Neurointervention.
2017 Sep;12(2):59-68. 10.5469/neuroint.2017.12.2.59.
A Meta-Analysis of Observational Evidence for the Use of Endovascular Thrombectomy in Proximal Occlusive Stroke Beyond 6 Hours in Patients with Limited Core Infarct
- Affiliations
-
- 1Department of Neuroradiology, North Bristol NHS Trust, Southmead Hospital, Bristol, BS10 5NB, United Kingdom. alex_mortimer@hotmail.com
- 2NeuroSpine Surgery Research Group (NSURG), Level 7, Prince of Wales Private Hospital, Barker Street, Sydney, NSW, 2109, Australia.
- KMID: 2389497
- DOI: http://doi.org/10.5469/neuroint.2017.12.2.59
Abstract
- PURPOSE
The safety and efficacy of endovascular thrombectomy (EVT) for patients with proximal occlusive stroke presenting beyond 6 hours and selected on the basis of favorable neuroimaging remains unclear.
MATERIALS AND METHODS
A systematic search was performed from four electronic databases from their inception to Jan 2017. A meta-analysis of outcomes from studies with patients treated beyond 6 hours was compared to those treated within the established 6 hour therapeutic window in randomized trials, selected using conventional imaging methods with CT/CT angiography.
RESULTS
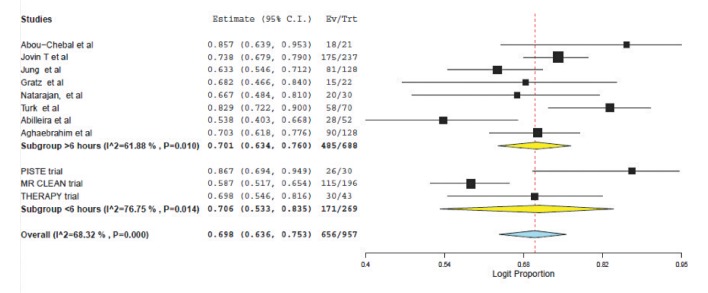
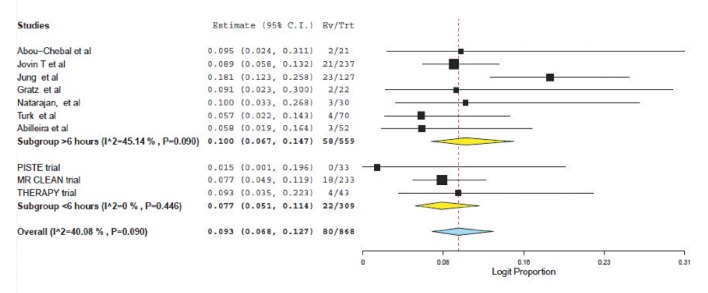
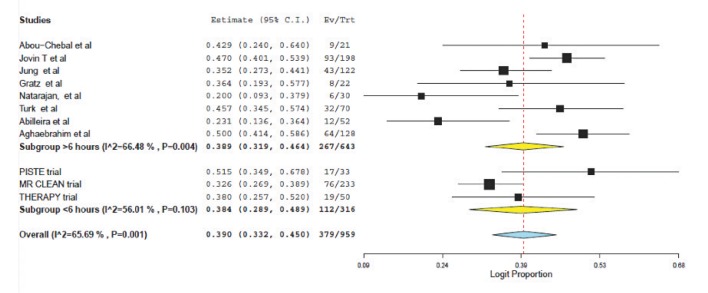
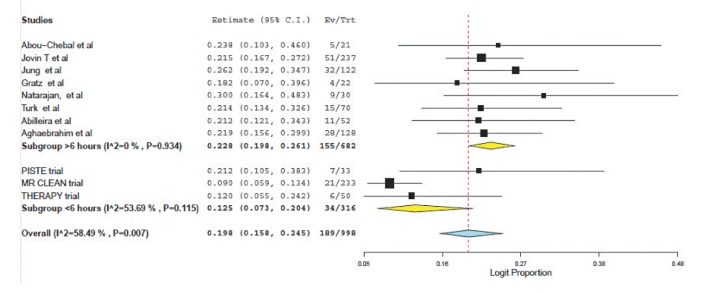
A total of 8 articles met inclusion criteria for the study population (a prospective single-center study, 5 retrospective single-center studies and 2 retrospective multicenter studies). These were compared to the results of three prospective trials of patients treated within 6 hours selected using CT/CT angiography. For patients treated >6 hours and <6 hours respectively, the weighted mean age was 64.7 vs. 67.0 years; the presenting NIHSS was 15.7 vs. 17.1 and the time from symptom onset to puncture was 4.0 hours vs. 15.1 hours. Weighted pooled estimates of successful recanalization (TIMI 2/3 or TICI 2b/3) and favorable outcome (mRS ≤2) were similar between both groups, 70.1% vs. 70.6%, P=0.75 and 38.9% vs. 38.4%, P=0.88 respectively. Pooled mortality measured at 3 months was 22.8% for those treated >6 hours and 12.5% for <6 hours, P<0.0001. Symptomatic intracranial hemorrhage was not significantly different (10.0% vs. 7.7%, P=0.33).
CONCLUSION
When compared to established methods of patient selection, EVT employed beyond 6 hours in those selected with imaging to exclude large core infarcts achieves similar rates of recanalization, and functional outcome but there is a significant increase in mortality despite no increase in symptomatic intracranial hemorrhage.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Mechanical Thrombectomy in Strokes with Large-Vessel Occlusion Beyond 6 Hours: A Pooled Analysis of Randomized Trials
Simone Vidale, Marco Longoni, Luca Valvassori, Elio Agostoni
J Clin Neurol. 2018;14(3):407-412. doi: 10.3988/jcn.2018.14.3.407.
Reference
-
1. Saver JL, Goyal M, van der Lugt A, Menon BK, Majoie CB, Dippel DW, et al. Time to Treatment With Endovascular Thrombectomy and Outcomes From Ischemic Stroke: A Meta-analysis. JAMA. 2016; 316:1279–1288. PMID: 27673305.
Article2. Muir KW, Ford GA, Messow CM, Ford I, Murray A, Clifton A, et al. Endovascular therapy for acute ischaemic stroke: the Pragmatic Ischaemic Stroke Thrombectomy Evaluation (PISTE) randomised, controlled trial. J Neurol Neurosurg Psychiatry. 2017; 88:38–44. PMID: 27756804.
Article3. Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. A Randomized trial of Intraarterial treatment for acute Ischemic stroke. N Engl J Med. 2015; 372:11–20. PMID: 25517348.4. Mocco J, Zaidat OO, von Kummer R, Yoo AJ, Gupta R, Lopes D, et al. Aspiration Thrombectomy After Intravenous Alteplase Versus Intravenous Alteplase Alone. Stroke. 2016; 47:2331–2338. PMID: 27486173.
Article5. White PM, Bhalla A, Dinsmore J, James M, McConachie N, Roffe C, et al. Standards for providing safe acute ischaemic stroke thrombectomy services. Clin Radiol. 2017; 72:175175.e1–175.e9.6. ESO Karolinska Consensus Stroke Update Consensus statement. 2015. http://2014strokeupdate.org/consensus-statement-mechanical-thrombectomy-acuteischemic-stroke.7. Powers WJ, Derdeyn CP, Biller J, Coffey CS, Hoh BL, Jauch EC, et al. 2015 American Heart Association/American Stroke Association Focused Update of the 2013 Guidelines for the Early Management of Patients With Acute Ischemic Stroke Regarding Endovascular Treatment: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2015; 46:3020–3035. PMID: 26123479.
Article8. Addo J, Ayis S, Leon J, Rudd AG, McKevitt C, Wolfe CD. Delay in presentation after an acute stroke in a Multiethnic population in south London: The south London stroke register. J Am Heart Assoc. 2012; 1:e001685. PMID: 23130144.
Article9. HQIP. SSNAP acute organisational audit report. 2016. http://www.hqip.org.uk/resources/ssnap-acute-organisational-auditreport.10. Hakimelahi R, Vachha B, Copen W, Papini GD, He J, Higazi MM, et al. Time and diffusion lesion size in major anterior circulation ischemic strokes. Stroke. 2014; 45:2936–2941. PMID: 25190444.
Article11. Campbell BC, Christensen S, Tress BM, Churilov L, Desmond PM, Parsons MW, et al. Failure of collateral blood flow is associated with infarct growth in ischemic stroke. J Cereb Blood Flow Metab. 2013; 33:1168–1172. PMID: 23652626.
Article12. Bang OY, Goyal M, Liebeskind DS. Collateral circulation in ischemic stroke: Assessment tools and therapeutic strategies. Stroke. 2015; 46:3302–3309. PMID: 26451027.13. Miteff F, Levi C, Bateman G, Spratt N, McElduff P, Parsons MW. The independent predictive utility of computed tomography angiographic collateral status in acute ischaemic stroke. Brain. 2009; 132:2231–2238. PMID: 19509116.
Article14. Lansberg MG, Straka M, Kemp S, Mlynash M, Wechsler LR, Jovin TG, et al. MRI profile and response to endovascular reperfusion after stroke (DEFUSE 2): a prospective cohort study. Lancet Neurol. 2012; 11:860–867. PMID: 22954705.
Article15. Wouters A, Lemmens R, Christensen S, Wilms G, Dupont P, Mlynash M, et al. Magnetic resonance imaging-based endovascular versus medical stroke treatment for symptom onset up to 12 h. Int J Stroke. 2016; 11:127–133. PMID: 26763028.16. Jovin T. Diffusion-weighted imaging or computerized tomography perfusion assessment with clinical mismatch in the triage of wake up and late presenting strokes undergoing neurointervention with Trevo (DAWN). In : 3rd European Stroke Organisation Conference (ESOC); 2017 May 16 - 18; Prague: Czech Republic: 2017.17. Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, et al. Stent-Retriever Thrombectomy after intravenous t-pA vs. tpA alone in stroke. N Engl J Med. 2015; 372:2285–2229. PMID: 25882376.
Article18. Bracard S, Ducrocq X, Mas JL, Soudant M, Oppenheim C, Moulin T, et al. Mechanical thrombectomy after intravenous alteplase versus alteplase alone after stroke (THRACE): a randomised controlled trial. Lancet Neurol. 2016; 15:1138–1147. PMID: 27567239.
Article19. Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, et al. Thrombectomy within 8 hours after symptom onset in Ischemic stroke. N Engl J Med. 2015; 372:2296–2306. PMID: 25882510.
Article20. Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015; 372:1019–1030. PMID: 25671798.21. Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015; 372:1009–1018. PMID: 25671797.
Article22. Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005; 5:13. PMID: 15840177.
Article23. Cochrane Handbook. http://handbook.cochrane.org/chapter_7/7_7_3_5_mediansand_interquartile_ranges.htm.24. Abou-Chebl A. Endovascular treatment of acute ischemic stroke may be safely performed with no time window limit in appropriately selected patients. Stroke. 2010; 41:1996–2000. PMID: 20651271.
Article25. Jovin TG, Liebeskind D, Gupta R, Rymer M, Rai A, Zaidat OO, et al. Imaging-based endovascular therapy for acute ischemic stroke due to proximal intracranial anterior circulation occlusion treated beyond 8 hours from time last seen well: retrospective multicenter analysis of 237 consecutive patients. Stroke. 2011; 42:2206–2211. PMID: 21778444.26. Jung S, Gralla J, Fischer U, Mono ML, Weck A, L¨udi R, et al. Safety of endovascular treatment beyond the 6-h time window in 205 patients. Eur J Neurol. 2013; 20:865–871. PMID: 23293861.
Article27. Gratz PP, Jung S, Schroth G, Gralla J, Mordasini P, Hsieh K, et al. Outcome of standard and high-risk patients with acute anterior circulation stroke after stent retriever thrombectomy. Stroke. 2014; 45:152–158. PMID: 24262328.
Article28. Natarajan SK, Snyder KV, Siddiqui AH, Ionita CC, Hopkins LN, Levy EI. Safety and effectiveness of Endovascular therapy after 8 hours of acute Ischemic stroke onset and wake-up strokes. Stroke. 2009; 40:3269–3274. PMID: 19628808.
Article29. Turk AS, Nyberg E, Chaudry M, Turner RD, Magarik JA, Nicholas JS, et al. Utilization of CT perfusion patient selection for mechanical thrombectomy irrespective of time: a comparison of functional outcomes and complications. J Neurointerv Surg. 2013; 5:518–522. PMID: 22935349.
Article30. Abilleira S, Cardona P, Ribó M, Millán M, Obach V, Roquer J, et al. Outcomes of a contemporary cohort of 536 consecutive patients with acute ischemic stroke treated with endovascular therapy. Stroke. 2014; 45:1046–1052. PMID: 24595590.
Article31. Aghaebrahim A, Leiva-Salinas C, Jadhav A, Jankowitz B, Zaidi S, Jumaa M, et al. Outcomes after endovascular treatment for anterior circulation stroke presenting as wake-up strokes are not different than those with witnessed onset beyond 8 hours. J Neurointerv Surg. 2015; 7:875–880. PMID: 25326003.32. Telischak NA, Wintermark M. Imaging predictors of procedural and clinical outcome in endovascular acute stroke therapy. Neurovasc Imaging. 2015; 1:4.
Article33. Sheth SA, Sanossian N, Hao Q, Starkman S, Ali LK, Kim D, et al. Collateral flow as causative of good outcomes in endovascular stroke therapy. J Neurointerv Surg. 2016; 8:2–7. PMID: 25378639.
Article34. Liebeskind DS, Tomsick T, Foster L, Yeatts SD, Carrozzella J, Demchuk AM, et al. Collaterals at angiography and outcomes in the Interventional management of stroke (IMS) III trial. Stroke. 2014; 45:759–764. PMID: 24473178.
Article35. Saver JL, Jahan R, Levy EI, Jovin TG, Baxter B, Nogueira RG, et al. Solitaire flow restoration device versus the Merci Retriever in patients with acute ischaemic stroke (SWIFT): a randomised, parallel-group, non-inferiority trial. Lancet. 2012; 380:1241–1249. PMID: 22932715.
Article36. Pan J, Konstas AA, Bateman B, Ortolano GA, Pile-Spellman J. Reperfusion injury following cerebral ischemia: Pathophysiology, MR imaging, and potential therapies. Neuroradiology. 2007; 49:93–102. PMID: 17177065.
Article37. Liebeskind DS, Sanossian N, Yong WH, Starkman S, Tsang MP, Moya AL, et al. CT and MRI early vessel signs reflect clot composition in acute stroke. Stroke. 2011; 42:1237–1243. PMID: 21393591.
Article38. Riedel CH, Zimmermann P, Jensen-Kondering U, Stingele R, Deuschl G, Jansen O. The importance of size: successful recanalization by intravenous thrombolysis in acute anterior stroke depends on thrombus length. Stroke. 2011; 42:1775–1777. PMID: 21474810.39. Shobha N, Bal S, Boyko M, Kroshus E, Menon BK, Bhatia R, et al. Measurement of length of Hyperdense MCA sign in acute Ischemic stroke predicts disappearance after IV tPA. J Neuroimaging. 2014; 24:7–10. PMID: 23316960.
Article40. Puetz V, Dzialowski I, Hill MD, Subramaniam S, Sylaja PN, Krol A, et al. Intracranial Thrombus extent predicts clinical outcome, final infarct size and Hemorrhagic transformation in Ischemic stroke: The clot burden score. Int J Stroke. 2008; 3:230–236. PMID: 18811738.
Article41. Qazi EM, Sohn SI, Mishra S, Almekhlafi MA, Eesa M, d'Esterre CD, et al. Thrombus Characteristics Are Related to Collaterals and Angioarchitecture in Acute Stroke. Can J Neurol Sci. 2015; 42:381–388. PMID: 26365832.
Article42. Schramm P, Schellinger PD, Klotz E, Kallenberg K, Fiebach JB, Külkens S, et al. Comparison of perfusion computed tomography and computed tomography angiography source images with perfusion-weighted imaging and diffusion-weighted imaging in patients with acute stroke of less than 6 hours' duration. Stroke. 2004; 35:1652–1658. PMID: 15155964.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Mechanical Thrombectomy in Strokes with Large-Vessel Occlusion Beyond 6 Hours: A Pooled Analysis of Randomized Trials
- Discrepancy in core infarct betweennon-contrast CT and CT perfusionwhen selecting for mechanicalthrombectomy
- Alberta Stroke Program Early CT Score in the Prognostication after Endovascular Treatment for Ischemic Stroke: A Meta-analysis
- Endovascular Stroke Therapy Focused on Stent Retriever Thrombectomy and Direct Clot Aspiration: Historical Review and Modern Application
- Intravenous Thrombolysis and Endovascular Thrombectomy in Acute Ischemic Stroke with Minor Symptom