J Korean Neurosurg Soc.
2017 Nov;60(6):627-634. 10.3340/jkns.2016.0707.003.
Mechanical Thrombectomy with Solitaire Stent Retrieval for Acute Cardioembolic Stroke
- Affiliations
-
- 1Department of Neurosurgery, Dongguk University Ilsan Hospital, Goyang, Korea. han850317@naver.com
- 2Department of Neurosurgery, Dongguk University College of Medicine, Seoul, Korea.
- KMID: 2395781
- DOI: http://doi.org/10.3340/jkns.2016.0707.003
Abstract
OBJECTIVE
Few studies have reported the outcome of mechanical thrombectomy with Solitaire stent retrival (MTSR) in subtypes of acute ischemic stroke. The purpose of this study was to evaluate the efficacy and result of MTSR in acute cardioembolic stroke.
METHODS
Twenty consecutive patients with acute cardioembolic stroke were treated by MTSR. The angiographic outcome was assessed by thrombolysis in cerebral infarction (TICI) grade. TICI grade 2a, 2b, or 3 with a measurable thrombus that was retrieved was considered as a success when MTSR was performed in the site of primary vessel occlusion, and TICI grade 2b or 3 was considered as a success when final result was reported. Clinical and radiological results were compared between two groups divided on the basis of final results of MTSR. Persistent thrombus compression sign on angiogram was defined as a stenotic, tapered arterial lumen whenever temporary stenting was performed. The clinical outcomes were assessed by the modified Rankin Scale (mRS) at 3 months.
RESULTS
The failure rate of MTSR was 20% (4/20) and other modalities, such as permanent stenting, were needed. Final successful recanalization (TICI grade 2b or 3) was 80% when other treatments were included. The rate of good outcome (mRS≤2) was 35% at the 3-month follow-up. Failure of MTSR was significantly correlated with persistent thrombus compression sign (p=0.001).
CONCLUSION
Some cases of cardioembolic stroke are resistant to MTSR and may need other treatment modalities. Careful interpretation of angiogram may be helpful to the decision.
MeSH Terms
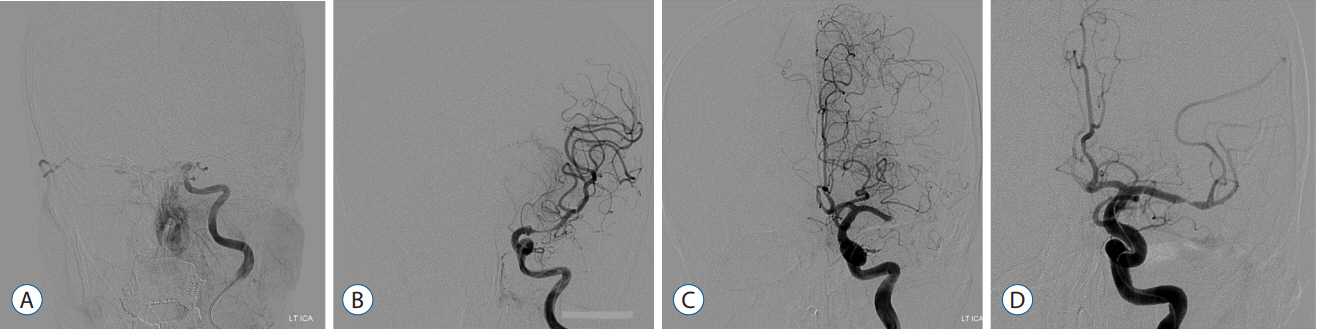
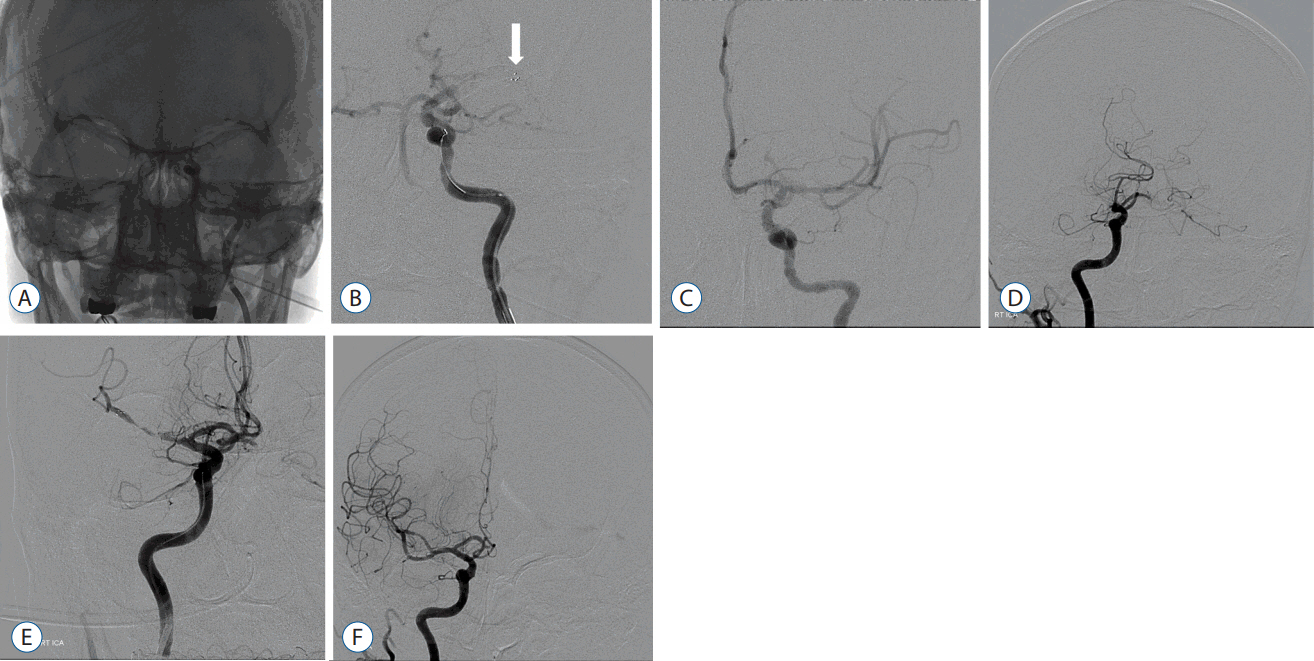
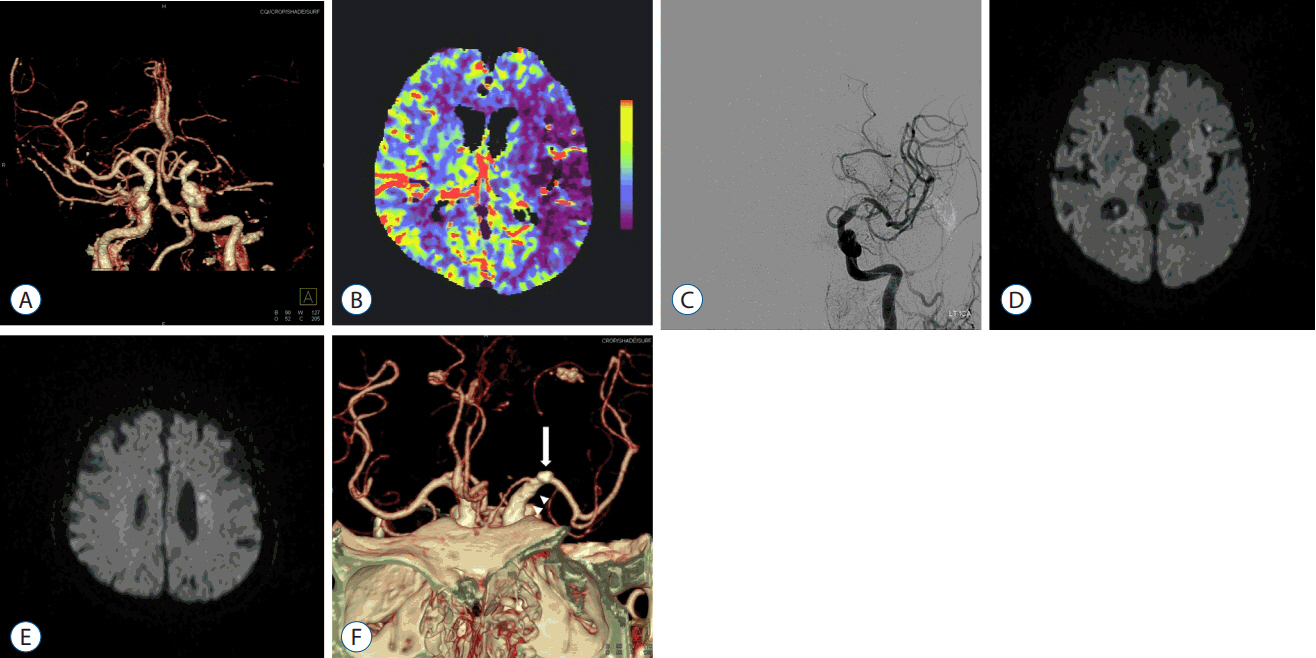
Figure
Reference
-
References
1. Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial TOAST Trial of Org 10172 in Acute Stroke Treatment. Stroke. 24:35–41. 1993.
Article2. Akins PT, Amar AP, Pakbaz RS, Fields JD. SWIF Investigators. Complications of endovascular treatment for acute stroke in the SWIFT trial with solitaire and Merci devices. AJNR Am J Neuroradiol. 35:524–528. 2014.
Article3. Arboix A, Alió J. Cardioembolic stroke: clinical features, specific cardiac disorders and prognosis. Curr Cardio Rev. 6:150–161. 2010.
Article4. Baek JH, Kim BM, Kim DJ, Heo JH, Nam HS, Yoo J. Stenting as a rescue treatment after failure of mechanical thrombectomy for anterior circulation large artery occlusion. Stroke. 47:2360–2363. 2016.
Article5. Baruch D. Platelet--vessel wall interactions. Therapie. 5:371–378. 2006.6. Bhatia R, Hill MD, Shobha N, Menon B, Bal S, Kochar P, et al. Low rates of acute recanalization with intravenous recombinant tissue plasminogen activator in ischemic stroke: real-world experience and a call for action. Stroke. 41:2254–2258. 2010.
Article7. Chueh J, Kuhn AL, Mehra M, Feula G, Wakhloo AK, Gounis MJ. Embolus adhesion to activated endothelium after embolization: a parameter to predict outcomes of mechanical thrombectomy in acute ischemic stroke. Stroke. 43:A3750. 2012.8. Chueh JY, Wakhloo AK, Hendricks GH, Silva CF, Weaver JP, Gounis MJ. Mechanical characterization of thromboemboli in acute ischemic stroke and laboratory embolus analogs. AJNR Am J Neuroradiol. 32:1237–1244. 2011.
Article9. Costalat V, Machi P, Lobotesis K, Maldonado I, Vendrell JF, Riquelme C, et al. Rescue, combined, and stand-alone thrombectomy in the management of large vessel occlusion stroke using the solitaire device: a prospective 50-patient single-center study: timing, safety, and efficacy. Stroke. 42:1929–1935. 2011.
Article10. Esmon CT. Basic mechanisms and pathogenesis of venous thrombosis. Blood Rev. 23:225–229. 2009.
Article11. Fineschi V, Turillazzi E, Neri M, Pomara C, Riezzo I. Histological age determination of venous thrombosis: a neglected forensic task in fatal pulmonary thrombo-embolism. Forensic Sci Internat. 186:22–28. 2009.
Article12. Gralla J, Brekenfeld C, Mordasini P, Schroth G. Mechanical thrombolysis and stenting in acute ischemic stroke. Stroke. 43:280–285. 2012.
Article13. Han SW, Kim SH, Lee JY, Chu CK, Yang JH, Shin HY, et al. A new subtype classification of ischemic stroke based on treatment and etiologic mechanism. Eur Neurol. 57:96–102. 2007.
Article14. Karšaj I, Humphrey JD. A mathematical model of evolving mechanical properties of intraluminal thrombus. Biorheology. 46:509–527. 2009.
Article15. Kim TK, Rhim JK, Lee CJ, Oh SH, Chung BS. The limitations of thrombectomy with SolitaireTM AB as first-line treatment in acute ischemic stroke: a single center experience. J Cerebrovasc Endovasc Neurosurg. 14:203–209. 2012.
Article16. Levy EI, Siddiqui AH, Crumlish A, Snyder KV, Hauck EF, Fiorella DJ, et al. First Food and Drug Administration-approved prospective trial of primary intracranial stenting for acute stroke: SARIS (stent-assisted recanalization in acute ischemic stroke). Stroke. 40:3552–3556. 2009.
Article17. Liebeskind DS, Sanossian N, Yong WH, Starkman S, Tsang MP, Moya AL, et al. CT and MRI early vessel signs reflect clot composition in acute stroke. Stroke. 42:1237–1243. 2011.
Article18. Machi P, Costalat V, Lobotesis K, Maldonado IL, Vendrell JF, Riquelme C, et al. Solitaire FR thrombectomy system: immediate results in 56 consecutive acute ischemic stroke patients. J Neurointerv Surg. 4:62–66. 2012.
Article19. Marder VJ, Chute DJ, Starkman S, Abolian AM, Kidwell C, Liebeskind D, et al. Analysis of thrombi retrieved from cerebral arteries of patients with acute ischemic stroke. Stroke. 37:2086–2093. 2006.
Article20. Mehta BP, Nogueira RG. Should clot composition affect choice of endovascular therapy? Neurology. 79(13 Suppl 1):S63–S67. 2012.
Article21. National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med. 333:1581–1587. 1995.22. Niesten JM, van der Schaaf IC, van Dam L, Vink A, Albert Vos J, Schonewille WJ, et al. Histopathologic composition of cerebral thrombi of acute stroke patients is correlated with stroke subtype and thrombus attenuation. PLoS One. 9:e88882. 2014.
Article23. Nogueira RG, Sukavaneshvar S, Rabinov JD, Dabus G, Yoo AJ, Buonanno FS, et al. Scanning electron microscopy analysis of thromboembolic material retrieved from cerebral and cervical arteries of patients with acute ischemic stroke: Abstracts from the 2008 international stroke conference. Stroke. 39:562. 2008.24. Nosaka M, Ishida Y, Kimura A, Kondo T. Time-dependent organic changes of intravenous thrombi in stasis-induced deep vein thrombosis model and its application to thrombus age determination. Forensic Sci Int. 195:143–147. 2010.
Article25. Romeo G, Martinez ML, Maroto J, Felez J. Blood clot simulation model by using the Bond-Graph technique. Scientific World Journal. 2013:519047. 2013.26. Ruggeri ZM. Platelets in atherothrombosis. Nat Med. 8:1227–1234. 2002.
Article27. Ruggeri ZM, Mendolicchio GL. Adhesion mechanisms in platelet function. Circ Res. 100:1673–1685. 2007.
Article28. Ruggeri ZM, Orje JN, Habermann R, Federici AB, Reininger AJ. Activation-independent platelet adhesion and aggregation under elevated shear stress. Blood. 108:1903–1910. 2006.
Article29. Shiozaki S, Ishikawa KL, Takagi S. Numerical study on platelet adhesion to vessel walls using the kinetic Monte Carlo method. JBSE. 7:275–283. 2012.
Article30. Stampfl S, Hartmann M, Ringleb PA, Haehnel S, Bendszus M, Rohde S. Stent placement for flow restoration in acute ischemic stroke: a single-center experience with the Solitaire stent system. AJNR Am J Neuroradiol. 32:1245–1248. 2011.
Article31. Tan JC, Dillon WP, Liu S, Adler F, Smith WS, Wintermark M. Systematic comparison of perfusion-CT and CT-angiography in acute stroke patients. Ann Neurol. 61:533–543. 2007.
Article32. Viera AJ, Garrett JM. Understanding interobserver agreement: the kappa statistic. Fam Med. 37:360–363. 2005.33. Ware JA, Heistad DD. Platelet-endothelium interactions. N Engl J Med. 328:628–635. 1993.
Article34. Zangerle A, Kiechl S, Spiegel M, Furtner M, Knoflach M, Werner P, et al. Recanalization after thrombolysis in stroke patients: predictors and prognostic implications. Neurology. 68:39–44. 2007.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Safety and Efficacy of Mechanical Thrombectomy with Solitaire Stent Retrieval for Acute Ischemic Stroke: A Systematic Review
- Unexpected Detachment of Solitaire Stents during Mechanical Thrombectomy
- Refinement of a Thrombectomy Technique to Treat Acute Ischemic Stroke: Technical Note on Microcatheter Advance during Retrieving Self-Expandable Stent
- The Limitations of Thrombectomy with Solitaire(TM) AB as First-line Treatment in Acute Ischemic Stroke: A Single Center Experience
- Mechanical Thrombectomy Using a Solitaire Stent in Acute Ischemic Stroke: The Relationship between the Visible Antegrade Flow on First Device Deployment and Final Success in Revascularization