Ann Surg Treat Res.
2017 Jul;93(1):35-42. 10.4174/astr.2017.93.1.35.
Long-term oncologic outcomes of laparoscopic surgery for splenic flexure colon cancer are comparable to conventional open surgery
- Affiliations
-
- 1Department of Surgery, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. jgkim@catholic.ac.kr
- 2Department of Surgery, Yeouido St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 3Department of Surgery, St. Vincent Hospital, College of Medicine, The Catholic University of Korea, Suwon, Korea.
- KMID: 2392281
- DOI: http://doi.org/10.4174/astr.2017.93.1.35
Abstract
- PURPOSE
Few studies about laparoscopic surgery for splenic flexure colon cancer have been published. This study aims to compare the short- and long-term outcomes of laparoscopic surgery for splenic flexure colon cancer with those of conventional open surgery.
METHODS
From January 2004 to December 2010, 51 consecutive patients who underwent curative resection for stages I-III splenic flexure colon cancer were enrolled. Thirty-three patients underwent laparoscopy-assisted colectomy, while 18 patients underwent conventional open colectomy. Short- and long-term outcomes of the 2 groups were compared.
RESULTS
There were no differences in baseline characteristics, intra- and postoperative complications. The laparoscopy group showed longer operation time (median [interquartile range, IQR]: 295.0 [255.0-362.5] minutes vs. 180.0 [168.8-206.3] minutes, P < 0.001). In the laparoscopy group, return of bowel function was faster (median [IQR]: 3 [2-4] vs. 4 [3-5], P = 0.007) and postoperative hospital stay was shorter (median [IQR]: 9 [8-11] vs. 10.5 [9-19], P = 0.026). There were no statistically significant differences in overall survival rate (84.3% vs. 76.0%, P = 0.560) or disease-free survival rate (93.8% vs. 74.5%, P = 0.078) between the 2 groups.
CONCLUSION
Laparoscopic surgery for splenic flexure colon cancer has better short-term outcomes than open surgery, as well as acceptable long-term outcomes. Laparoscopic surgery can be a safe and feasible alternative to conventional open surgery for splenic flexure colon cancer.
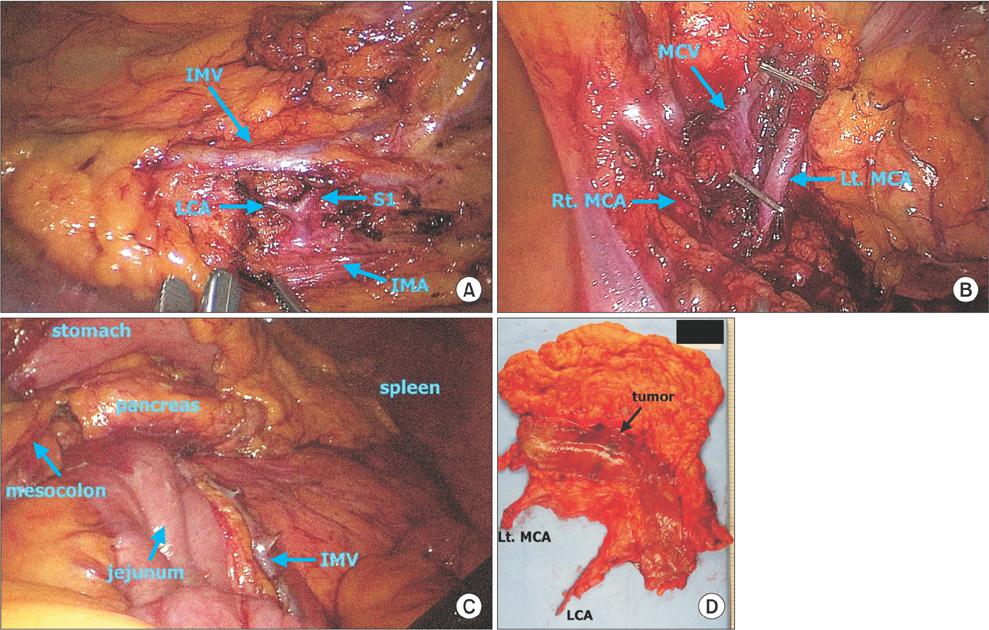
Figure
Reference
-
1. Fleshman J, Sargent DJ, Green E, Anvari M, Stryker SJ, Beart RW Jr, et al. Laparoscopic colectomy for cancer is not inferior to open surgery based on 5-year data from the COST Study Group trial. Ann Surg. 2007; 246:655–662.2. Green BL, Marshall HC, Collinson F, Quirke P, Guillou P, Jayne DG, et al. Long-term follow-up of the Medical Research Council CLASICC trial of conventional versus laparoscopically assisted resection in colorectal cancer. Br J Surg. 2013; 100:75–82.3. Colon Cancer Laparoscopic or Open Resection Study Group. Buunen M, Veldkamp R, Hop WC, Kuhry E, Jeekel J, et al. Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol. 2009; 10:44–52.4. Lacy AM, Delgado S, Castells A, Prins HA, Arroyo V, Ibarzabal A, et al. The long-term results of a randomized clinical trial of laparoscopy-assisted versus open surgery for colon cancer. Ann Surg. 2008; 248:1–7.5. Hohenberger W, Weber K, Matzel K, Papadopoulos T, Merkel S. Standardized surgery for colonic cancer: complete mesocolic excision and central ligation--technical notes and outcome. Colorectal Dis. 2009; 11:354–364.6. Benseler V, Hornung M, Iesalnieks I, von Breitenbuch P, Glockzin G, Schlitt HJ, et al. Different approaches for complete mobilization of the splenic flexure during laparoscopic rectal cancer resection. Int J Colorectal Dis. 2012; 27:1521–1529.7. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–213.8. Kim CW, Shin US, Yu CS, Kim JC. Clinicopathologic characteristics, surgical treatment and outcomes for splenic flexure colon cancer. Cancer Res Treat. 2010; 42:69–76.9. Levien DH, Gibbons S, Begos D, Byrne DW. Survival after resection of carcinoma of the splenic flexure. Dis Colon Rectum. 1991; 34:401–403.10. Griffiths JD. Surgical anatomy of the blood supply of the distal colon. Ann R Coll Surg Engl. 1956; 19:241–256.11. Jamali FR, Soweid AM, Dimassi H, Bailey C, Leroy J, Marescaux J. Evaluating the degree of difficulty of laparoscopic colorectal surgery. Arch Surg. 2008; 143:762–767.12. Akiyoshi T, Kuroyanagi H, Oya M, Ueno M, Fujimoto Y, Konishi T, et al. Factors affecting difficulty of laparoscopic surgery for left-sided colon cancer. Surg Endosc. 2010; 24:2749–2754.13. Pisani Ceretti A, Maroni N, Sacchi M, Bona S, Angiolini MR, Bianchi P, et al. Laparoscopic colonic resection for splenic flexure cancer: our experience. BMC Gastroenterol. 2015; 15:76.14. Fiscon V, Portale G, Migliorini G, Frigo F. Splenic flexure colon cancers: minimally invasive treatment. Updates Surg. 2015; 67:55–59.15. Nakashima M, Akiyoshi T, Ueno M, Fukunaga Y, Nagayama S, Fujimoto Y, et al. Colon cancer in the splenic flexure: comparison of short-term outcomes of laparoscopic and open colectomy. Surg Laparosc Endosc Percutan Tech. 2011; 21:415–418.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Long-term Survival for Laparoscopic-assisted Surgery and Open Surgery for Right Colon Cancer: A Case-Control Study
- Three Surgical Approaches of Laparoscopic Splenic Flexure Mobilization
- Laparoscopic Surgery for Splenic Flexure Colon Cancer
- Short- and long-term outcomes of laparoscopic segmental left colectomy for splenic flexure colon cancer: comparison with propensity score matching
- Laparoscopic Colectomy : Present and Future