Ann Rehabil Med.
2017 Jun;41(3):426-433. 10.5535/arm.2017.41.3.426.
Effects of Capping of the Tracheostomy Tube in Stroke Patients With Dysphagia
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Myongji Hospital, Seonam University College of Medicine, Goyang, Korea. rallo1080@naver.com
- KMID: 2389458
- DOI: http://doi.org/10.5535/arm.2017.41.3.426
Abstract
OBJECTIVE
To investigate the impact of tracheostomy tube capping on swallowing physiology in stroke patients with dysphagia via videofluoroscopic swallowing study (VFSS).
METHODS
This study was conducted as a prospective study that involved 30 stroke patients. Then, 4 mL semisolid swallowing was conducted with capping of the tracheostomy tube or without capping of the tracheostomy tube. The following five parameters were measured: laryngeal elevation, pharyngeal transit time, post-swallow pharyngeal remnant, upper esophageal sphincter width (UES), and penetration-aspiration scale (PAS) score.
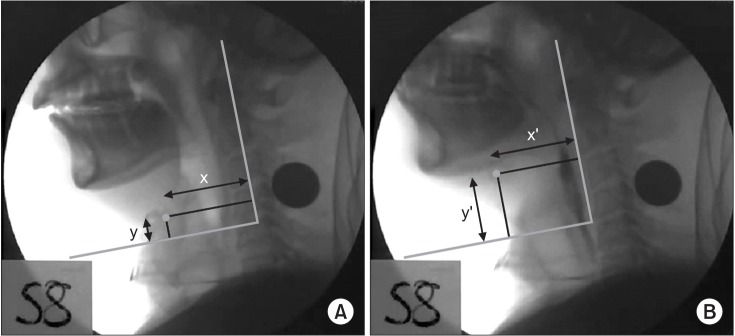
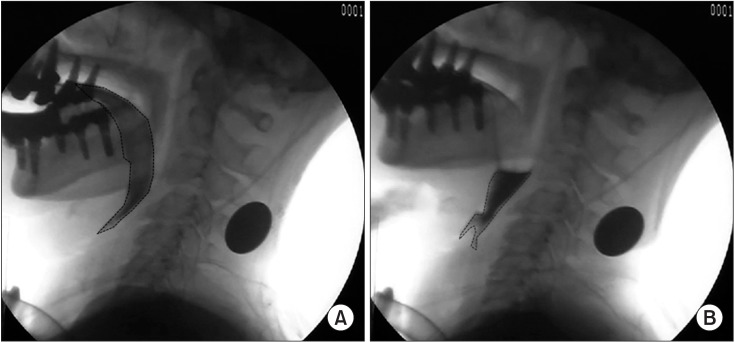
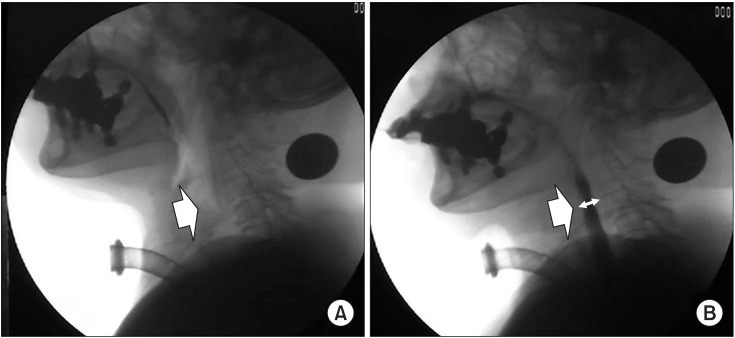
RESULTS
On assessment of the differences in swallowing parameters during swallowing between "˜with capping' and "˜without capping' statuses, statistically significant differences were found in the post-swallow pharyngeal remnant (without capping, 48.19%±28.70%; with capping, 25.09%±19.23%; p<0.001), normalized residue ratio scale for the valleculae (without capping, 0.17±0.12; with capping, 0.09±0.12; p=0.013), normalized residue ratio scale for the piriform sinus (without capping, 0.16±0.12; with capping, 0.10±0.07; p=0.015), and UES width (without capping, 3.32±1.61 mm; with capping, 4.61±1.95 mm; p=0.003). However, there were no statistically significant differences in laryngeal elevation (x-axis without capping, 2.48±1.45 mm; with capping, 3.26±2.37 mm; y-axis without capping, 11.11±5.24 mm; with capping, 12.64±6.16 mm), pharyngeal transit time (without capping, 9.19± 10.14 s; with capping, 9.09±10.21 s), and PAS score (without capping, 4.94±2.83; with capping, 4.18±2.24).
CONCLUSION
Tracheostomy tube capping is a useful way to reduce post-swallow remnants and it can be considered an alternative method for alleviating dysphagia in stroke patients who can tolerate tracheostomy tube capping when post-swallow remnants are observed.
Keyword
MeSH Terms
Figure
Reference
-
1. Goldenberg D, Ari EG, Golz A, Danino J, Netzer A, Joachims HZ. Tracheotomy complications: a retrospective study of 1130 cases. Otolaryngol Head Neck Surg. 2000; 123:495–500. PMID: 11020193.
Article2. Das P, Zhu H, Shah RK, Roberson DW, Berry J, Skinner ML. Tracheotomy-related catastrophic events: results of a national survey. Laryngoscope. 2012; 122:30–37. PMID: 22183626.
Article3. Mann G, Hankey GJ, Cameron D. Swallowing disorders following acute stroke: prevalence and diagnostic accuracy. Cerebrovasc Dis. 2000; 10:380–386. PMID: 10971024.
Article4. Falsetti P, Acciai C, Palilla R, Bosi M, Carpinteri F, Zingarelli A, et al. Oropharyngeal dysphagia after stroke: incidence, diagnosis, and clinical predictors in patients admitted to a neurorehabilitation unit. J Stroke Cerebrovasc Dis. 2009; 18:329–335. PMID: 19717014.
Article5. Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke. 2005; 36:2756–2763. PMID: 16269630.6. Bosel J. Tracheostomy in stroke patients. Curr Treat Options Neurol. 2014; 16:274. PMID: 24357462.
Article7. Walcott BP, Kamel H, Castro B, Kimberly WT, Sheth KN. Tracheostomy after severe ischemic stroke: a population-based study. J Stroke Cerebrovasc Dis. 2014; 23:1024–1029. PMID: 24103666.
Article8. Rabinstein AA, Wijdicks EF. Outcome of survivors of acute stroke who require prolonged ventilatory assistance and tracheostomy. Cerebrovasc Dis. 2004; 18:325–331. PMID: 15359100.
Article9. Muz J, Mathog RH, Nelson R, Jones LA Jr. Aspiration in patients with head and neck cancer and tracheostomy. Am J Otolaryngol. 1989; 10:282–286. PMID: 2764241.
Article10. DeVita MA, Spierer-Rundback L. Swallowing disorders in patients with prolonged orotracheal intubation or tracheostomy tubes. Crit Care Med. 1990; 18:1328–1330. PMID: 2245604.
Article11. Bonanno PC. Swallowing dysfunction after tracheostomy. Ann Surg. 1971; 174:29–33. PMID: 5092509.
Article12. Sasaki CT, Suzuki M, Horiuchi M, Kirchner JA. The effect of tracheostomy on the laryngeal closure reflex. Laryngoscope. 1977; 87(9 Pt 1):1428–1433. PMID: 895306.
Article13. Leder SB, Ross DA. Incidence of vocal fold immobility in patients with dysphagia. Dysphagia. 2005; 20:163–167. discussion 168-9. PMID: 16172827.
Article14. Gross RD, Steinhauer KM, Zajac DJ, Weissler MC. Direct measurement of subglottic air pressure while swallowing. Laryngoscope. 2006; 116:753–761. PMID: 16652083.
Article15. Kim YK, Choi JH, Yoon JG, Lee JW, Cho SS. Improved dysphagia after decannulation of tracheostomy in patients with brain injuries. Ann Rehabil Med. 2015; 39:778–785. PMID: 26605176.
Article16. Gross RD, Mahlmann J, Grayhack JP. Physiologic effects of open and closed tracheostomy tubes on the pharyngeal swallow. Ann Otol Rhinol Laryngol. 2003; 112:143–152. PMID: 12597287.
Article17. Elpern EH, Borkgren Okonek M, Bacon M, Gerstung C, Skrzynski M. Effect of the Passy-Muir tracheostomy speaking valve on pulmonary aspiration in adults. Heart Lung. 2000; 29:287–293. PMID: 10900066.
Article18. Stachler RJ, Hamlet SL, Choi J, Fleming S. Scintigraphic quantification of aspiration reduction with the Passy-Muir valve. Laryngoscope. 1996; 106(2 Pt 1):231–234. PMID: 8583860.
Article19. Eibling DE, Gross RD. Subglottic air pressure: a key component of swallowing efficiency. Ann Otol Rhinol Laryngol. 1996; 105:253–258. PMID: 8604883.
Article20. Rumbak MJ, Graves AE, Scott MP, Sporn GK, Walsh FW, Anderson WM, et al. Tracheostomy tube occlusion protocol predicts significant tracheal obstruction to air flow in patients requiring prolonged mechanical ventilation. Crit Care Med. 1997; 25:413–417. PMID: 9118655.
Article21. Pearson WG Jr, Molfenter SM, Smith ZM, Steele CM. Image-based measurement of post-swallow residue: the normalized residue ratio scale. Dysphagia. 2013; 28:167–177. PMID: 23089830.
Article22. Adzaku FK. The morphological and functional characteristics of the innervation of the subglottic mucosa of the larynx. Ann R Coll Surg Engl. 1980; 62:426–431. PMID: 7436302.23. Leder SB, Tarro JM, Burrell MI. Effect of occlusion of a tracheotomy tube on aspiration. Dysphagia. 1996; 11:254–258. PMID: 8870353.
Article24. Heitmiller RF, Tseng E, Jones B. Prevalence of aspiration and laryngeal penetration in patients with unilateral vocal fold motion impairment. Dysphagia. 2000; 15:184–187. PMID: 11014880.
Article25. Alfonsi E, Merlo IM, Ponzio M, Montomoli C, Tassorelli C, Biancardi C, et al. An electrophysiological approach to the diagnosis of neurogenic dysphagia: implications for botulinum toxin treatment. J Neurol Neurosurg Psychiatry. 2010; 81:54–60. PMID: 19762326.
Article26. Eisenhuber E, Schima W, Schober E, Pokieser P, Stadler A, Scharitzer M, et al. Videofluoroscopic assessment of patients with dysphagia: pharyngeal retention is a predictive factor for aspiration. AJR Am J Roentgenol. 2002; 178:393–398. PMID: 11804901.27. Kim JC, Kim JS, Jung JH, Kim YK. The effect of balloon dilatation through Video-Fluoroscopic Swallowing Study (VFSS) in stroke patients with cricopharyngeal dysfunction. J Korean Acad Rehabil Med. 2011; 35:23–26.28. Kim YK, Choi SS, Choi JH, Yoon JG. Effectiveness of rehabilitative balloon swallowing treatment on upper esophageal sphincter relaxation and pharyngeal motility for neurogenic dysphagia. Ann Rehabil Med. 2015; 39:524–534. PMID: 26361588.
Article29. Haapaniemi JJ, Laurikainen EA, Pulkkinen J, Marttila RJ. Botulinum toxin in the treatment of cricopharyngeal dysphagia. Dysphagia. 2001; 16:171–175. PMID: 11453562.
Article30. Ahsan SF, Meleca RJ, Dworkin JP. Botulinum toxin injection of the cricopharyngeus muscle for the treatment of dysphagia. Otolaryngol Head Neck Surg. 2000; 122:691–695. PMID: 10793348.
Article31. Dodds WJ, Logemann JA, Stewart ET. Radiologic assessment of abnormal oral and pharyngeal phases of swallowing. AJR Am J Roentgenol. 1990; 154:965–974. PMID: 2108570.
Article32. Cook IJ, Dodds WJ, Dantas RO, Massey B, Kern MK, Lang IM, et al. Opening mechanisms of the human upper esophageal sphincter. Am J Physiol. 1989; 257(5 Pt 1):G748–G759. PMID: 2596608.
Article33. Logemann JA, Pauloski BR, Rademaker AW, Colangelo LA, Kahrilas PJ, Smith CH. Temporal and biomechanical characteristics of oropharyngeal swallow in younger and older men. J Speech Lang Hear Res. 2000; 43:1264–1274. PMID: 11063246.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Dysphagia and Decannulation Following Tracheostomy in Children
- Effect of Tracheostomy Tube on Swallowing in Patients with Stroke
- Comparison of Percutaneous Endoscopic Gastrostomy and Nasogastric Tube Feeding in Dysphagic Stroke
- Interventional Management of Post-stroke Dysphagia
- Gastroesophageal Reflux during Nasogastric Tube Feeding versus Oroesophageal Tube Feeding in Stroke Patients: A 24 Hour Esophageal pH-monitoring