Korean Circ J.
2017 Sep;47(5):543-554. 10.4070/kcj.2017.0030.
Current Drug Therapy in Chronic Heart Failure: the New Guidelines of the European Society of Cardiology (ESC)
- Affiliations
-
- 1Department of Cardiology and Angiology, Hannover Medical School, Hannover, Germany. berliner.dominik@mh-hannover.de, bauersachs.johann@mh-hannover.de
- KMID: 2389594
- DOI: http://doi.org/10.4070/kcj.2017.0030
Abstract
- Congestive heart failure (HF) is a morbidity that is increasing worldwide due to the aging population and improvement in (acute) care for patients with cardiovascular diseases. The prognosis for patients with HF is very poor without treatment. Furthermore, (repeated) hospitalizations for cardiac decompensation cause an increasing economic burden. Modern drugs and the consequent implementation of therapeutic recommendations have substantially improved the morbidity and mortality of HF patients. This paper provides an overview of the current pharmacological management of HF patients, based on the 2016 guidelines of the European Society of Cardiology (ESC).
MeSH Terms
Figure
Reference
-
1. Heart Failure Society of America. HFSA 2010 comprehensive heart failure practice guideline. J Card Fail. 2010; 16:e1–e194.2. Askoxylakis V, Thieke C, Pleger ST, et al. Long-term survival of cancer patients compared to heart failure and stroke: a systematic review. BMC Cancer. 2010; 10:105.3. Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2016; 18:891–975.4. Yancy CW, Jessup M, Bozkurt B, et al. 2016 ACC/AHA/HFSA focused update on new pharmacological therapy for heart failure: an update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. J Am Coll Cardiol. 2016; 68:1476–1488.5. Solomon SD, Claggett B, Lewis EF, et al. Influence of ejection fraction on outcomes and efficacy of spironolactone in patients with heart failure with preserved ejection fraction. Eur Heart J. 2016; 37:455–462.6. CONSENSUS Trial Study Group. Effects of enalapril on mortality in severe congestive heart failure. Results of the Cooperative North Scandinavian Enalapril Survival Study (CONSENSUS). N Engl J Med. 1987; 316:1429–1435.7. SOLVD Investigators. Yusuf S, Pitt B, Davis CE, Hood WB, Cohn JN. Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. N Engl J Med. 1991; 325:293–302.8. Packer M, Poole-Wilson PA, Armstrong PW, et al. Comparative effects of low and high doses of the angiotensin-converting enzyme inhibitor, lisinopril, on morbidity and mortality in chronic heart failure. ATLAS Study Group. Circulation. 1999; 100:2312–2318.9. Maggioni AP, Anker SD, Dahlström U, et al. Are hospitalized or ambulatory patients with heart failure treated in accordance with European Society of Cardiology guidelines? Evidence from 12,440 patients of the ESC Heart Failure Long-Term Registry. Eur J Heart Fail. 2013; 15:1173–1184.10. Heart Failure: 150 Questions & Answers. 2nd ed. Neuilly-sur-Seinex: Servier;2011.11. CIBIS-II Investigators and Committees. The Cardiac Insufficiency Bisoprolol Study II (CIBIS-II): a randomised trial. Lancet. 1999; 353:9–13.12. Packer M, Fowler MB, Roecker EB, et al. Effect of carvedilol on the morbidity of patients with severe chronic heart failure: results of the carvedilol prospective randomized cumulative survival (COPERNICUS) study. Circulation. 2002; 106:2194–2199.13. Hjalmarson A, Goldstein S, Fagerberg B, et al. Effects of controlled-release metoprolol on total mortality, hospitalizations, and well-being in patients with heart failure: the Metoprolol CR/XL Randomized Intervention Trial in congestive heart failure (MERIT-HF). MERIT-HF Study Group. JAMA. 2000; 283:1295–1302.14. Flather MD, Shibata MC, Coats AJ, et al. Randomized trial to determine the effect of nebivolol on mortality and cardiovascular hospital admission in elderly patients with heart failure (SENIORS). Eur Heart J. 2005; 26:215–225.15. Pitt B, Zannad F, Remme WJ, et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized Aldactone Evaluation Study Investigators. N Engl J Med. 1999; 341:709–717.16. Pitt B, Remme W, Zannad F, et al. Eplerenone, a selective aldosterone blocker, in patients with left ventricular dysfunction after myocardial infarction. N Engl J Med. 2003; 348:1309–1321.17. Zannad F, McMurray JJ, Krum H, et al. Eplerenone in patients with systolic heart failure and mild symptoms. N Engl J Med. 2011; 364:11–21.18. Eschalier R, McMurray JJ, Swedberg K, et al. Safety and efficacy of eplerenone in patients at high risk for hyperkalemia and/or worsening renal function: analyses of the EMPHASIS-HF study subgroups (Eplerenone in Mild Patients Hospitalization and SurvIval Study in Heart Failure). J Am Coll Cardiol. 2013; 62:1585–1593.19. Bauersachs J. The ARTS of third-generation mineralocorticoid receptor antagonists: achieving cardiovascular benefit with minimized renal side effects? Eur Heart J. 2013; 34:2426–2428.20. Swedberg K, Komajda M, Böhm M, et al. Ivabradine and outcomes in chronic heart failure (SHIFT): a randomised placebo-controlled study. Lancet. 2010; 376:875–885.21. Böhm M, Borer J, Ford I, et al. Heart rate at baseline influences the effect of ivabradine on cardiovascular outcomes in chronic heart failure: analysis from the SHIFT study. Clin Res Cardiol. 2013; 102:11–22.22. Berliner D, Bauersachs J. Eine vielversprechende neue Behandlungsoption - verändert LCZ696 die Therapie der Herzinsuffizienz? Kompendium Herz-Kreislauf. 2015; 11:23–27.23. McMurray JJ, Packer M, Desai AS, et al. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med. 2014; 371:993–1004.24. Dec GW. LCZ696 (sacubitril/valsartan): can we predict who will benefit? J Am Coll Cardiol. 2015; 66:2072–2074.25. Kristensen SL, Preiss D, Jhund PS, et al. Risk related to pre-diabetes mellitus and diabetes mellitus in heart failure with reduced ejection fraction: insights from prospective comparison of ARNI with ACEI to determine impact on global mortality and morbidity in heart failure trial. Circ Heart Fail. 2016; 9:e002560.26. Digitalis Investigation Group. The effect of digoxin on mortality and morbidity in patients with heart failure. N Engl J Med. 1997; 336:525–533.27. Adams KF Jr, Butler J, Patterson JH, et al. Dose response characterization of the association of serum digoxin concentration with mortality outcomes in the Digitalis Investigation Group trial. Eur J Heart Fail. 2016; 18:1072–1081.28. Gheorghiade M, Patel K, Filippatos G, et al. Effect of oral digoxin in high-risk heart failure patients: a pre-specified subgroup analysis of the DIG trial. Eur J Heart Fail. 2013; 15:551–559.29. Bavendiek U, Aguirre Davila L, Koch A, Bauersachs J. Assumption versus evidence: the case of digoxin in atrial fibrillation and heart failure. [Epub ahead of print]. Eur Heart J. 2017.30. Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015; 373:2117–2128.31. Fitchett D, Zinman B, Wanner C, et al. Heart failure outcomes with empagliflozin in patients with type 2 diabetes at high cardiovascular risk: results of the EMPA-REG OUTCOME® trial. Eur Heart J. 2016; 37:1526–1534.32. Jankowska EA, Rozentryt P, Witkowska A, et al. Iron deficiency: an ominous sign in patients with systolic chronic heart failure. Eur Heart J. 2010; 31:1872–1880.33. Anker SD, Comin Colet J, Filippatos G, et al. Ferric carboxymaltose in patients with heart failure and iron deficiency. N Engl J Med. 2009; 361:2436–2448.34. Jankowska EA, Tkaczyszyn M, Suchocki T, et al. Effects of intravenous iron therapy in iron-deficient patients with systolic heart failure: a meta-analysis of randomized controlled trials. Eur J Heart Fail. 2016; 18:786–795.35. Burnier M, Brunner HR. Angiotensin II receptor antagonists. Lancet. 2000; 355:637–645.36. Burnier M. Angiotensin II type 1 receptor blockers. Circulation. 2001; 103:904–912.37. Schmieder RE, Hilgers KF, Schlaich MP, Schmidt BM. Renin-angiotensin system and cardiovascular risk. Lancet. 2007; 369:1208–1219.38. Bristow MR. Mechanism of action of beta-blocking agents in heart failure. Am J Cardiol. 1997; 80:26L–40L.39. Metra M, Nodari S, D'Aloia A, Bontempi L, Boldi E, Cas LD. A rationale for the use of β-blockers as standard treatment for heart failure. Am Heart J. 2000; 139:511–521.40. Bristow MR. Why does the myocardium fail? Insights from basic science. Lancet. 1998; 352:Suppl 1. SI8–SI14.41. Young MJ, Lam EY, Rickard AJ. Mineralocorticoid receptor activation and cardiac fibrosis. Clin Sci (Lond). 2007; 112:467–475.42. Bauersachs J, Jaisser F, Toto R. Mineralocorticoid receptor activation and mineralocorticoid receptor antagonist treatment in cardiac and renal diseases. Hypertension. 2015; 65:257–263.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
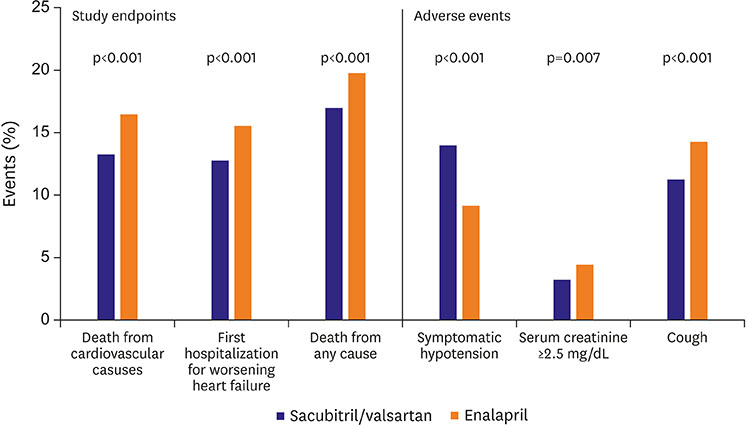
- Similar articles
-
- A Comparative Study of USA and Europe Guidelines of Rate and Rhythm Control Pharmacotherapy in Atrial Fibrillation
- Updated Guidelines for Acute Coronary Syndrome
- New European Society of Cardiology/European Atherosclerosis Society Guideline for the Management of Dyslipidemia
- A Comparative Study the USA, Europe and Korea Guidelines of Antiplatelet Therapy for Patients with Acute Coronary Syndrome
- Acute Heart Failure and Its Management