J Adv Prosthodont.
2017 Oct;9(5):371-380. 10.4047/jap.2017.9.5.371.
Effect of implant- and occlusal load location on stress distribution in Locator attachments of mandibular overdenture. A finite element study
- Affiliations
-
- 1Department of Prosthodontics and Occlusion, School of Dentistry, University of Oviedo, Oviedo, Spain. arenal@uniovi.es
- 2Department of Oral Stomatology I. Faculty of Medicine and Dentistry, University of Basque Country, Bilbao, Spain.
- KMID: 2393223
- DOI: http://doi.org/10.4047/jap.2017.9.5.371
Abstract
- PURPOSE
The aim of this study is to evaluate and compare the stress distribution in Locator attachments in mandibular two-implant overdentures according to implant locations and different loading conditions.
MATERIALS AND METHODS
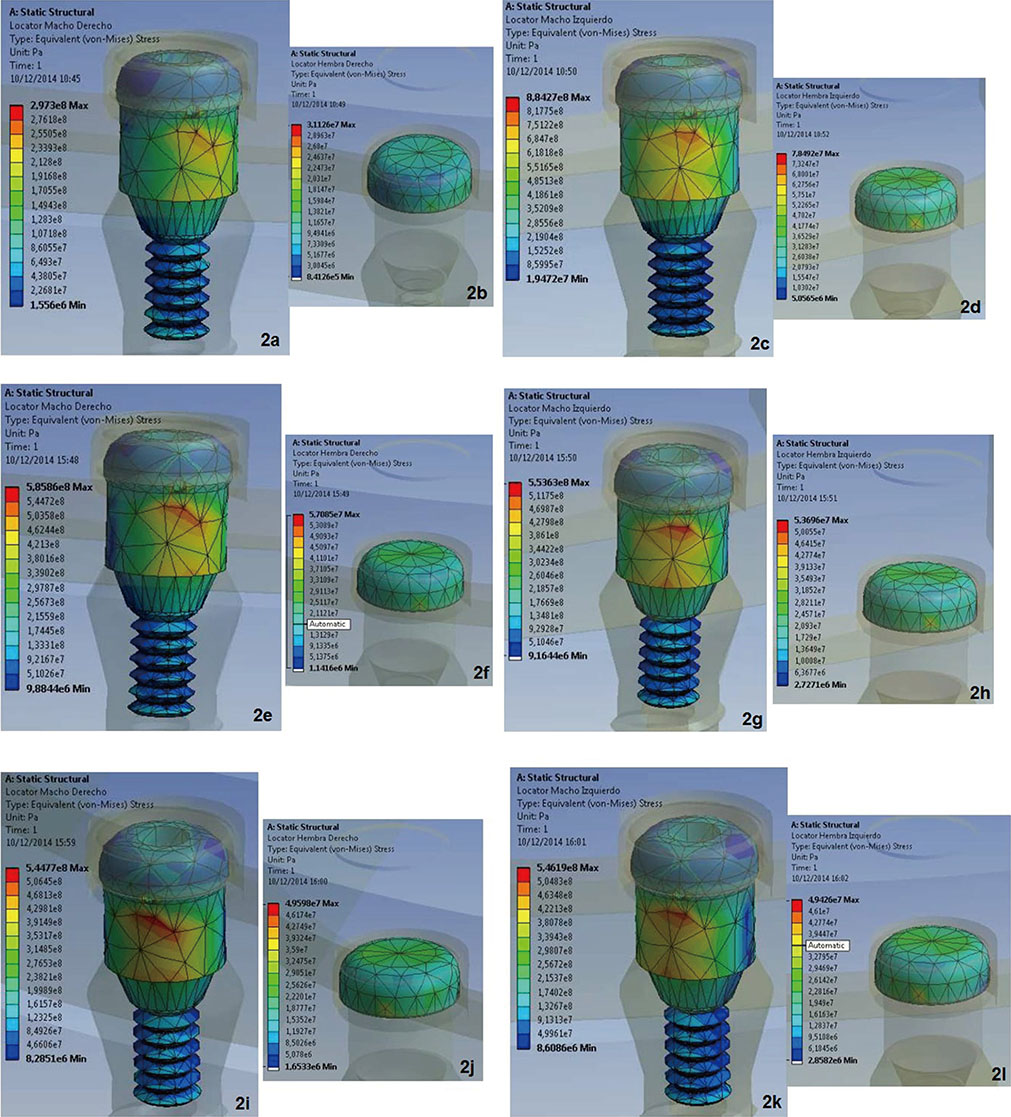
Four three-dimensional finite element models were created, simulating two osseointegrated implants in the mandible to support two Locator attachments and an overdenture. The models simulated an overdenture with implants located in the position of the level of lateral incisors, canines, second premolars, and crossed implant. A 150 N vertical unilateral and bilateral load was applied at different locations and 40 N was also applied when combined with anterior load at the midline. Data for von Mises stresses in the abutment (matrix) of the attachment and the plastic insert (patrix) of the attachment were produced numerically, color-coded, and compared between the models for attachments and loading conditions.
RESULTS
Regardless of the load, the greatest stress values were recorded in the overdenture attachments with implants at lateral incisor locations. In all models and load conditions, the attachment abutment (matrix) withstood a much greater stress than the insert plastic (patrix). Regardless of the model, when a unilateral load was applied, the load side Locator attachments recorded a much higher stress compared to the contralateral side. However, with load bilateral posterior alone or combined at midline load, the stress distribution was more symmetrical. The stress is distributed primarily in the occlusal and lateral surface of the insert plastic patrix and threadless area of the abutment (matrix).
CONCLUSION
The overdenture model with lateral incisor level implants is the worst design in terms of biomechanical environment for the attachment components. The bilateral load in general favors a more uniform stress distribution in both attachments compared to a much greater stress registered with unilateral load in the load side attachments. Regardless of the implant positions and the occlusal load application site, the stress transferred to the insert plastic is much lower than that registered in the abutment.
Figure
Reference
-
1. Dantas Ide S, Souza MB, Morais MH, Carreiro Ada F, Barbosa GA. Success and survival rates of mandibular overdentures supported by two or four implants: a systematic review. Braz Oral Res. 2014; 28:74–80.2. Kern JS, Kern T, Wolfart S, Heussen N. A systematic review and meta-analysis of removable and fixed implant-supported prostheses in edentulous jaws: post-loading implant loss. Clin Oral Implants Res. 2016; 27:174–195.3. Awad MA, Rashid F, Feine JS. Overdenture Effectiveness Study Team Consortium. The effect of mandibular 2-implant overdentures on oral health-related quality of life: an international multicentre study. Clin Oral Implants Res. 2014; 25:46–51.4. Harris D, Höfer S, O'Boyle CA, Sheridan S, Marley J, Benington IC, Clifford T, Houston F, O'Connell B. A comparison of implant-retained mandibular overdentures and conventional dentures on quality of life in edentulous patients: a randomized, prospective, within-subject controlled clinical trial. Clin Oral Implants Res. 2013; 24:96–103.5. Thomason JM. The use of mandibular implant-retained overdentures improve patient satisfaction and quality of life. J Evid Based Dent Pract. 2012; 12:182–184.6. Hobkirk JA, Abdel-Latif HH, Howlett J, Welfare R, Moles DR. Prosthetic treatment time and satisfaction of edentulous patients treated with conventional or implant-stabilized complete mandibular dentures: a case-control study (part 2). Int J Prosthodont. 2009; 22:13–19.7. Feine JS, Carlsson GE, Awad MA, Chehade A, Duncan WJ, Gizani S, Head T, Lund JP, MacEntee M, Mericske-Stern R, Mojon P, Morais J, Naert I, Payne AG, Penrod J, Stoker GT, Tawse-Smith A, Taylor TD, Thomason JM, Thomson WM, Wismeijer D. The McGill consensus statement on overdentures Mandibular two-implant overdentures as first choice standard of care for edentulous patients. Montreal, Quebec, May 24-25, 2002. Int J Oral Maxillofac Implants. 2002; 17:601–602.8. Thomason JM, Feine J, Exley C, Moynihan P, Müller F, Naert I, Ellis JS, Barclay C, Butterworth C, Scott B, Lynch C, Stewardson D, Smith P, Welfare R, Hyde P, McAndrew R, Fenlon M, Barclay S, Barker D. Mandibular two implant-supported overdentures as the first choice standard of care for edentulous patients-the York Consensus Statement. Br Dent J. 2009; 207:185–186.9. Hong HR, Pae A, Kim Y, Paek J, Kim HS, Kwon KR. Effect of implant position, angulation, and attachment height on peri-implant bone stress associated with mandibular two-implant overdentures: a finite element analysis. Int J Oral Maxillofac Implants. 2012; 27:e69–e76.10. Taylor TD. Indications and treatment planning for mandibular implant overdentures. In : Feine JS, Carlsson GE, editors. Implant Overdentures as the Standard of Care for Edentulous Patients. Chicago: Quintessence;2003. p. 71–81.11. Elsyad MA, Hammouda NI. Expansion of mandibular knifeedge ridge and simultaneous implant placement to retain overdentures: One-year clinical and radiographic results of a prospective study. Clin Implant Dent Relat Res. 2017; 19:167–179.12. Thomason JM. The use of mandibular implant-retained overdentures improve patient satisfaction and quality of life. J Evid Based Dent Pract. 2010; 10:61–63.13. Ellis JS, Burawi G, Walls A, Thomason JM. Patient satisfaction with two designs of implant supported removable overdentures; ball attachment and magnets. Clin Oral Implants Res. 2009; 20:1293–1298.14. Carlsson GE. Implant and root supported overdentures - a literature review and some data on bone loss in edentulous jaws. J Adv Prosthodont. 2014; 6:245–252.15. Cakarer S, Can T, Yaltirik M, Keskin C. Complications associated with the ball, bar and Locator attachments for implant-supported overdentures. Med Oral Patol Oral Cir Bucal. 2011; 16:e953–e959.16. Ozan O, Ramoglu S. Effect of implant height differences on different attachment types and peri-implant bone in mandibular two-implant overdentures: 3D finite element study. J Oral Implantol. 2015; 41:e50–e59.17. Cristache CM, Muntianu LA, Burlibasa M, Didilescu AC. Five-year clinical trial using three attachment systems for implant overdentures. Clin Oral Implants Res. 2014; 25:e171–e178.18. Elsyad MA, Agha NN, Habib AA. Retention and stability of implant-retained mandibular overdentures using different types of resilient attachments: An in vitro study. Int J Oral Maxillofac Implants. 2016; 31:1040–1048.19. Kleis WK, Kämmerer PW, Hartmann S, Al-Nawas B, Wagner W. A comparison of three different attachment systems for mandibular two-implant overdentures: one-year report. Clin Implant Dent Relat Res. 2010; 12:209–218.20. Chung KH, Chung CY, Cagna DR, Cronin RJ Jr. Retention characteristics of attachment systems for implant overdentures. J Prosthodont. 2004; 13:221–226.21. Uludag B, Polat S, Sahin V, Çomut AA. Effects of implant angulations and attachment configurations on the retentive forces of locator attachment-retained overdentures. Int J Oral Maxillofac Implants. 2014; 29:1053–1057.22. Daas M, Dubois G, Bonnet AS, Lipinski P, Rignon-Bret C. A complete finite element model of a mandibular implant-retained overdenture with two implants: comparison between rigid and resilient attachment configurations. Med Eng Phys. 2008; 30:218–225.23. Arat Bilhan S, Bilhan H, Bozdag E, Sunbuloglu E, Baykasoglu C, Kutay O. The influence of the attachment type and implant number supporting mandibular overdentures on stress distribution: an in vitro study, part I. Implant Dent. 2013; 22:39–48.24. Kuoppala R, Näpänkangas R, Raustia A. Quality of Life of Patients Treated With Implant-Supported Mandibular Overdentures Evaluated With the Oral Health Impact Profile (OHIP-14): a Survey of 58 Patients. J Oral Maxillofac Res. 2013; 4:e4.25. Roccuzzo M, Bonino F, Gaudioso L, Zwahlen M, Meijer HJ. What is the optimal number of implants for removable reconstructions? A systematic review on implant-supported overdentures. Clin Oral Implants Res. 2012; 23:229–237.26. Engelhardt F, Zeman F, Behr M, Hahmel S. Prosthetic complications and maintenance requirements in locator-attached implant-supported overdentures: A retrospective study. Eur J Prosthodont Restor Dent. 2016; 24:31–35.27. Andreiotelli M, Att W, Strub JR. Prosthodontic complications with implant overdentures: a systematic literature review. Int J Prosthodont. 2010; 23:195–203.28. Liu J, Pan S, Dong J, Mo Z, Fan Y, Feng H. Influence of implant number on the biomechanical behaviour of mandibular implant-retained/supported overdentures: a three-dimensional finite element analysis. J Dent. 2013; 41:241–249.29. Gross MD. Occlusion in implant dentistry. A review of the literature of prosthetic determinants and current concepts. Aust Dent J. 2008; 53:S60–S68.30. Kim Y, Oh TJ, Misch CE, Wang HL. Occlusal considerations in implant therapy: clinical guidelines with biomechanical rationale. Clin Oral Implants Res. 2005; 16:26–35.31. Mericske-Stern RD, Taylor TD, Belser U. Management of the edentulous patient. Clin Oral Implants Res. 2000; 11:108–125.32. Petropoulos VC, Smith W. Maximum dislodging forces of implant overdenture stud attachments. Int J Oral Maxillofac Implants. 2002; 17:526–535.33. Rutkunas V, Mizutani H, Takahashi H. Influence of attachment wear on retention of mandibular overdenture. J Oral Rehabil. 2007; 34:41–51.34. Lekholm U, Zarb GA. Patient selection and preparation. In : Brånemak PI, Zarb GA, Albrektsson T, editors. Tissue integrated prostheses: osseointegration in clinical dentistry. Chicago: Quintessence;1985. p. 199–210.35. Rentsch-Kollar A, Huber S, Mericske-Stern R. Mandibular implant overdentures followed for over 10 years: patient compliance and prosthetic maintenance. Int J Prosthodont. 2010; 23:91–98.36. Dashti MH, Atashrazm P, Emadi MI, Mishaeel S, Banava S. The effects of two attachment types on the stresses introduced to the mandibular residual ridge: a 3D finite element analysis. Quintessence Int. 2013; 44:585–590.37. Kono K, Kurihara D, Suzuki Y, Ohkubo C. In vitro assessment of mandibular single/two implant-retained overdentures using stress-breaking attachments. Implant Dent. 2014; 23:456–462.38. Geng JP, Tan KB, Liu GR. Application of finite element analysis in implant dentistry: a review of the literature. J Prosthet Dent. 2001; 85:585–598.39. Greco GD, Jansen WC, Landre Junior J, Seraidarian PI. Biomechanical analysis of the stresses generated by different disocclusion patterns in an implant-supported mandibular complete denture. J Appl Oral Sci. 2009; 17:515–520.40. Baggi L, Cappelloni I, Di Girolamo M, Maceri F, Vairo G. The influence of implant diameter and length on stress distribution of osseointegrated implants related to crestal bone geometry: a three-dimensional finite element analysis. J Prosthet Dent. 2008; 100:422–431.41. Chun HJ, Park DN, Han CH, Heo SJ, Heo MS, Koak JY. Stress distributions in maxillary bone surrounding overdenture implants with different overdenture attachments. J Oral Rehabil. 2005; 32:193–205.42. de Almeida EO, Rocha EP, Assunção WG, Júnior AC, Anchieta RB. Cortical bone stress distribution in mandibles with different configurations restored with prefabricated barprosthesis protocol: a three-dimensional finite-element analysis. J Prosthodont. 2011; 20:29–34.43. Ebadian B, Farzin M, Talebi S, Khodaeian N. Evaluation of stress distribution of implant-retained mandibular overdenture with different vertical restorative spaces: A finite element analysis. Dent Res J (Isfahan). 2012; 9:741–747.44. Chung KH, Whiting D, Kronstrom M, Chan D, Wataha J. Retentive characteristics of overdenture attachments during repeated dislodging and cyclic loading. Int J Prosthodont. 2011; 24:127–129.45. Stergiou A, Juszczyk AS, Clark RK, Radford DR. The retentive forces of the locator attachment system at different angulations. Eur J Prosthodont Restor Dent. 2012; 20:168–174.46. Al-Ghafli SA, Michalakis KX, Hirayama H, Kang K. The in vitro effect of different implant angulations and cyclic dislodgement on the retentive properties of an overdenture attachment system. J Prosthet Dent. 2009; 102:140–147.47. Rabbani S, Juszczyk AS, Clark RK, Radford DR. Investigation of retentive force reduction and wear of the locator attachment system with different implant angulations. Int J Oral Maxillofac Implants. 2015; 30:556–563.48. Barão VA, Delben JA, Lima J, Cabral T, Assunção WG. Comparison of different designs of implant-retained overdentures and fixed full-arch implant-supported prosthesis on stress distribution in edentulous mandible-a computed tomography-based three-dimensional finite element analysis. J Biomech. 2013; 46:1312–1320.49. Elsyad MA, Setta FA, Khirallah AS. Strains around distally inclined implants retaining mandibular overdentures with Locator attachments: an in vitro study. J Adv Prosthodont. 2016; 8:116–124.50. Jayaraman S, Mallan S, Rajan B, Anachaperumal MP. Three-dimensional finite element analysis of immediate loading mini over denture implants with and without acrylonitrile O-ring. Indian J Dent Res. 2012; 23:840–841.51. Tanino F, Hayakawa I, Hirano S, Minakuchi S. Finite element analysis of stress-breaking attachments on maxillary implant-retained overdentures. Int J Prosthodont. 2007; 20:193–198.52. Geering AH, Kundert M. Total-und hybridprothetik. Stuttgart: Thieme Verlag;1986.53. Budtz-Jorgensen E. Prosthodontics for the elderly. Diagnosis and treatment. Chicago: Quintessence;1999.54. Anusavice KJ, Shen Ch, Rawls HR. Phillips' science of dental materials. St. Louis: Elsevier;2013. p. 365–395.55. Petrie CS, Walker MP, Lu Y, Thiagarajan G. A preliminary three-dimensional finite element analysis of mandibular implant overdentures. Int J Prosthodont. 2014; 27:70–72.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Finite Element Analysis of Stress Distribution on Telescopic System for Mandibular Implant Supported Overdenture
- Effect of attachments and palatal coverage of maxillary implant overdenture on stress distribution: a finite element analysis
- 3D finite element analysis of overdenture stability and stress distribution on mandibular implant-retained overdenture
- Finite element stress analysis of maxillary two implants-retained overdenture according go position of implant fixtures
- Comparative evaluation of peri-implant stress distribution in implant protected occlusion and cuspally loaded occlusion on a 3 unit implant supported fixed partial denture: A 3D finite element analysis study