J Korean Med Sci.
2017 Nov;32(11):1820-1827. 10.3346/jkms.2017.32.11.1820.
Lactate Parameters Predict Clinical Outcomes in Patients with Nonvariceal Upper Gastrointestinal Bleeding
- Affiliations
-
- 1Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. lhyuk.lee@samsung.com
- KMID: 2390309
- DOI: http://doi.org/10.3346/jkms.2017.32.11.1820
Abstract
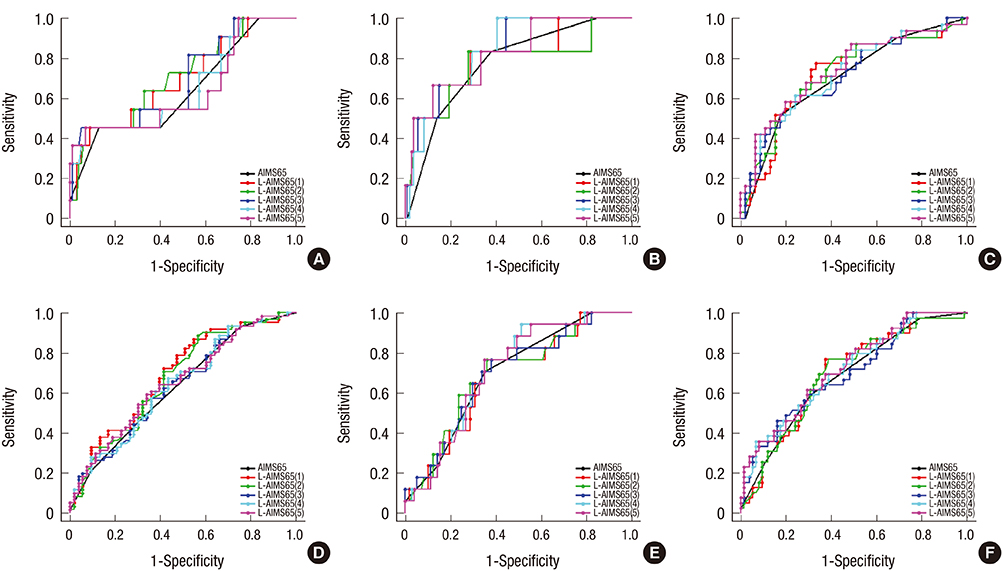
- The predictive role of lactate in patients with nonvariceal upper gastrointestinal bleeding (NVUGIB) has been suggested. This study evaluated several lactate parameters in terms of predicting outcomes of bleeding patients and sought to establish a new scoring model by combining lactate parameters and the AIMS65 score. A total of 114 patients with NVUGIB who underwent serum lactate level testing at least twice and endoscopic hemostasis within 24 hours after admission were retrospectively analyzed. The associations between five lactate parameters and clinical outcomes were evaluated and the predictive power of lactate parameter combined AIMS65s (L-AIMS65s) and AIMS56 scoring was compared. The most common cause of bleeding was gastric ulcer (48.2%). Lactate clearance rate (LCR) was associated with 30-day rebleeding (odds ratio [OR], 0.931; 95% confidence interval [CI], 0.872-0.994; P = 0.033). Initial lactate (OR, 1.313; 95% CI, 1.050-1.643; P = 0.017), maximal lactate (OR, 1.277; 95% CI, 1.037-1.573; P = 0.021), and average lactate (OR, 1.535; 95% CI, 1.137-2.072; P = 0.005) levels were associated with 30-day mortality. Initial lactate (OR, 1.213; 95% CI, 1.027-1.432; P = 0.023), maximal lactate (OR, 1.271; 95% CI, 1.074-1.504; P = 0.005), and average lactate (OR, 1.501; 95% CI, 1.150-1.959; P = 0.003) levels were associated with admission over 7 days. Although L-AIMS65s showed the highest area under the curve for prediction of each outcome, differences between L-AIMS65s and AIMS65 did not reach statistical significance. In conclusion, lactate parameters have a prognostic role in patients with NVUGIB. However, they do not increase the predictive power of AIMS65 when combined.
MeSH Terms
Figure
Reference
-
1. Button LA, Roberts SE, Evans PA, Goldacre MJ, Akbari A, Dsilva R, Macey S, Williams JG. Hospitalized incidence and case fatality for upper gastrointestinal bleeding from 1999 to 2007: a record linkage study. Aliment Pharmacol Ther. 2011; 33:64–76.2. Wu CY, Wu MS, Kuo KN, Wang CB, Chen YJ, Lin JT. Long-term peptic ulcer rebleeding risk estimation in patients undergoing haemodialysis: a 10-year nationwide cohort study. Gut. 2011; 60:1038–1042.3. Hsu YC, Lin JT, Chen TT, Wu MS, Wu CY. Long-term risk of recurrent peptic ulcer bleeding in patients with liver cirrhosis: a 10-year nationwide cohort study. Hepatology. 2012; 56:698–705.4. Gralnek IM, Dumonceau JM, Kuipers EJ, Lanas A, Sanders DS, Kurien M, Rotondano G, Hucl T, Dinis-Ribeiro M, Marmo R, et al. Diagnosis and management of nonvariceal upper gastrointestinal hemorrhage: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2015; 47:a1–a46.5. Blatchford O, Murray WR, Blatchford M. A risk score to predict need for treatment for upper-gastrointestinal haemorrhage. Lancet. 2000; 356:1318–1321.6. Rockall TA, Logan RF, Devlin HB, Northfield TC. Risk assessment after acute upper gastrointestinal haemorrhage. Gut. 1996; 38:316–321.7. Robertson M, Majumdar A, Boyapati R, Chung W, Worland T, Terbah R, Wei J, Lontos S, Angus P, Vaughan R. Risk stratification in acute upper GI bleeding: comparison of the AIMS65 score with the Glasgow-Blatchford and Rockall scoring systems. Gastrointest Endosc. 2016; 83:1151–1160.8. Martínez-Cara JG, Jiménez-Rosales R, Úbeda-Muñoz M, de Hierro ML, de Teresa J, Redondo-Cerezo E. Comparison of AIMS65, Glasgow-Blatchford score, and Rockall score in a European series of patients with upper gastrointestinal bleeding: performance when predicting in-hospital and delayed mortality. United European Gastroenterol J. 2016; 4:371–379.9. Chandra S. AIMS65 score predicts short-term mortality but not the need for intervention in acute upper GI bleeding. Gastrointest Endosc. 2013; 78:381–382.10. Andersen LW, Mackenhauer J, Roberts JC, Berg KM, Cocchi MN, Donnino MW. Etiology and therapeutic approach to elevated lactate levels. Mayo Clin Proc. 2013; 88:1127–1140.11. Wada T, Hagiwara A, Uemura T, Yahagi N, Kimura A. Early lactate clearance for predicting active bleeding in critically ill patients with acute upper gastrointestinal bleeding: a retrospective study. Intern Emerg Med. 2016; 11:737–743.12. El-Kersh K, Chaddha U, Sinha RS, Saad M, Guardiola J, Cavallazzi R. Predictive role of admission lactate level in critically Ill patients with acute upper gastrointestinal bleeding. J Emerg Med. 2015; 49:318–325.13. Ko BS, Kim WY, Ryoo SM, Ahn S, Sohn CH, Seo DW, Lee YS, Lim KS, Jung HY. Predicting the occurrence of hypotension in stable patients with nonvariceal upper gastrointestinal bleeding: point-of-care lactate testing. Crit Care Med. 2015; 43:2409–2415.14. Shah A, Chisolm-Straker M, Alexander A, Rattu M, Dikdan S, Manini AF. Prognostic use of lactate to predict inpatient mortality in acute gastrointestinal hemorrhage. Am J Emerg Med. 2014; 32:752–755.15. Levy B, Sadoune LO, Gelot AM, Bollaert PE, Nabet P, Larcan A. Evolution of lactate/pyruvate and arterial ketone body ratios in the early course of catecholamine-treated septic shock. Crit Care Med. 2000; 28:114–119.16. Revelly JP, Tappy L, Martinez A, Bollmann M, Cayeux MC, Berger MM, Chioléro RL. Lactate and glucose metabolism in severe sepsis and cardiogenic shock. Crit Care Med. 2005; 33:2235–2240.17. Mikkelsen ME, Miltiades AN, Gaieski DF, Goyal M, Fuchs BD, Shah CV, Bellamy SL, Christie JD. Serum lactate is associated with mortality in severe sepsis independent of organ failure and shock. Crit Care Med. 2009; 37:1670–1677.18. Levraut J, Ciebiera JP, Chave S, Rabary O, Jambou P, Carles M, Grimaud D. Mild hyperlactatemia in stable septic patients is due to impaired lactate clearance rather than overproduction. Am J Respir Crit Care Med. 1998; 157:1021–1026.19. Laine L, Peterson WL. Bleeding peptic ulcer. N Engl J Med. 1994; 331:717–727.20. Chung IK, Ham JS, Kim HS, Park SH, Lee MH, Kim SJ. Comparison of the hemostatic efficacy of the endoscopic hemoclip method with hypertonic saline-epinephrine injection and a combination of the two for the management of bleeding peptic ulcers. Gastrointest Endosc. 1999; 49:13–18.21. Cho SH, Lee YS, Kim YJ, Sohn CH, Ahn S, Seo DW, Kim WY, Lee JH, Lim KS. Outcomes and role of urgent endoscopy in high-risk patients with acute nonvariceal gastrointestinal bleeding. Clin Gastroenterol Hepatol. Forthcoming. 2017.22. Saltzman JR, Tabak YP, Hyett BH, Sun X, Travis AC, Johannes RS. A simple risk score accurately predicts in-hospital mortality, length of stay, and cost in acute upper GI bleeding. Gastrointest Endosc. 2011; 74:1215–1224.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Lactate Parameters Predict Clinical Outcomes in Patients with Nonvariceal Upper Gastrointestinal Bleeding
- Endoscopic Management of Nonvariceal Upper Gastrointestinal Bleeding
- Endoscopy Timing in Patients with Acute Upper Gastrointestinal Bleeding
- Recent Update of Embolization of Upper Gastrointestinal Tract Bleeding
- Transcatheter Arterial Embolization of Nonvariceal Upper Gastrointestinal Bleeding with N-Butyl Cyanoacrylate