Anesth Pain Med.
2017 Jul;12(3):251-255. 10.17085/apm.2017.12.3.251.
Anesthetic management with extracorporeal membrane oxygenation in a patient with acute airway obstruction after inhalation burn injury: A case report
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea. s2248@paik.ac.kr
- KMID: 2388842
- DOI: http://doi.org/10.17085/apm.2017.12.3.251
Abstract
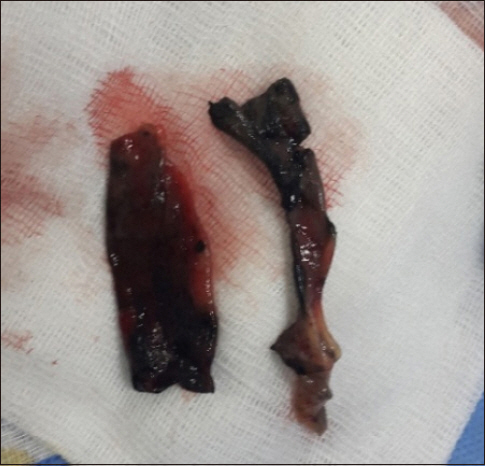
- A 36-year-old woman was admitted to the intensive care unit because of an inhalation burn injury. Five days after admission, she developed dyspnea and hypercarbia. Therefore, fiberoptic bronchoscopy was performed through the endotracheal tube, which revealed foreign bodies in the tube. Tracheostomy was performed to remove, albeit incompletely, the foreign bodies (endotracheal debris). As sudden movement of the patient or airway reaction could cause the foreign bodies to move deeper into the bronchus during manipulation of the rigid bronchoscope, general anesthesia was induced and maintained by using total intravenous anesthesia with extracorporeal membrane oxygenation (ECMO). The foreign bodies were successfully removed without any other complications. This case showed that sloughed endobronchial debris after an inhalation burn injury caused acute airway obstruction. In such cases, alternative ventilation methods such as tracheostomy and ECMO may have to be applied, which can support a surgeon to focus on the procedure regardless of prolonged procedural time.
Keyword
MeSH Terms
Figure
Reference
-
1. You K, Yang HT, Kym D, Yoon J, Haejun Yim, Cho YS, et al. Inhalation injury in burn patients: establishing the link between diagnosis and prognosis. Burns. 2014; 40:1470–5. DOI: 10.1016/j.burns.2014.09.015. PMID: 25406889.2. Bishop S, Maguire S. Anaesthesia and intensive care for major burns. Contin Educ Anaesth Crit Care Pain. 2012; 12:118–22. DOI: 10.1093/bjaceaccp/mks001.3. Edelman DA, White MT, Tyburski JG, Wilson RF. Factors affecting prognosis of inhalation injury. J Burn Care Res. 2006; 27:848–53. DOI: 10.1097/01.BCR.0000245493.26814.CE. PMID: 17091081.4. Luo G, Peng Y, Yuan Z, Liu Y, Cheng W, Huang Y, et al. Inhalation injury in southwest China--the evolution of care. Burns. 2010; 36:506–10. DOI: 10.1016/j.burns.2009.07.008. PMID: 19857928.5. Mlcak RP, Suman OE, Herndon DN. Respiratory management of inhalation injury. Burns. 2007; 33:2–13. DOI: 10.1016/j.burns.2006.07.007. PMID: 17223484.6. Fang-Gang N, Yang C, Yu-Xuan Q, Yan-Hua R, Wei-Li D, Cheng W, et al. Laryngeal morphologic changes and epidemiology in patients with inhalation injury: a retrospective study. Burns. 2015; 41:1340–6. DOI: 10.1016/j.burns.2015.02.003. PMID: 25791918.7. Antunes MB, Cohen NA. Mucociliary clearance--a critical upper airway host defense mechanism and methods of assessment. Curr Opin Allergy Clin Immunol. 2007; 7:5–10. DOI: 10.1097/ACI.0b013e3280114eef. PMID: 17218804.8. Kwon MA, Kim HS, Oh JY, Song BK, Song JK. Gene cloning, expression, and characterization of a new carboxylesterase from Serratia sp. SES-01: comparison with Escherichia coli BioHe enzyme. J Microbiol Biotechnol. 2009; 19:147–54. DOI: 10.4014/jmb.0804.287. PMID: 19307763.9. Cancio LC. Airway management and smoke inhalation injury in the burn patient. Clin Plast Surg. 2009; 36:555–67. DOI: 10.1016/j.cps.2009.05.013. PMID: 19793551.10. Palmieri TL, Jackson W, Greenhalgh DG. Benefits of early tracheostomy in severely burned children. Crit Care Med. 2002; 30:922–4. DOI: 10.1097/00003246-200204000-00036. PMID: 11940771.11. Herndon DN, Thompson PB, Traber DL. Pulmonary injury in burned patients. Crit Care Clin. 1985; 1:79–96. PMID: 3916776.12. Willms DC, Mendez R, Norman V, Chammas JH. Emergency bedside extracorporeal membrane oxygenation for rescue of acute tracheal obstruction. Respir Care. 2012; 57:646–9. DOI: 10.4187/respcare.01417. PMID: 22472502.13. Kim H, Jeong SM, Kim H, Ryu HG. Successful use of extracorporeal membrane oxygenation for sudden aggravation of acute respiratory distress syndrome: A case report. Anesth Pain Med. 2013; 8:279–81.14. Chen A. ECMO-assisted rigid bronchoscopy for tracheal obstruction. J Bronchology Interv Pulmonol. 2009; 16:296–7. DOI: 10.1097/LBR.0b013e3181b767ff. PMID: 23168599.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Inhalation Burn-Induced Extensive Tracheal Inflammatory Crust Removed by Ventilating Bronchoscopy under Tracheostomy and Extracorporeal Membrane Oxygenation
- Anesthetic management of a patient with nitric acid inhalation injury for extracorporeal membrane oxygenation
- Extracorporeal Membrane Oxygenation as a Bridge to Definitive Airway Security in 3 Severe Acute Extrinsic Airway Compression Patients: A Case Report
- Tracheostomy Assisted with Emergency Bypass System in Severe Tracheal Stenosis
- Emergency Bilobectomy under the Extracorporeal Membrane Oxygenation Support for Pediatric Patient with Blunt Traumatic Bronchial Transection: A case report