Pediatr Gastroenterol Hepatol Nutr.
2017 Sep;20(3):153-159. 10.5223/pghn.2017.20.3.153.
Not All Children with Cystic Fibrosis Have Abnormal Esophageal Neutralization during Chemical Clearance of Acid Reflux
- Affiliations
-
- 1Division of Gastroenterology, Hepatology and Nutrition, Nationwide Children's Hospital, Columbus, OH, USA. Frederick.Woodley@nationwidechildrens.org
- 2Department of Pediatrics, The Ohio State University College of Medicine, Columbus, OH, USA.
- 3Biostatistics Core, Nationwide Children's Hospital, Columbus, OH, USA.
- 4Department of Pediatrics, Federal University of Sao Paulo, Sao Paulo, Brazil.
- 5Division of Pulmonary Medicine, Nationwide Children's Hospital, Columbus, OH, USA.
- 6Research Institute and Neonatology, Nationwide Children's Hospital, Columbus, OH, USA.
- 7Division of Gastroenterology, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, USA.
- 8Department of Pediatrics, OSU University of Cincinnati College of Medicine, Cincinnati, OH, USA.
- 9Division of Gastroenterology, Rady Children's Hospital, San Diego, CA, USA.
- 10Department of Pediatrics, The University of California at San Diego College of Medicine, San Diego, CA, USA.
- KMID: 2390546
- DOI: http://doi.org/10.5223/pghn.2017.20.3.153
Abstract
- PURPOSE
Acid neutralization during chemical clearance is significantly prolonged in children with cystic fibrosis, compared to symptomatic children without cystic fibrosis. The absence of available reference values impeded identification of abnormal findings within individual patients with and without cystic fibrosis. The present study aimed to test the hypothesis that significantly more children with cystic fibrosis have acid neutralization durations during chemical clearance that fall outside the physiological range.
METHODS
Published reference value for acid neutralization duration during chemical clearance (determined using combined impedance/pH monitoring) was used to assess esophageal acid neutralization efficiency during chemical clearance in 16 children with cystic fibrosis (3 to <18 years) and 16 age-matched children without cystic fibrosis.
RESULTS
Duration of acid neutralization during chemical clearance exceeded the upper end of the physiological range in 9 of 16 (56.3%) children with and in 3 of 16 (18.8%) children without cystic fibrosis (p=0.0412). The likelihood ratio for duration indicated that children with cystic fibrosis are 2.1-times more likely to have abnormal acid neutralization during chemical clearance, and children with abnormal acid neutralization during chemical clearance are 1.5-times more likely to have cystic fibrosis.
CONCLUSION
Significantly more (but not all) children with cystic fibrosis have abnormally prolonged esophageal clearance of acid. Children with cystic fibrosis are more likely to have abnormal acid neutralization during chemical clearance. Additional studies involving larger sample sizes are needed to address the importance of genotype, esophageal motility, composition and volume of saliva, and gastric acidity on acid neutralization efficiency in cystic fibrosis children.
MeSH Terms
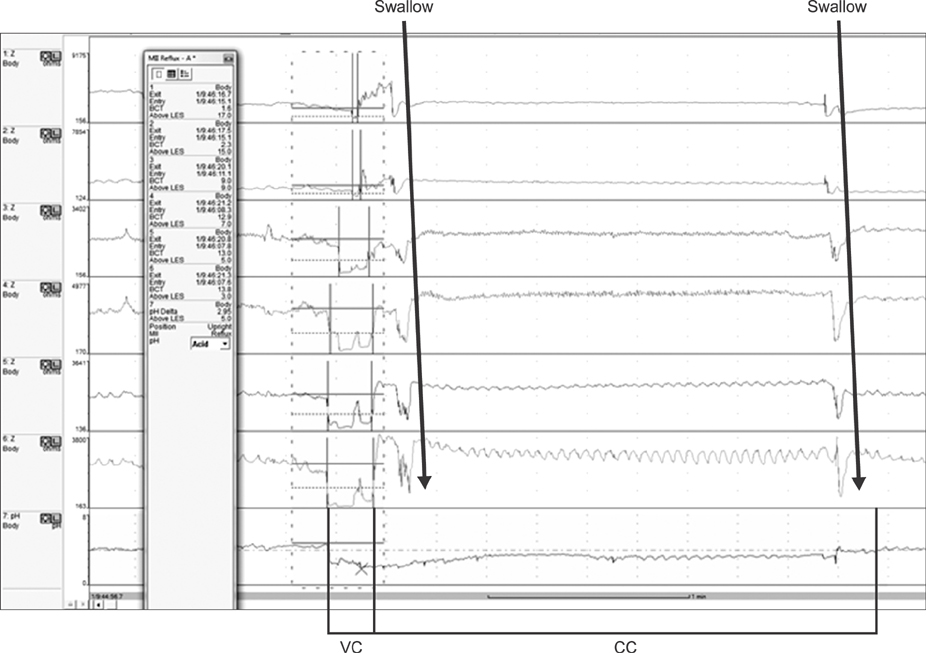
Figure
Reference
-
1. Simrén M, Silny J, Holloway R, Tack J, Janssens J, Sifrim D. Relevance of ineffective oesophageal motility during oesophageal acid clearance. Gut. 2003; 52:784–790.
Article2. Helm JF, Dodds WJ, Pelc LR, Palmer DW, Hogan WJ, Teeter BC. Effect of esophageal emptying and saliva on clearance of acid from the esophagus. N Engl J Med. 1984; 310:284–288.
Article3. Boyd DD, Carney CN, Powell DW. Neurohumoral control of esophageal epithelial electrolyte transport. Am J Physiol. 1980; 239:G5–G11.
Article4. Hamilton BH, Orlando RC. In vivo alkaline secretion by mammalian esophagus. Gastroenterology. 1989; 97:640–648.
Article5. Meyers RL, Orlando RC. In vivo bicarbonate secretion by human esophagus. Gastroenterology. 1992; 103:1174–1178.
Article6. Orlando RC. Esophageal mucosal defense mechanisms. Part 1 Oral cavity, pharynx, and esophagus. GI Motil Online. 2006; DOI: 10.1038/gimo15.7. Abdulnour-Nakhoul S, Nakhoul NL, Orlando RC. Lumen-to-surface pH gradients in opossum and rabbit esophagi: role of submucosal glands. Am J Physiol Gastrointest Liver Physiol. 2000; 278:G113–G120.
Article8. Abdulnour-Nakhoul S, Nakhoul HN, Kalliny MI, Gyftopoulos A, Rabon E, Doetjes R, et al. Ion transport mechanisms linked to bicarbonate secretion in the esophageal submucosal glands. Am J Physiol Regul Integr Comp Physiol. 2011; 301:R83–R96.
Article9. Sivalingam M, Sitaram S, Hasenstab KA, Wei L, Woodley FW, Jadcherla SR. Effects of esophageal acidification on troublesome symptoms: an approach to characterize true acid GERD in dysphagic neonates. Dysphagia. 2017; 32:509–519.
Article10. Frazzoni M, Manta R, Mirante VG, Conigliaro R, Frazzoni L, Melotti G. Esophageal chemical clearance is impaired in gastro-esophageal reflux disease--a 24-h impedance-pH monitoring assessment. Neurogastroenterol Motil. 2013; 25:399–406.11. Vaezi MF, Singh S, Richter JE. Role of acid and duodenogastric reflux in esophageal injury: a review of animal and human studies. Gastroenterology. 1995; 108:1897–1907.
Article12. Tuttle SG, Rufin F, Bettarello A. The physiology of heartburn. Ann Intern Med. 1961; 55:292–300.
Article13. Pauwels A, Blondeau K, Mertens V, Farre R, Verbeke K, Dupont LJ, et al. Gastric emptying and different types of reflux in adult patients with cystic fibrosis. Aliment Pharmacol Ther. 2011; 34:799–807.
Article14. Pauwels A, Decraene A, Blondeau K, Mertens V, Farre R, Proesmans M, et al. Bile acids in sputum and increased airway inflammation in patients with cystic fibrosis. Chest. 2012; 141:1568–1574.
Article15. Woodley FW, Machado RS, Hayes D Jr, Di Lorenzo C, Kaul A, Skaggs B, et al. Children with cystic fibrosis have prolonged chemical clearance of acid reflux compared to symptomatic children without cystic fibrosis. Dig Dis Sci. 2014; 59:623–630.
Article16. Woodley FW, Machado R, Di Lorenzo C, Mousa H. Chemical clearance in infants and children with acid reflux in the physiologic range. J Pediatr Gastroenterol Nutr. 2015; 60:783–786.
Article17. Pauwels A, Blondeau K, Dupont LJ, Sifrim D. Mechanisms of increased gastroesophageal reflux in patients with cystic fibrosis. Am J Gastroenterol. 2012; 107:1346–1353.
Article18. Navarro J, Rainisio M, Harms HK, Hodson ME, Koch C, Mastella G, et al. Factors associated with poor pulmonary function: cross-sectional analysis of data from the ERCF. Eur Respir J. 2001; 18:298–305.
Article19. Dodds WJ, Dent J, Hogan WJ, Helm JF, Hauser R, Patel GK, et al. Mechanisms of gastroesophageal reflux in patients with reflux esophagitis. N Engl J Med. 1982; 307:1547–1552.
Article20. Richter J. Do we know the cause of reflux disease? Eur J Gastroenterol Hepatol. 1999; 11:Suppl 1. S3–S9.
Article21. Orlando RC. Overview of the mechanisms of gastroesophageal reflux. Am J Med. 2001; 111:Suppl 8A. 174S–177S.
Article22. Maclean JE, Solomon M, Corey M, Selvadurai H. Cystic fibrosis newborn screening does not delay the identification of cystic fibrosis in children with negative results. J Cyst Fibros. 2011; 10:333–337.
Article23. Martinucci I, de Bortoli N, Savarino E, Piaggi P, Bellini M, Antonelli A, et al. Esophageal baseline impedance levels in patients with pathophysiological characteristics of functional heartburn. Neurogastroenterol Motil. 2014; 26:546–555.
Article24. Woodley FW, Fernandez S, Mousa H. Diurnal variation in the chemical clearance of acid gastroesophageal reflux in infants. Clin Gastroenterol Hepatol. 2007; 5:37–43.
Article25. Frazzoni M, Savarino E, de Bortoli N, Martinucci I, Furnari M, Frazzoni L, et al. Analyses of the post-reflux swallow-induced peristaltic wave index and nocturnal baseline impedance parameters increase the diagnostic yield of impedance-pH monitoring of patients with reflux disease. Clin Gastroenterol Hepatol. 2016; 14:40–46.
Article26. Mekus F, Ballmann M, Bronsveld I, Bijman J, Veeze H, Tümmler B. Categories of deltaF508 homozygous cystic fibrosis twin and sibling pairs with distinct phenotypic characteristics. Twin Res. 2000; 3:277–293.
Article27. Vanscoy LL, Blackman SM, Collaco JM, Bowers A, Lai T, Naughton K, et al. Heritability of lung disease severity in cystic fibrosis. Am J Respir Crit Med. 2007; 175:1036–1043.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Nocturnal Gastroesophageal Reflux Revisited by Impedance-pH Monitoring
- Esophageal Motility and Acid Clearance in Patients with Esophageal Varices
- A Study of Dual-probe Esophageal pH Meter in Children with Gastroesophageal Reflux
- Factors of Reflux Episodes With Post-reflux Swallowinduced Peristaltic Wave in Gastroesophageal Reflux Disease
- Esophageal acid clearance in patients with ineffective esophageal motility