J Breast Cancer.
2011 Sep;14(3):247-250.
Invasive Lobular Breast Cancer Presenting an Unusual Metastatic Pattern in the Form of Peritoneal and Rectal Metastases: A Case Report
- Affiliations
-
- 1Department of Radiology and Magnetic Resonance Imaging, University Clinical Center of Serbia, Belgrade, School of Medicine, University of Belgrade, Belgrade, Serbia. jelenadjokic2003@yahoo.co.uk
- 2First Surgical University Hospital, University Clinical Center, Belgrade, School of Medicine, University of Belgrade, Belgrade, Serbia.
- 3Institute for Oncology and Radiology, Belgrade, Belgrade, Serbia.
- 4Institute for Nuclear Medicine, University Clinical Center of Serbia, Belgrade, School of Medicine, University of Belgrade, Belgrade, Serbia.
- 5Department of Pathology, First Surgical University Hospital, Clinical Center of Serbia, Belgrade, Serbia, School of Medicine, University of Belgrade, Belgrade, Serbia.
Abstract
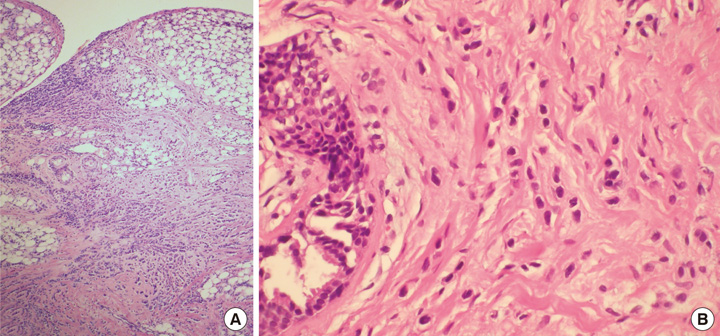
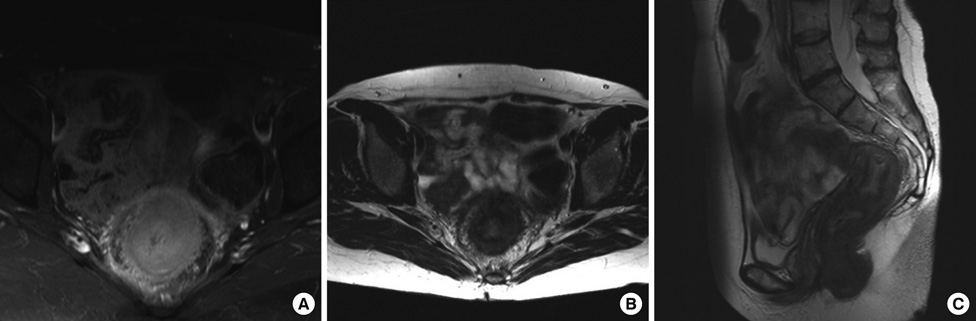
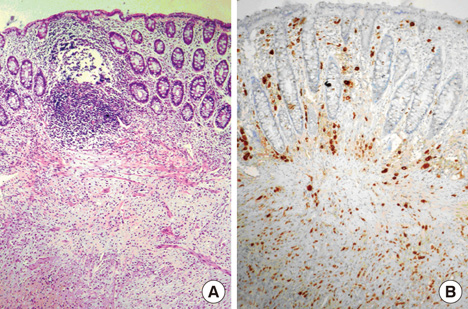
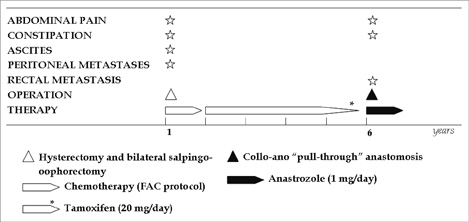
- Gastrointestinal metastases from invasive lobular breast cancer are uncommon with the stomach and small intestines being the most common metastatic sites. Peritoneal and rectal metastases are very rare and only rarely occur as the first manifestation of disease. We herein report the case of a 47-year-old woman who presented with abdominal carcinomatosis as a first sign of invasive lobular breast carcinoma (ILC). Identifying the most important immunohistochemical markers for ILC: gross cystic disease fluid protein 15, estrogen and progesterone receptors enabled a correct diagnosis. After a six year disease-free period, relapse occurred with severe obstruction due to rectal metastasis from lobular breast carcinoma. Since there was no widespread metastatic disease, surgery with concomitant hormonal therapy was performed.
Keyword
MeSH Terms
Figure
Reference
-
1. Winston CB, Hadar O, Teitcher JB, Caravelli JF, Sklarin NT, Panicek DM, et al. Metastatic lobular carcinoma of the breast: patterns of spread in the chest, abdomen, and pelvis on CT. AJR Am J Roentgenol. 2000. 175:795–800.2. Sickles EA. The subtle and atypical mammographic features of invasive lobular carcinoma. Radiology. 1991. 178:25–26.
Article3. Sato T, Ohwada A, Miyaji A, Miyazaki R, Suzuki M, Matsumoto T. Immunohistochemistry for the differentiation of peritoneal disseminated carcinoma of unknown origin. Intern Med. 2004. 43:415–419.
Article4. Berx G, Cleton-Jansen AM, Strumane K, de Leeuw WJ, Nollet F, van Roy F, et al. E-cadherin is inactivated in a majority of invasive human lobular breast cancers by truncation mutations throughout its extracellular domain. Oncogene. 1996. 13:1919–1925.5. Venanzi FM, Soverchia L, Felicetti P, Mennecozzi M, Concetti A. HER2/neu oncogene sequence revisited. J Natl Cancer Inst. 2002. 94:1808–1809.
Article6. Sheen-Chen SM, Liu YW, Sun CK, Lin SE, Eng HL, Huang WT, et al. Abdominal carcinomatosis attributed to metastatic breast carcinoma. Dig Dis Sci. 2008. 53:3043–3045.
Article7. Tuthill M, Pell R, Guiliani R, Lim A, Gudi M, Contractor KB, et al. Peritoneal disease in breast cancer: a specific entity with an extremely poor prognosis. Eur J Cancer. 2009. 45:2146–2149.
Article8. Katz A, Saad ED, Porter P, Pusztai L. Primary systemic chemotherapy of invasive lobular carcinoma of the breast. Lancet Oncol. 2007. 8:55–62.
Article9. McLemore EC, Pockaj BA, Reynolds C, Gray RJ, Hernandez JL, Grant CS, et al. Breast cancer: presentation and intervention in women with gastrointestinal metastasis and carcinomatosis. Ann Surg Oncol. 2005. 12:886–894.
Article10. Meyers MA, McSweeney J. Secondary neoplasms of the bowel. Radiology. 1972. 105:1–11.
Article11. Raju U, Ma CK, Shaw A. Signet ring variant of lobular carcinoma of the breast: a clinicopathologic and immunohistochemical study. Mod Pathol. 1993. 6:516–520.12. Tot T. The role of cytokeratins 20 and 7 and estrogen receptor analysis in separation of metastatic lobular carcinoma of the breast and metastatic signet ring cell carcinoma of the gastrointestinal tract. APMIS. 2000. 108:467–472.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Nodular Metastatic Carcinoma from Invasive Lobular Breast Cancer
- Peritoneal and gastric metastasis from invasive lobular breast carcinoma: a case report
- Lobular Breast Carcinoma Metastasis to the Thyroid Gland: Case Report and Literature Review
- Occult Invasive Lobular Carcinoma of Breast Detected by Stomach Metastasis: A Case Report
- Lobular carcinoma in situ in sclerosing adenosis