Ann Dermatol.
2017 Dec;29(6):742-746. 10.5021/ad.2017.29.6.742.
The Lateral Tarsal Strip for Paralytic Ectropion in Patients with Leprosy
- Affiliations
-
- 1Department of Dermatology, Veterans Health Service Medical Center, Seoul, Korea.
- 2Division of Dermatology, Department of Medicine, Hanyang University Graduate School, Seoul, Korea.
- 3Department of Dermatology, Gachon University Gil Medical Center, Incheon, Korea. parkhjmd@gmail.com
- KMID: 2395182
- DOI: http://doi.org/10.5021/ad.2017.29.6.742
Abstract
- BACKGROUND
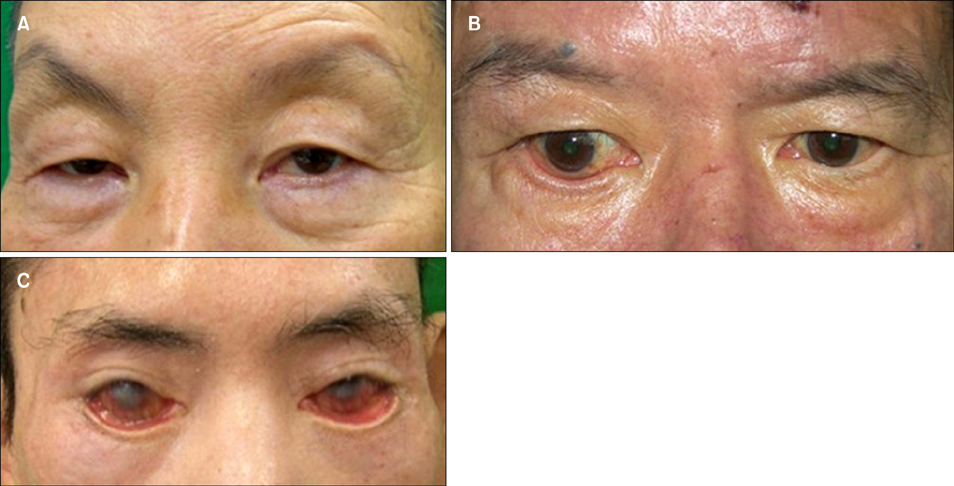
In patients with leprosy, paralysis of the facial nerve results in the lower eyelid ectropion and lagophthalmos as a sequela even when the leprosy is cured. Paralytic ectropion causes many functional and cosmetic eye problems, leading to blindness if left untreated.
OBJECTIVE
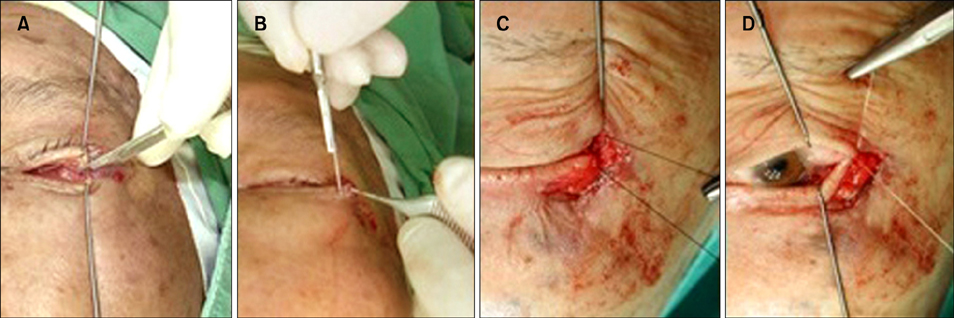
The purpose of this retrospective study is to evaluate the efficacy of surgical correction of paralytic ectropion, the lateral tarsal strip, in patients with leprosy.
METHODS
Between 2010 and 2015, 40 Korean patients (44 eyelids) with paralytic ectropion who had visited Korean Hansen Welfare Association Hospital were treated with the lateral tarsal strip. Four-point patients' global assessment scale, local complications, and recurrence were assessed at the end of follow-up period. The average follow-up period was 12 months.
RESULTS
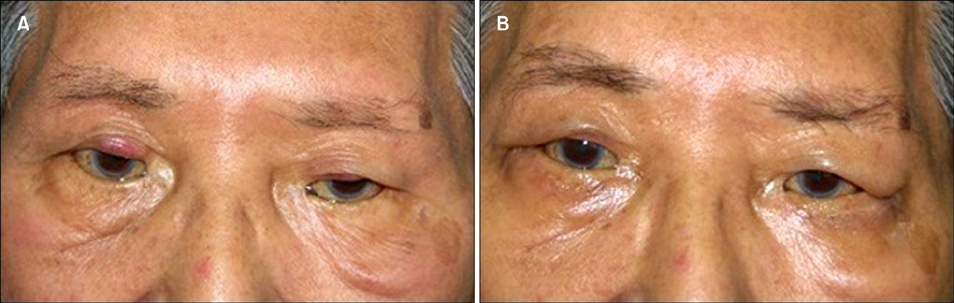
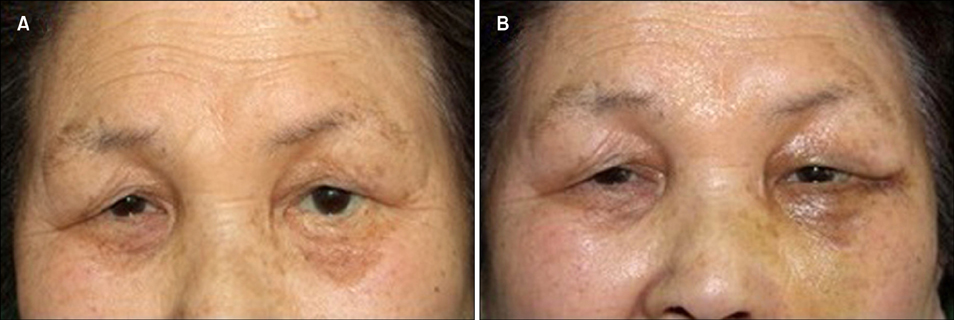
In the 44 eyelids, recurrence was observed in 5 cases (5/44, 11.4%). There were no serious postoperative complications except mild size discrepancy of both eyes. Most patients were satisfied with the results and mean satisfaction scale was 2.6/3.
CONCLUSION
The lateral tarsal strip is a simple, safe, and effective treatment method for the dermatologic surgeon to correct paralytic ectropion of mild to moderate degree in patients with leprosy.
Keyword
MeSH Terms
Figure
Reference
-
1. Vallabhanath P, Carter SR. Ectropion and entropion. Curr Opin Ophthalmol. 2000; 11:345–351.
Article2. Lee DJ, Rea TH, Modlin RL. Leprosy. In : Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, Wolff K, editors. Fitzpatrick's dermatology in general medicine. 8th ed. New York: McGraw-Hill;2012. p. 2253–2263.3. Foffrion VC. Ocular leprosy. In : Hastings RC, editor. Leprosy. 2nd ed. New York: Churchill Livingstone;1994. p. 353–357.4. Lewallen S, Tungpakorn NC, Kim SH, Courtright P. Progression of eye disease in “cured” leprosy patients: implications for understanding the pathophysiology of ocular disease and for addressing eyecare needs. Br J Ophthalmol. 2000; 84:817–821.
Article5. Moe KS, Linder T. The lateral transorbital canthopexy for correction and prevention of ectropion: report of a procedure, grading system, and outcome study. Arch Facial Plast Surg. 2000; 2:9–15.
Article6. Malik AN, Morris RW, Ffytche TJ. The prevalence of ocular complications in leprosy patients seen in the United Kingdom over a period of 21 years. Eye (Lond). 2011; 25:740–745.
Article7. Kim KH, Chung IY, Seo SW. The effect of augmented lateral tarsal strip for paralytic ectropion in leprosy patients. J Korean Ophthalmol Soc. 2009; 50:497–504.
Article8. Bosniak SL. Ectropion. In : Smith BC, Della Rocca RC, Nesi FA, Lisman RD, editors. Ophthalmic plastic and reconstructive surgery. St. Louis: Mosby;1987. p. 562–568.9. Anderson RL, Gordy DD. The tarsal strip procedure. Arch Ophthalmol. 1979; 97:2192–2196.
Article10. Jordan DR, Anderson RL. The lateral tarsal strip revisited. The enhanced tarsal strip. Arch Ophthalmol. 1989; 107:604–606.11. Barrett RV, Meyer DR. The modified Bick quick strip procedure for surgical treatment of eyelid malposition. Ophthal Plast Reconstr Surg. 2012; 28:294–299.
Article12. Townsend DJ. Eyelid malposition. In : Borodic GE, Townsend DJ, editors. Atlas of eyelid surgery. Philadelphia: W.B. Saunders;1994. p. 121–127.13. Putterman AM. Cheek-Midface lift. In : Fagien S, editor. Putterman's cosmetic oculoplastic surgery. 4th ed. Philadelphia: W.B. Saunders;2008. p. 187–203.14. Anderson RL. Tarsal strip procedure for correction of eyelid laxity and canthal malposition in the anophthalmic socket. Ophthalmology. 1981; 88:895–903.
Article15. Liu D. Lower eyelid tightening: a comparative study. Ophthal Plast Reconstr Surg. 1997; 13:199–203.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Lateral tarsal strip operation for the correction of paralytic and involutional Ectropion in Sorokdo Leprosy Patients
- Reappraisal of the lateral tarsal strip in the treatment of paralytic ectropion
- The Effect of Augmented Lateral Tarsal Strip for Paralytic Ectropion in Leprosy Patients
- Spacer graft using deep temporal fascia in the treatment of paralytic ectropion
- Involutional Ectropion Repair with the Modified Medial Spindle and the Lateral Tarsal Strip Procedure