J Korean Med Sci.
2017 Dec;32(12):2064-2068. 10.3346/jkms.2017.32.12.2064.
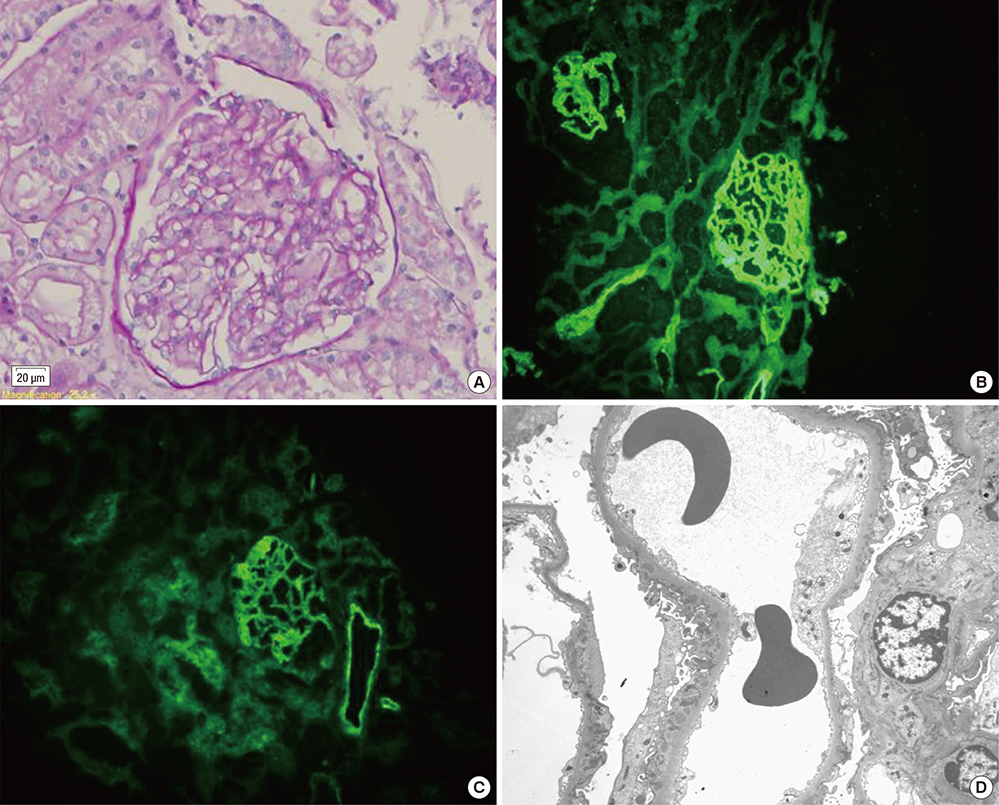
Hypocomplementemic Urticarial Vasculitis Syndrome with Membranous Nephropathy: Case Report
- Affiliations
-
- 1Department of Medicine, Graduate School, Kyung Hee University, Seoul, Korea.
- 2Division of Rheumatology, Department of Internal Medicine, Kyung Hee University Medical Center, Seoul, Korea. aprildaum@hanmail.net
- 3Division of Nephrology, Department of Internal Medicine, Kyung Hee University Medical Center, Seoul, Korea.
- 4Division of Nephrology, Asan Chungmu Hospital, Asan, Korea.
- KMID: 2396387
- DOI: http://doi.org/10.3346/jkms.2017.32.12.2064
Abstract
- Urticarial vasculitis is a rare disorder that principally manifests with recurrent urticarial, sometimes hemorrhagic, skin lesions and/or angioedema. Its clinical presentation is not always limited to cutaneous lesions and it can potentially affect other organs, such as the joints, lungs, kidneys, and eyes. Systemic involvement can either be present at the onset of disease or develop over time. In cases with systemic manifestations, urticarial vasculitis is more likely to be associated with a low complement level. We present the case of a teenage boy with hypocomplementemic urticarial vasculitis syndrome (HUVS) that occurred shortly following swine-origin influenza A virus infection in 2009. Afterwards, HUVS was systemically complicated with myositis and membranous nephropathy that developed several months and about 2 years after its onset, respectively. A combination of glucocorticoid and immunosuppressive agents has been used to effectively control disease activity.
MeSH Terms
Figure
Reference
-
1. McDuffie FC, Sams WM Jr, Maldonado JE, Andreini PH, Conn DL, Samayoa EA. Hypocomplementemia with cutaneous vasculitis and arthritis. Possible immune complex syndrome. Mayo Clin Proc. 1973; 48:340–348.2. Black AK. Urticarial vasculitis. Clin Dermatol. 1999; 17:565–569.3. Park C, Choi SW, Kim M, Park J, Lee JS, Chung HC. Membranoproliferative glomerulonephritis presenting as arthropathy and cardiac valvulopathy in hypocomplementemic urticarial vasculitis: a case report. J Med Case Reports. 2014; 8:352.4. Schwartz HR, McDuffie FC, Black LF, Schroeter AL, Conn DL. Hypocomplementemic urticarial vasculitis: association with chronic obstructive pulmonary disease. Mayo Clin Proc. 1982; 57:231–238.5. Pickering MC, Botto M. Are anti-C1q antibodies different from other SLE autoantibodies? Nat Rev Rheumatol. 2010; 6:490–493.6. Jachiet M, Flageul B, Deroux A, Le Quellec A, Maurier F, Cordoliani F, Godmer P, Abasq C, Astudillo L, Belenotti P, et al. The clinical spectrum and therapeutic management of hypocomplementemic urticarial vasculitis: data from a French nationwide study of fifty-seven patients. Arthritis Rheumatol. 2015; 67:527–534.7. Her MY, Song JY, Kim DY. Hypocomplementemic urticarial vasculitis in systemic lupus erythematosus. J Korean Med Sci. 2009; 24:184–186.8. Uva L, Miguel D, Pinheiro C, Freitas JP, Marques Gomes M, Filipe P. Cutaneous manifestations of systemic lupus erythematosus. Autoimmune Dis. 2012; 2012:834291.9. Davis MD, Brewer JD. Urticarial vasculitis and hypocomplementemic urticarial vasculitis syndrome. Immunol Allergy Clin North Am. 2004; 24:183–213. vi10. Petri M, Orbai AM, Alarcón GS, Gordon C, Merrill JT, Fortin PR, Bruce IN, Isenberg D, Wallace DJ, Nived O, et al. Derivation and validation of the Systemic Lupus International Collaborating Clinics classification criteria for systemic lupus erythematosus. Arthritis Rheum. 2012; 64:2677–2686.11. Kurts C, Panzer U, Anders HJ, Rees AJ. The immune system and kidney disease: basic concepts and clinical implications. Nat Rev Immunol. 2013; 13:738–753.12. Chew GY, Gatenby PA. Inflammatory myositis complicating hypocomplementemic urticarial vasculitis despite on-going immunosuppression. Clin Rheumatol. 2007; 26:1370–1372.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hypocomplementemic Urticarial Vasculitis in Systemic Lupus Erythematosus
- A case of hypocomplementemic urticarial vasculitis syndrome with cold urticaria
- A case of membranous nephropathy associated with relapsing polychondritis
- Plasmapheresis in a Patient With "Refractory" Urticarial Vasculitis
- Omalizumab as a Succesfull Therapy in Normocomplementemic Urticarial Vasculitis: A Series of Four Patients and Review of the Literature