Ann Rehabil Med.
2017 Aug;41(4):638-649. 10.5535/arm.2017.41.4.638.
Korean Database of Cerebral Palsy: A Report on Characteristics of Cerebral Palsy in South Korea
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Ajou University School of Medicine, Suwon Korea.
- 2Rehabilitation Institute of Chicago, Chicago, IL, USA and The Seum Hospital, Jeonju, Korea.
- 3Department of Physical Medicine and Rehabilitation, The Catholic University of Korea, Seoul, Korea.
- 4Department of Physical Medicine and Rehabilitation, CHA University, Seongnam, Korea.
- 5Department of Physical Medicine and Rehabilitation, Pusan National University School of Medicine, Busan, Korea.
- 6Department of Physical Medicine and Rehabilitation, Kwangju Christian Hospital, Gwangju, Korea.
- 7Department of Physical Medicine and Rehabilitation, Daegu Fatima Hospital, Daegu, Korea.
- 8Department of Physical Medicine and Rehabilitation, Dongguk University College of Medicine, Goyang, Korea.
- 9Department of Physical Medicine and Rehabilitation, Hanmaeum Hospital, Jeju, Korea.
- 10Department of Physical Medicine and Rehabilitation, National Health Insurance Service Ilsan Hospital, Goyang, Korea.
- 11Department of Physical Medicine and Rehabilitation, Inha University School of Medicine, Incheon, Korea.
- 12Department of Physical Medicine and Rehabilitation, Sungkyunkwan University School of Medicine, Suwon, Korea.
- 13Department of Physical Medicine and Rehabilitation, University of Ulsan College of Medicine, Seoul, Korea. iysung@amc.seoul.kr
- KMID: 2389410
- DOI: http://doi.org/10.5535/arm.2017.41.4.638
Abstract
OBJECTIVE
To introduce the Korean Database of Cerebral Palsy (KDCP) and to provide the first report on characteristics of subjects with cerebral palsy (CP).
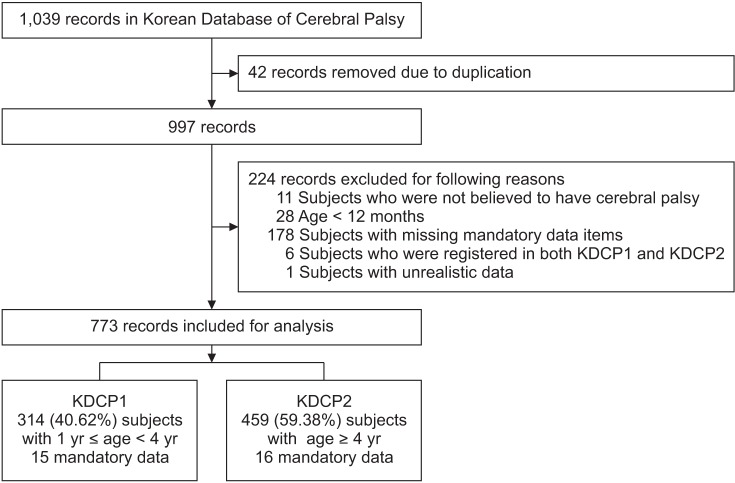
METHODS
The KDCP is a nationwide database of subjects with CP, which includes a total of 773 subjects. Characteristics such as demography, birth history, onset and type of CP, brain magnetic resonance imaging (MRI) findings, functional ability and accompanying impairments, were extracted and analyzed.
RESULTS
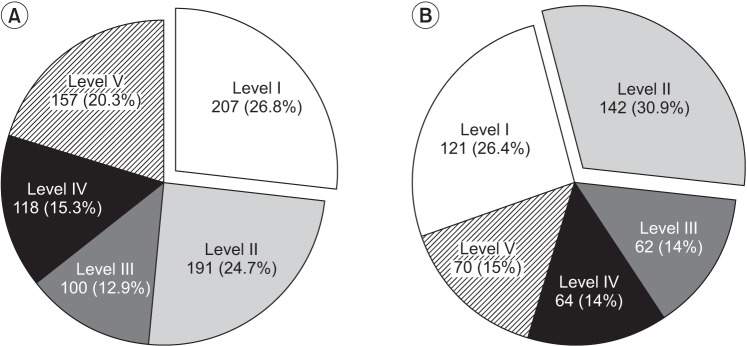
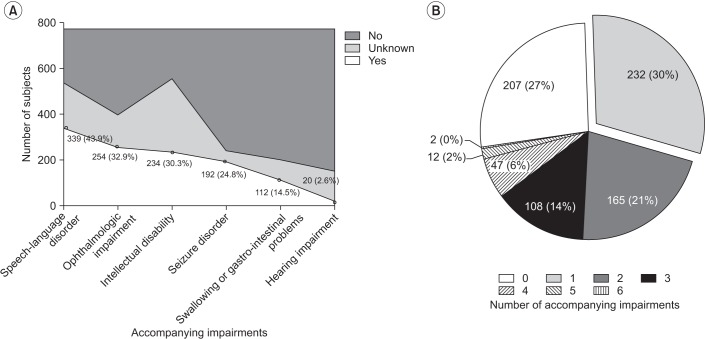
Preterm delivery and low birth weight were found in 59.51% and 60.28% of subjects, respectively. Postnatally acquired CP was 15.3%. The distribution of CP was 87.32%, 5.17%, and 1.81% for spastic, dyskinetic, and ataxic types, respectively. Functional ability was the worst in dyskinetic CP, as compared to other types of CP. Speech-language disorder (43.9%), ophthalmologic impairment (32.9%), and intellectual disability (30.3%) were the three most common accompanying impairments. The number of accompanying impairments was elevated in subjects with preterm birth and low birth weight. Brain MRI showed normal findings, malformations, and non-malformations in 10.62%, 9.56%, and 77.35% of subjects, respectively. Subjects with normal MRI findings had better functional ability than subjects with other MRI findings. MRI findings of a non-malformation origin, such as periventricular leukomalacia, were more common in subjects with preterm birth and low birth weight.
CONCLUSION
The KDCP and its first report are introduced in this report, wherein the KDCP established agreement on terminologies of CP. This study added information on the characteristics of subjects with CP in South Korea, which can now be compared to those of other countries and ethnicities.
Keyword
MeSH Terms
Figure
Cited by 3 articles
-
Cost of Rehabilitation Treatment of Patients With Cerebral Palsy in Korea
Seong Woo Kim, Ha Ra Jeon, Taemi Youk, Jiyong Kim
Ann Rehabil Med. 2018;42(5):722-729. doi: 10.5535/arm.2018.42.5.722.The Role of Regular Physical Therapy on Spasticity in Children With Cerebral Palsy
Heewon Lee, Eun Kyung Kim, Dong Baek Son, Youngdeok Hwang, Joon-Sung Kim, Seong Hoon Lim, Bomi Sul, Bo Young Hong
Ann Rehabil Med. 2019;43(3):289-296. doi: 10.5535/arm.2019.43.3.289.The Long-Term Outcome and Rehabilitative Approach of Intraventricular Hemorrhage at Preterm Birth
Juntaek Hong, Dong-wook Rha
J Korean Neurosurg Soc. 2023;66(3):289-297. doi: 10.3340/jkns.2022.0262.
Reference
-
1. Rosenbaum P, Paneth N, Leviton A, Goldstein M, Bax M, Damiano D, et al. A report: the definition and classification of cerebral palsy April 2006. Dev Med Child Neurol Suppl. 2007; 109:8–14. PMID: 17370477.2. Mantovani JF. Definition and classification of CP: medical-legal and service implications. Dev Med Child Neurol Suppl. 2007; 109:42. PMID: 17370482.3. Prevalence and characteristics of children with cerebral palsy in Europe. Dev Med Child Neurol. 2002; 44:633–640. PMID: 12227618.4. Jessen C, Mackie P, Jarvis S. Epidemiology of cerebral palsy. Arch Dis Child Fetal Neonatal Ed. 1999; 80:F158.
Article5. Paneth N, Hong T, Korzeniewski S. The descriptive epidemiology of cerebral palsy. Clin Perinatol. 2006; 33:251–267. PMID: 16765723.
Article6. Shevell M, Dagenais L, Oskoui M. The epidemiology of cerebral palsy: new perspectives from a Canadian registry. Semin Pediatr Neurol. 2013; 20:60–64. PMID: 23948680.
Article7. Froslev-Friis C, Dunkhase-Heinl U, Andersen JD, Stausbol-Gron B, Hansen AV, Garne E. Epidemiology of cerebral palsy in Southern Denmark. Dan Med J. 2015; 62:A4990. PMID: 25557331.8. Dolk H, Pattenden S, Bonellie S, Colver A, King A, Kurinczuk JJ, et al. Socio-economic inequalities in cerebral palsy prevalence in the United Kingdom: a register-based study. Paediatr Perinat Epidemiol. 2010; 24:149–155. PMID: 20415771.
Article9. Ferreira MC, Di Naccio BL, Otsuka MY, de Melo Barbosa A, Correa PF, Gardenghi G. Assessing the burden on primary caregivers of children with cerebral palsy and its relation to quality of life and socioeconomic aspects. Acta Fisiatr. 2015; 22:9–13.
Article10. Surveillance of Cerebral Palsy in Europe. Surveillance of cerebral palsy in Europe: a collaboration of cerebral palsy surveys and registers. Surveillance of Cerebral Palsy in Europe (SCPE). Dev Med Child Neurol. 2000; 42:816–824. PMID: 11132255.11. Morris C. Development of the gross motor function classification system (1997). Dev Med Child Neurol. 2008; 50:5. PMID: 18173618.
Article12. Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol. 1997; 39:214–223. PMID: 9183258.
Article13. Wood E, Rosenbaum P. The gross motor function classification system for cerebral palsy: a study of reliability and stability over time. Dev Med Child Neurol. 2000; 42:292–296. PMID: 10855648.
Article14. Reid SM, Carlin JB, Reddihough DS. Using the Gross Motor Function Classification System to describe patterns of motor severity in cerebral palsy. Dev Med Child Neurol. 2011; 53:1007–1012. PMID: 22014320.
Article15. Carnahan KD, Arner M, Hagglund G. Association between gross motor function (GMFCS) and manual ability (MACS) in children with cerebral palsy: a population-based study of 359 children. BMC Musculoskelet Disord. 2007; 8:50. PMID: 17584944.
Article16. Eliasson AC, Krumlinde-Sundholm L, Rosblad B, Beckung E, Arner M, Ohrvall AM, et al. The Manual Ability Classification System (MACS) for children with cerebral palsy: scale development and evidence of validity and reliability. Dev Med Child Neurol. 2006; 48:549–554. PMID: 16780622.
Article17. Morris C, Kurinczuk JJ, Fitzpatrick R, Rosenbaum PL. Reliability of the manual ability classification system for children with cerebral palsy. Dev Med Child Neurol. 2006; 48:950–953. PMID: 17109781.
Article18. Reid SM, Lanigan A, Reddihough DS. Post-neonatally acquired cerebral palsy in Victoria, Australia, 1970-1999. J Paediatr Child Health. 2006; 42:606–611. PMID: 16972967.
Article19. Cans C, McManus V, Crowley M, Guillem P, Platt MJ, Johnson A, et al. Cerebral palsy of post-neonatal origin: characteristics and risk factors. Paediatr Perinat Epidemiol. 2004; 18:214–220. PMID: 15130161.
Article20. Bax M, Tydeman C, Flodmark O. Clinical and MRI correlates of cerebral palsy: the European Cerebral Palsy Study. JAMA. 2006; 296:1602–1608. PMID: 17018805.21. Himmelmann K, Uvebrant P. Function and neuroimaging in cerebral palsy: a population-based study. Dev Med Child Neurol. 2011; 53:516–521. PMID: 21574988.
Article22. Himmelmann K, Sundh V. Survival with cerebral palsy over five decades in western Sweden. Dev Med Child Neurol. 2015; 57:762–767. PMID: 25694102.
Article23. Korean Statistical Information Service. Evaluation result of caesarean section in 2013 [Internet]. Seoul: Statistics Korea;c2017. cited 2017 Jul 1. Available from: http://kosis.kr/.24. Surman G, Bonellie S, Chalmers J, Colver A, Dolk H, Hemming K, et al. UKCP: a collaborative network of cerebral palsy registers in the United Kingdom. J Public Health (Oxf). 2006; 28:148–156. PMID: 16556625.
Article25. Robinson MN, Peake LJ, Ditchfield MR, Reid SM, Lanigan A, Reddihough DS. Magnetic resonance imaging findings in a population-based cohort of children with cerebral palsy. Dev Med Child Neurol. 2009; 51:39–45. PMID: 19018841.
Article26. Benini R, Dagenais L, Shevell MI. Registre de la Paralysie Cerebrale au Quebec (Quebec Cerebral Palsy Registry) Consortium. Quebec Cerebral Palsy Registry) Consortium. Normal imaging in patients with cerebral palsy: what does it tell us? J Pediatr. 2013; 162:369–374. PMID: 22944004.27. Cans C, Surman G, McManus V, Coghlan D, Hensey O, Johnson A. Cerebral palsy registries. Semin Pediatr Neurol. 2004; 11:18–23. PMID: 15132250.
Article28. Platt MJ, Krageloh-Mann I, Cans C. Surveillance of cerebral palsy in europe: reference and training manual. Med Educ. 2009; 43:495–496. PMID: 19422516.
Article29. Zarrinkalam R, Russo RN, Gibson CS, van Essen P, Peek AK, Haan EA. CP or not CP? A review of diagnoses in a cerebral palsy register. Pediatr Neurol. 2010; 42:177–180. PMID: 20159426.
Article30. Sigurdardottir S, Thorkelsson T, Halldorsdottir M, Thorarensen O, Vik T. Trends in prevalence and characteristics of cerebral palsy among Icelandic children born 1990 to 2003. Dev Med Child Neurol. 2009; 51:356–363. PMID: 19388148.31. Ravn SH, Flachs EM, Uldall P. Cerebral palsy in eastern Denmark: declining birth prevalence but increasing numbers of unilateral cerebral palsy in birth year period 1986-1998. Eur J Paediatr Neurol. 2010; 14:214–218. PMID: 19564124.
Article32. Andersen GL, Irgens LM, Haagaas I, Skranes JS, Meberg AE, Vik T. Cerebral palsy in Norway: prevalence, subtypes and severity. Eur J Paediatr Neurol. 2008; 12:4–13. PMID: 17574886.
Article33. Topp M, Huusom LD, Langhoff-Roos J, Delhumeau C, Hutton JL, Dolk H, et al. Multiple birth and cerebral palsy in Europe: a multicenter study. Acta Obstet Gynecol Scand. 2004; 83:548–553. PMID: 15144336.
Article34. Hayes BC, Ryan S, McGarvey C, Mulvany S, Doherty E, Grehan A, et al. Brain magnetic resonance imaging and outcome after hypoxic ischaemic encephalopathy. J Matern Fetal Neonatal Med. 2016; 29:777–782. PMID: 25754207.
Article35. O'Callaghan M, MacLennan A. Cesarean delivery and cerebral palsy: a systematic review and meta-analysis. Obstet Gynecol. 2013; 122:1169–1175. PMID: 24201683.