surg.
2017 Nov;21(4):228-231. 10.14701/ahbps.2017.21.4.228.
Primary gigantic leiomyosarcoma of the liver treated with portal vein embolization and liver resection
- Affiliations
-
- 1Department of Surgery, European Interbalkan Medical Centre, Thessaloniki, Greece. dgiak@auth.gr
- 2Division of Transplant Surgery, Department of Surgery, Medical School, Aristotle University of Thessaloniki, Greece.
- 3Department of HPB Surgery, Royal London Hospital, London, UK.
- 4Department of Anesthesiology, European Interbalkan Medical Centre, Thessaloniki, Greece.
- 5Histodierevnitiki Laboratory of Pathology, European Interbalkan Medical Centre, Thessaloniki, Greece.
- KMID: 2397804
- DOI: http://doi.org/10.14701/ahbps.2017.21.4.228
Abstract
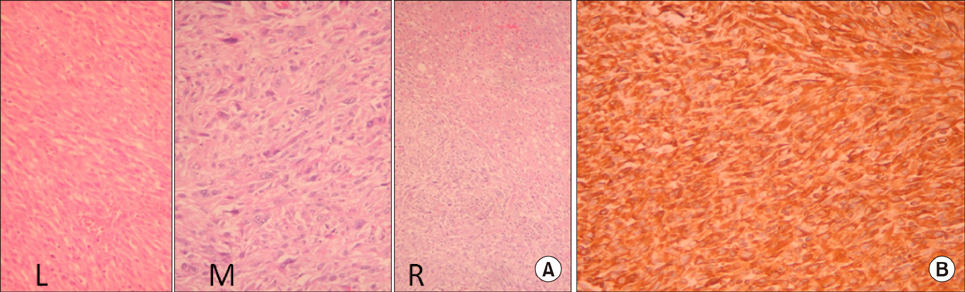
- Primary hepatic leiomyosarcoma (PHL) is an extremely rare tumor. The tumor has no specific presentations and often diagnosis is delayed until it reaches a significant size. We report the case of a 69-year-old female presented with a huge PHL. Due to size of the tumor and to be operable, the patient subjected to right portal vein embolization (PVE) and selective embolization of segment V. Four weeks after the PVE, liver resection was conducted (Segments V+VI bisegmentectomy plus resection of IVA). The patient had an uncomplicated post-operative course, and discharged at the 8th post-operative day. Diagnosis of PHL was confirmed by histopathological and immunohistochemical examinations. The patient refused to receive adjuvant chemotherapy, and revealed evidence of recurrence six months after the operation, and finally died 12 months after the operation and 16 months after initial diagnosis. PHL is an extremely rare tumor and often in first presentation has significant size. Radical surgery with adjuvant chemotherapy is key feature for prolonged survival.
MeSH Terms
Figure
Cited by 1 articles
-
Primary leiomyosarcoma of the liver: Two new cases and a systematic review
Francesco Esposito, Chetana Lim, Laurence Baranes, Chady Salloum, Cyrille Feray, Julien Calderaro, Daniel Azoulay
Ann Hepatobiliary Pancreat Surg. 2020;24(1):63-67. doi: 10.14701/ahbps.2020.24.1.63.
Reference
-
1. Maki HS, Hubert BC, Sajjad SM, Kirchner JP, Kuehner ME. Primary hepatic leiomyosarcoma. Arch Surg. 1987; 122:1193–1196.2. Weitz J, Klimstra DS, Cymes K, Jarnagin WR, D'Angelica M, La Quaglia MP, et al. Management of primary liver sarcomas. Cancer. 2007; 109:1391–1396.3. Holloway H, Walsh CB, Thomas R, Fielding J. Primary hepatic leiomyosarcoma. J Clin Gastroenterol. 1996; 23:131–133.4. Yamaguchi J, Azuma T, Fujioka H, Tanaka K, Furui J, Tomioka T, et al. Leiomyosarcoma occurring in the ligamentum teres of the liver: a case report and a review of seven reported cases. Hepatogastroenterology. 1996; 43:1051–1056.5. Shivathirthan N, Kita J, Iso Y, Hachiya H, Kyunghwa P, Sawada T, et al. Primary hepatic leiomyosarcoma: case report and literature review. World J Gastrointest Oncol. 2011; 3:148–152.6. Pinson CW, Lopez RR, Ivancev K, Ireland K, Sawyers JL. Resection of primary hepatic malignant fibrous histiocytoma, fibrosarcoma, and leiomyosarcoma. South Med J. 1994; 87:384–391.7. Ferrozzi F, Bova D, Zangrandi A, Garlaschi G. Primary liver leiomyosarcoma: CT appearance. Abdom Imaging. 1996; 21:157–160.8. Lv WF, Han JK, Cheng DL, Tang WJ, Lu D. Imaging features of primary hepatic leiomyosarcoma: a case report and review of literature. Oncol Lett. 2015; 9:2256–2260.9. Yu RS, Chen Y, Jiang B, Wang LH, Xu XF. Primary hepatic sarcomas: CT findings. Eur Radiol. 2008; 18:2196–2205.10. Smith MB, Silverman JF, Raab SS, Towell BD, Geisinger KR. Fine-needle aspiration cytology of hepatic leiomyosarcoma. Diagn Cytopathol. 1994; 11:321–327.11. Sprogøe-Jakobsen S, Hølund B. Immunohistochemistry (Ki-67 and p53) as a tool in determining malignancy in smooth muscle neoplasms (exemplified by a myxoid leiomyosarcoma of the uterus). APMIS. 1996; 104:705–708.12. Liang X, Xiao-Min S, Jiang-Ping X, Jie-Yu Y, Xiao-Jun Z, Zhi-Ren F, et al. Liver transplantation for primary hepatic leiomyosarcoma: a case report and review of the literatures. Med Oncol. 2010; 27:1269–1272.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Portal vein embolization prior to hepatectomy: Techniques, outcomes and novel therapeutic approaches
- Refractory Ascites with Intrahepatic Portal Thrombosis after Living Donor Liver Transplantation Successfully Treated by Splenic Artery Embolization and Apixaban (Case Report)
- Right trisectionectomy with en bloc portal vein resection for perihilar cholangiocarcinoma after preoperative left portal vein stenting and sequential right portal and hepatic vein embolization
- Hemoperitoneum due to Ruptured Paraumbilical Vein in a Cirrhotic Patient with Portal Hypertension: Treatment by means of Coil Embolization
- Liver Transplantation in Liver Cirrhosis Patients Accompanied by Portal Vein Thrombosis