Ann Hepatobiliary Pancreat Surg.
2017 Aug;21(3):172-175. 10.14701/ahbps.2017.21.3.172.
Distal pancreatectomy for pancreatic arteriovenous malformation: report of a case
- Affiliations
-
- 1Department of Surgery, Kosin University Gospel Hospital, Kosin University College of Medicine, Busan, Korea. tsojc@naver.com
- KMID: 2389996
- DOI: http://doi.org/10.14701/ahbps.2017.21.3.172
Abstract
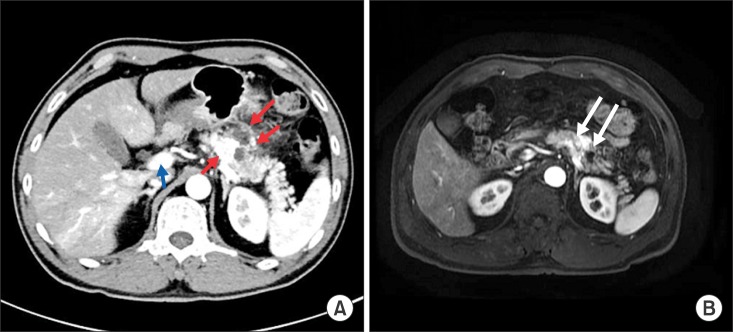
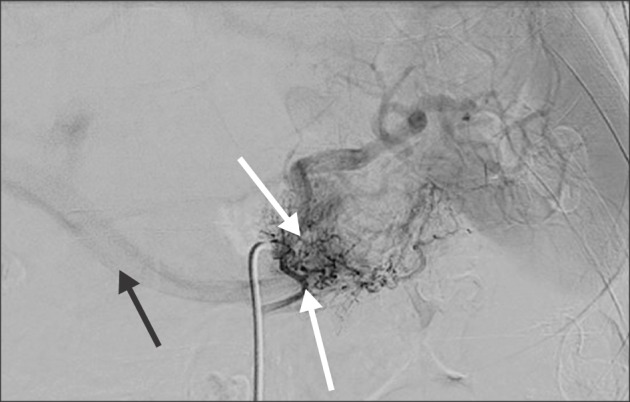
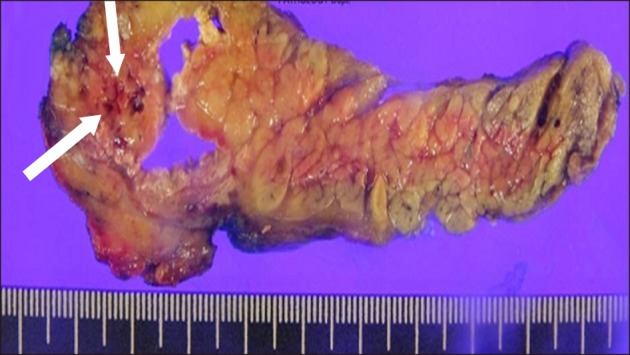
- Arteriovenous malformation (AVM) of the pancreas is an uncommon disease, which can cause an abdominal pain. This disease is characterized by a tangled vascular network, including the whole or part of the pancreas, resulting in portal hypertension by forming a shunt of the pancreas arteries to drain directly into the portal venous system. This study presents a case that was suspected as AVM of the pancreas by preoperative contrast-enhanced computed tomography scan (CT). A 49-year-old male patient had several episodes of abdominal discomfort associated with dyspepsia for 4 days. Magnetic resonance imaging showed enhancement of the conglomeration about 1.5 cm size in diameter in the pancreas. Selective angiography showed the proliferation of a vascular network in the pancreas and an early visualization of the portal vein during the arterial phase. Distal pancreatectomy with splenectomy was done. Histology of the pancreas showed AVM, with enzymatic fat necrosis extending to the capsule of the pancreas. The patient recovered successfully without postoperative complications. Surgical resection of pancreas is the definitive treatment for symptomatic AVM.
MeSH Terms
Figure
Reference
-
1. Halpern M, Turner AF, Citron BP. Hereditary hemorrhagic telangiectasia. An angiographic study of abdominal visceral angiodysplasias associated with gastrointestinal hemorrhage. Radiology. 1968; 90:1143–1149. PMID: 5656734.2. Lande A, Bedford A, Schechter LS. The spectrum of arteriographic findings in Osler-Weber-Rendu disease. Angiology. 1976; 27:223–240. PMID: 1053528.
Article3. Nishiyama R, Kawanishi Y, Mitsuhashi H, Kanai T, Ohba K, Mori T, et al. Management of pancreatic arteriovenous malformation. J Hepatobiliary Pancreat Surg. 2000; 7:438–442. PMID: 11180867.
Article4. Song KB, Kim SC, Park JB, Kim YH, Jung YS, Kim MH, et al. Surgical outcomes of pancreatic arteriovenous malformation in a single center and review of literature. Pancreas. 2012; 41:388–396. PMID: 22129532.
Article5. Makhoul F, Kaur P, Johnston TD, Jeon H, Gedaly R, Ranjan D. Arteriovenous malformation of the pancreas: A case report and review of literature. Int J Angiol. 2008; 17:211–213. PMID: 22477452.
Article6. Aida K, Nakamura H, Kihara Y, Abe S, Okamoto K, Otsuki M. Duodenal ulcer and pancreatitis associated with pancreatic arteriovenous malformation. Eur J Gastroenterol Hepatol. 2002; 14:551–554. PMID: 11984154.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pancreatic Arteriovenous Malformation Combined with Pseudocysts
- A Case of Recurrent Acute Pancreatitis due to Pancreatic Arteriovenous Malformation
- A Case of Arteriovenous Malformation of the Pancreas
- Arteriovenous Malformation with a Retention Cyst of the Pancreas
- Utilization of end to side inverted mattress pancreaticojejunostomy for Duval procedure: A case report