Imaging Sci Dent.
2017 Sep;47(3):149-155. 10.5624/isd.2017.47.3.149.
Three-dimensional analysis of impacted maxillary third molars: A cone-beam computed tomographic study of the position and depth of impaction
- Affiliations
-
- 1Master's Program in Dental Clinic, Faculty of Dentistry, Federal University of Juiz de Fora, Juiz de Fora, Minas Gerais, Brazil.
- 2Department of Restorative Dentistry, Faculty of Dentistry, Federal University of Juiz de Fora, Juiz de Fora, Minas Gerais, Brazil.
- 3Faculty of Medical and Health Sciences - SUPREMA, Juiz de Fora, Minas Gerais, Brazil.
- 4Department of Dental Clinic, Faculty of Dentistry, Federal University of Juiz de Fora, Juiz de Fora, Minas Gerais, Brazil. karina.devito@ufjf.edu.br
- KMID: 2390079
- DOI: http://doi.org/10.5624/isd.2017.47.3.149
Abstract
- PURPOSE
The classification of impacted maxillary third molars (IMTMs) facilitates interdisciplinary communication and helps estimate the degree of surgical difficulty. Thus, this study aimed to develop a 3-dimensional classification of the position and depth of impaction of IMTMs and to estimate their prevalence with respect to gender and age.
MATERIALS AND METHODS
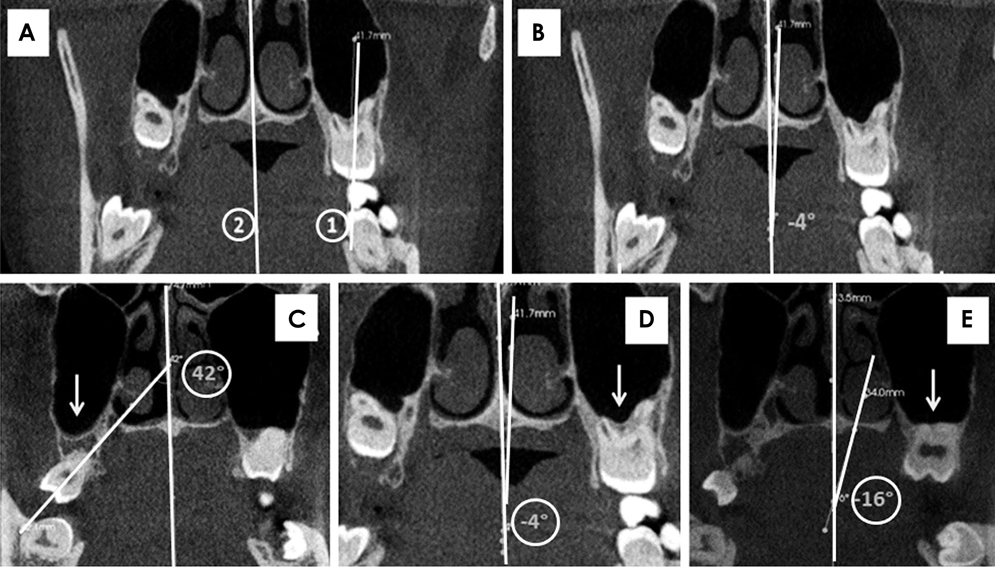
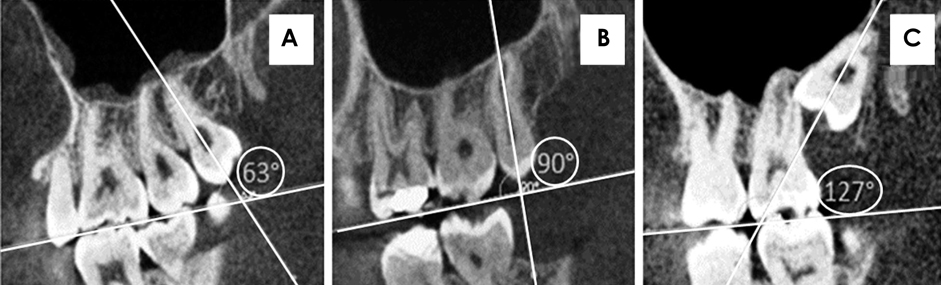
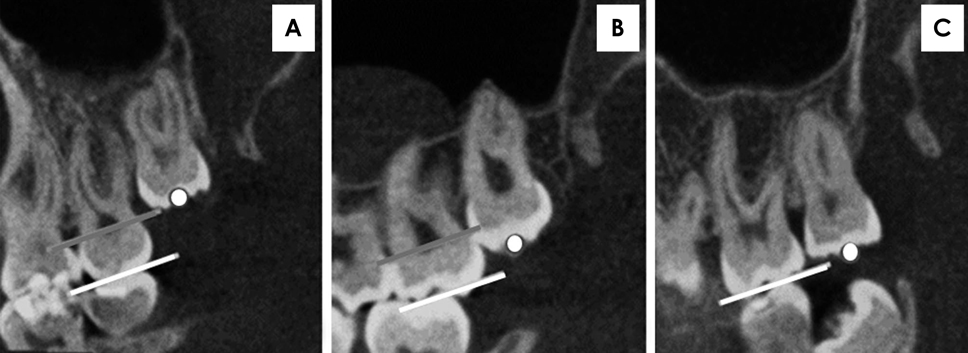
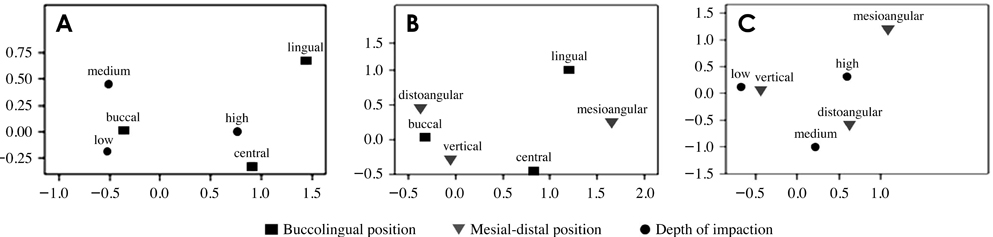
This cross-sectional retrospective study analyzed images in sagittal and coronal cone-beam computed tomography (CBCT) sections of 300 maxillary third molars. The proposed classification was based on 3 criteria: buccolingual position (buccal, lingual, or central), mesial-distal position (mesioangular, vertical, or distoangular), and depth of impaction (low, medium, or high). CBCT images of IMTMs were classified, and the associations of the classifications with gender and age were examined using analysis of variance with the Scheffé post-hoc test. To determine the associations among the 3 classifications, the chi-square test was used (P<.05).
RESULTS
No significant association of the classifications with gender was observed. Age showed a significant relationship with depth of impaction (P=.0001) and mesial-distal position (P=.005). The most common positions were buccal (n=222), vertical (n=184), and low (n=124). Significant associations among the 3 tested classifications were observed.
CONCLUSION
CBCT enabled the evaluation of IMTMs in a 3-dimensional format, and we developed a proposal for a new classification of the position and depth of impaction of IMTMs.
MeSH Terms
Figure
Cited by 1 articles
-
Radiographic evaluation before surgical extraction of impacted third molar to reduce the maxillary sinus related complication
Mi Hyun Seo, Buyanbileg Sodnom-Ish, Mi Young Eo, Hoon Myoung, Soung Min Kim
J Korean Assoc Oral Maxillofac Surg. 2023;49(4):192-197. doi: 10.5125/jkaoms.2023.49.4.192.
Reference
-
1. Topkara A, Sari Z. Investigation of third molar impaction in Turkish orthodontic patients: prevalence, depth and angular positions. Eur J Dent. 2013; 7:Suppl 1. S94–S98.
Article2. Nakamori K, Tomihara K, Noguchi M. Clinical significance of computed tomography assessment for third molar surgery. World J Radiol. 2014; 6:417–423.
Article3. de Carvalho RW, de Araújo Filho RC, do Egito Vasconcelos BC. Assessment of factors associated with surgical difficulty during removal of impacted maxillary third molars. J Oral Maxillofac Surg. 2013; 71:839–845.4. Carvalho RW, Araújo-Filho RC, Vasconcelos BC. Adverse events during the removal of impacted maxillary third molars. Int J Oral Maxillofac Surg. 2014; 43:1142–1147.
Article5. Winter GB. Principles of exodontia as applied to the impacted mandibular third molar; a complete treatise on the operative technic with clinical diagnoses and radiographic interpretations. St. Louis: American Medical Book Co.;1926.6. Pell GJ, Gregory BT. Impacted third molars: classification and modified technique for removal. Dent Dig. 1933; 39:330–338.7. Bouquet A, Coudert JL, Bourgeois D, Mazoyer JF, Bossard D. Contributions of reformatted computed tomography and panoramic radiography in the localization of third molars relative to the maxillary sinus. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004; 98:342–347.
Article8. Jung YH, Cho BH. Prevalence of missing and impacted third molars in adults aged 25 years and above. Imaging Sci Dent. 2013; 43:219–225.
Article9. Celikoglu M, Miloglu O, Kazanci F. Frequency of agenesis, impaction, angulation, and related pathologic changes of third molar teeth in orthodontic patients. J Oral Maxillofac Surg. 2010; 68:990–995.
Article10. Hassan AH. Pattern of third molar impaction in a Saudi population. Clin Cosmet Investig Dent. 2010; 2:109–113.
Article11. Hashemipour MA, Tahmasbi-Arashlow M, Fahimi-Hanzaei F. Incidence of impacted mandibular and maxillary third molars: a radiographic study in a Southeast Iran population. Med Oral Patol Oral Cir Bucal. 2013; 18:e140–e145.12. Lim AA, Wong CW, Allen JC Jr. Maxillary third molar: patterns of impaction and their relation to oroantral perforation. J Oral Maxillofac Surg. 2012; 70:1035–1039.
Article13. Sandhu S, Kaur T. Radiographic study of the positional changes and eruption of impacted third molars in young adults of an Asian Indian population. J Oral Maxillofac Surg. 2008; 66:1617–1624.
Article14. Oenning AC, Neves FS, Alencar PN, Prado RF, Groppo FC, Haiter-Neto F. External root resorption of the second molar associated with third molar impaction: comparison of panoramic radiography and cone beam computed tomography. J Oral Maxillofac Surg. 2014; 72:1444–1455.
Article15. Ventä I, Turtola L, Ylipaavalniemi P. Radiographic follow-up of impacted third molars from age 20 to 32 years. Int J Oral Maxillofac Surg. 2001; 30:54–57.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evaluation of Impacted Maxillary Canine Position Using Panoramic Radiographs and Cone-beam Computed Tomography
- Comparison of panoramic radiography and cone beam computed tomography for assessing the relationship between the maxillary sinus floor and maxillary molars
- Cone beam computed tomography findings of ectopic mandibular third molar in the mandibular condyle: report of a case
- Assessment of maxillary third molars with panoramic radiography and cone-beam computed tomography
- Assessment of the relationship between the mandibular third molar and the mandibular canal using panoramic radiograph and cone beam computed tomography