Korean Circ J.
2016 Sep;46(5):672-680. 10.4070/kcj.2016.46.5.672.
Prevalence of Comorbidity among People with Hypertension: The Korea National Health and Nutrition Examination Survey 2007-2013
- Affiliations
-
- 1Department of Preventive Medicine, Yonsei University College of Medicine, Seoul, Korea. HCKIM@yuhs.ac
- 2Cardiovascular and Metabolic Diseases Etiology Research Center, Yonsei University College of Medicine, Seoul, Korea.
- 3Department of Public Health, Yonsei University College of Medicine, Seoul, Korea.
- 4Department of Preventive Medicine, Graduate School of Public Health, Seoul, Korea.
- KMID: 2389625
- DOI: http://doi.org/10.4070/kcj.2016.46.5.672
Abstract
- BACKGROUND AND OBJECTIVES
Joint National Committee guidelines attempt to vary treatment recommendations for patients based on considerations of their comorbidities. The aim of the present study is to estimate the age-standardized prevalence of common comorbidities among Korean hypertension patients.
SUBJECTS AND METHODS
We analyzed the Korea National Health and Nutrition Examination Survey from 2007 to 2013. Among the 58423 participants, 30092 adults, aged ≥30 yrs who completed a health examination and interview survey, were selected. The survey procedures were used to estimate weighted prevalence and odds ratios for 8 comorbidities, including obesity, diabetes mellitus, dyslipidemia, cardiovascular disease, chronic kidney disease, and thyroid disease.
RESULTS
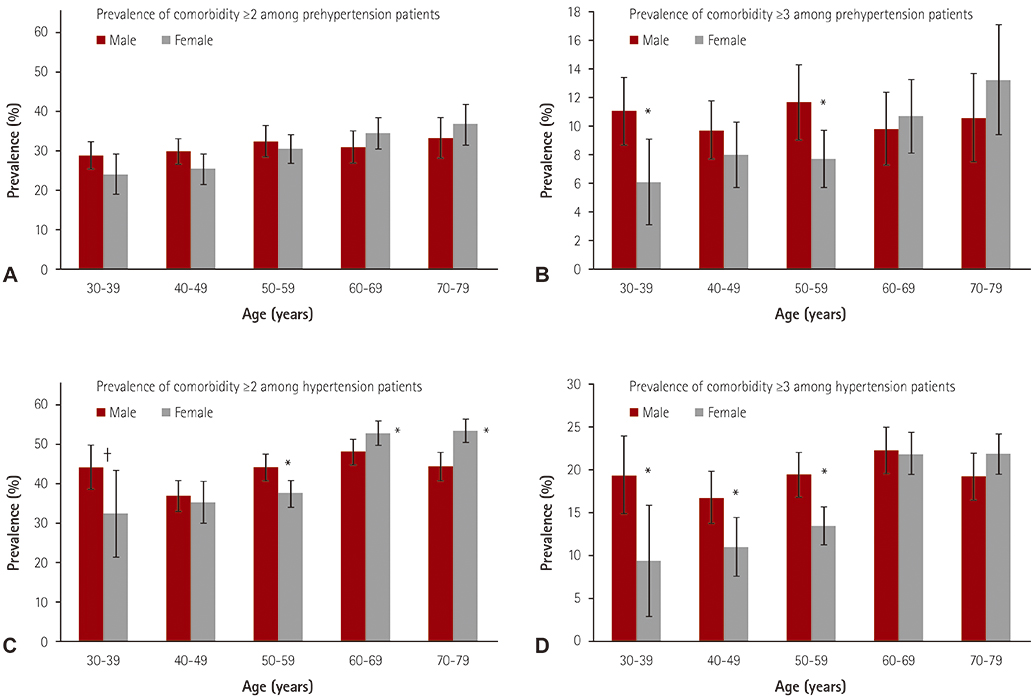
Most chronic conditions were more prevalent in adults with hypertension than in those without hypertension. Common comorbidities were obesity (60.1%), dyslipidemia (57.6%), and impaired fasting glucose (45.1%). Hypertensive patients with two or more comorbid diseases were 42.2% and those with three or more diseases were 17.7%. The age- and sex-specific prevalence of three or more comorbid diseases among male hypertension patients was significantly higher than those patients in the 30-59 (p<0.05) age group.
CONCLUSION
Comorbidity is highly prevalent in Korean patients with hypertension.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Lifestyle Modification, the Effective but Neglected Strategy in Lowering Blood Pressure
Wook Bum Pyun
Korean Circ J. 2018;48(7):652-654. doi: 10.4070/kcj.2018.0194.
Reference
-
1. Guiding principles for the care of older adults with multimorbidity: an approach for clinicians. Guiding principles for the care of older adults with multimorbidity: an approach for clinicians: American Geriatrics Society Expert Panel on the Care of Older Adults with Multimorbidity. J Am Geriatr Soc. 2012; 60:E1–E25.2. Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012; 380:37–43.3. Fortin M, Stewart M, Poitras M-E, Almirall J, Maddocks H. A systematic review of prevalence studies on multimorbidity: toward a more uniform methodology. Ann Fam Med. 2012; 10:142–151.4. Marengoni A, Angleman S, Melis R, et al. Aging with multimorbidity: a systematic review of the literature. Ageing Res Rev. 2011; 10:430–439.5. Sung YN, Jang SM, Lim DH, Shin SY, Song HJ, Lee SH. Prescribing patterns of antihypertensive drugs by outpatients with hypertension in 2007. Korean J Clin Pharm. 2009; 19:167–179.6. Violán C, Foguet-Boreu Q, Hermosilla-Pérez E, et al. Comparison of the information provided by electronic health records data and a population health survey to estimate prevalence of selected health conditions and multimorbidity. BMC Public Health. 2013; 13:251.7. Kim HJ, Kim Y, Cho Y, Jun B, Oh KW. Trends in the prevalence of major cardiovascular disease risk factors among Korean adults: results from the Korea National Health and Nutrition Examination Survey, 1998-2012. Int J Cardiol. 2014; 174:64–72.8. Lewis SA, Weiss ST, Platts-Mills TA, Burge H, Gold DR. The role of indoor allergen sensitization and exposure in causing morbidity in women with asthma. Am J Respir Crit Care Med. 2002; 165:961–966.9. Bassett J. International Diabetes Institute. World Health Organization Regional Office for the Western Pacific. International Association for the Study of Obesity. International Obesity Task Force. The Asia-Pacific perspective: redefining obesity and its treatment. Melbourne: Health Communications Australia;2000.10. Benoist Bd, McLean E, Cogswell IEaM. Worldwide prevalence of anaemia 1993-2005 of WHO: Global Database of anaemia. Geneva: World Health Organization;2008.11. Altman DG, Bland JM. Interaction revisited: the difference between two estimates. BMJ. 2003; 326:219.12. Tocci G, Muiesan ML, Parati G, et al. Trends in prevalence, awareness, treatment, and control of blood pressure recorded from 2004 to 2014 during world hypertension day in Italy. J Clin Hypertens (Greenwich). 2016; 18:551–556.13. Giampaoli S, Palmieri L, Donfrancesco C, Lo Noce C, Pilotto L, Vanuzzo D. Cardiovascular health in Italy. Ten-year surveillance of cardiovascular diseases and risk factors: Osservatorio Epidemiologico Cardiovascolare/Health Examination Survey 1998-2012. Eur J Prev Cardiol. 2015; 22:2 Suppl. 9–37.14. Steinman MA, Lee SJ, Boscardin WJ, et al. Patterns of multimorbidity in elderly veterans. J Am Geriatr Soc. 2012; 60:1872–1880.15. Fryar CD, Hirsch R, Eberhardt MS, Yoon SS, Wright JD. Hypertension, high serum total cholesterol, and diabetes: racial and ethnic prevalence differences in US adults, 1999-2006. NCHS Data Brief. 2010; (36):1–8.16. Davila EP, Hlaing WM. Co-Morbidities of Emergency Department Patients Admitted with Essential Hypertension in Florida. Ann Epidemiol. 17:726–727.17. Strandberg AY, Strandberg TE, Stenholm S, Salomaa VV, Pitkälä KH, Tilvis RS. Low midlife blood pressure, survival, comorbidity, and health-related quality of life in old age: the Helsinki Businessmen Study. J Hypertens. 2014; 32:1797–1804.18. Abad-Díez JM, Calderón-Larrañaga A, Poncel-Falcó A, et al. Age and gender differences in the prevalence and patterns of multimorbidity in the older population. BMC Geriatr. 2014; 14:75.19. Perelman J, Mateus C, Fernandes A. Gender equity in treatment for cardiac heart disease in Portugal. Soc Sci Med. 2010; 71:25–29.20. Bowling A, Bond M, McKee D, et al. Equity in access to exercise tolerance testing, coronary angiography, and coronary artery bypass grafting by age, sex and clinical indications. Heart. 2001; 85:680–686.21. García-Olmos L, Salvador CH, Alberquilla Á, et al. Comorbidity patterns in patients with chronic diseases in general practice. PLoS One. 2012; 7:e32141.22. Violán C, Foguet-Boreu Q, Roso-Llorach A, et al. Burden of multimorbidity, socioeconomic status and use of health services across stages of life in urban areas: a cross-sectional study. BMC Public Health. 2014; 14:530.23. Jung YH, Ko SJ, Kim EJ. A study on the effective chronic disease management: Policy directions for chronic diseases management. Seoul: Korea Institute for Health and Social Affairs Press;2013.24. Ministry of Health and Welfare. Korea Centers for Disease Control and Prevention. Korea health statistics 2013: Korea National Health and Nutrition Examination Survey (KNHANES VI-1). Cheongju: Korea Centers for Disease Control and Prevention;2014.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Trend Analysis of the Prevalence, Awareness, Treatment, and Control of Hypertension by Age Group
- Sex-Specific Trends in the Prevalence of Hypertension and the Number of People With Hypertension: Analysis of the Korea National Health and Nutrition Examination Survey (KNHANES) 1998–2018
- Prevalence of Hypertension and Related Risk Factors in the Elderly: Data from the 4th Korean National Health & Nutrition Examination Survey, 2007~2009
- The Current Status and the Perspectives of Nutrition Survey
- Association between Education Level and Hypertension in Korean Adults Over 30 Years Old: Korea National Health and Nutrition Examination Survey 2019