Investig Clin Urol.
2017 May;58(3):152-163. 10.4111/icu.2017.58.3.152.
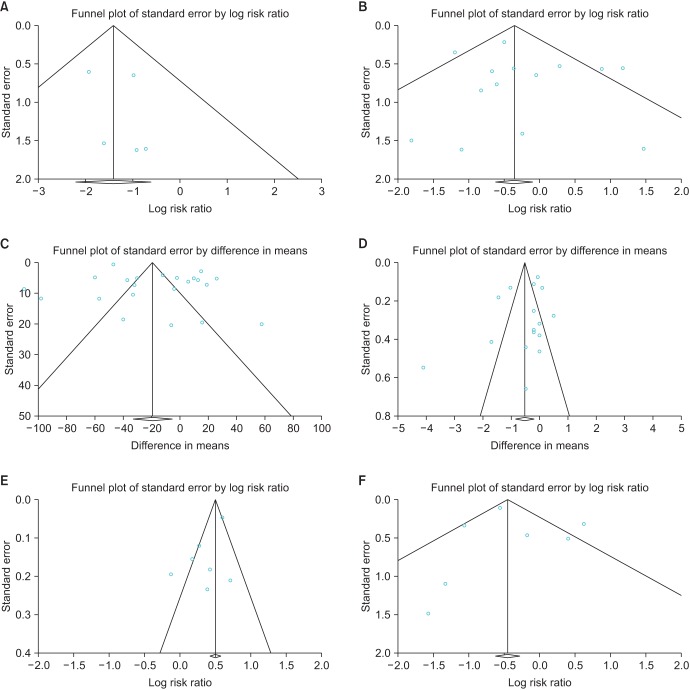
Robot-assisted radical prostatectomy has lower biochemical recurrence than laparoscopic radical prostatectomy: Systematic review and meta-analysis
- Affiliations
-
- 1Department of Nursing Science, Gachon University College of Nursing, Incheon, Korea.
- 2Department of Nursing, Chosun University College of Medicine, Gwangju, Korea.
- 3Department of Health Technology Assessment, National Evidence-Based Healthcare Collaborating Agency, Seoul, Korea.
- 4Department of Urology, CHA Seoul Station Medical Center, CHA University, CHA Medical School, Seoul, Korea.
- 5Department of Urology, Hanyang University School of Medicine, Graduate School, Seoul, Korea.
- 6Department of Urology, Urological Science Institute, Yonsei University College of Medicine, Seoul, Korea. khrha@yuhs.ac
- KMID: 2388059
- DOI: http://doi.org/10.4111/icu.2017.58.3.152
Abstract
- PURPOSE
To assess the effectiveness and safety of robot-assisted radical prostatectomy (RARP) versus laparoscopic radical prostatectomy (LRP) in the treatment of prostate cancer.
MATERIALS AND METHODS
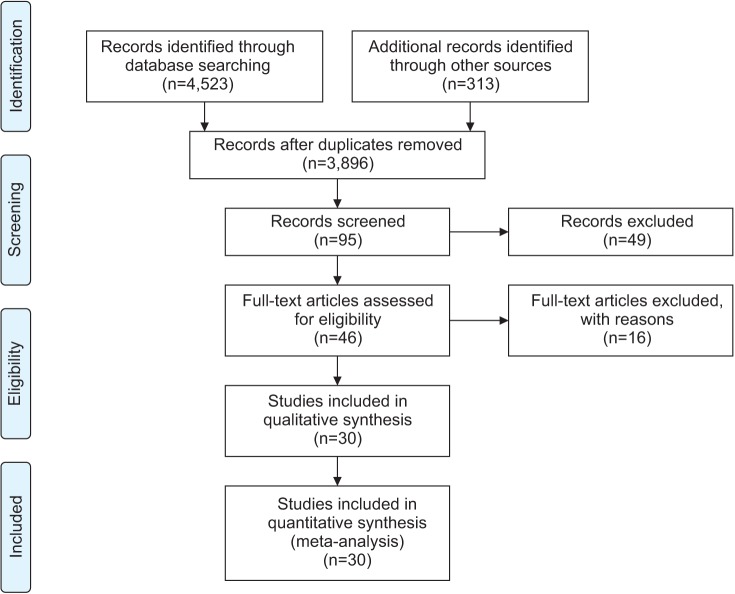
Existing systematic reviews were updated to investigate the effectiveness and safety of RARP. Electronic databases, including Ovid MEDLINE, Ovid Embase, the Cochrane Library, KoreaMed, Kmbase, and others, were searched through July 2014. The quality of the selected systematic reviews was assessed by using the revised assessment of multiple systematic reviews (R-Amstar) and the Cochrane Risk of Bias tool. Meta-analysis was performed by using Revman 5.2 (Cochrane Community) and Comprehensive Meta-Analysis 2.0 (CMA; Biostat). Cochrane Q and I2 statistics were used to assess heterogeneity.
RESULTS
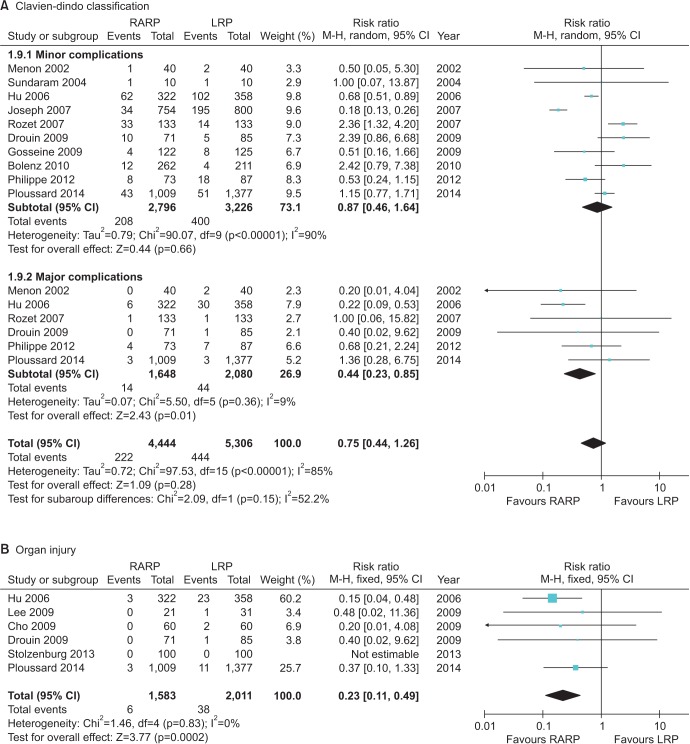
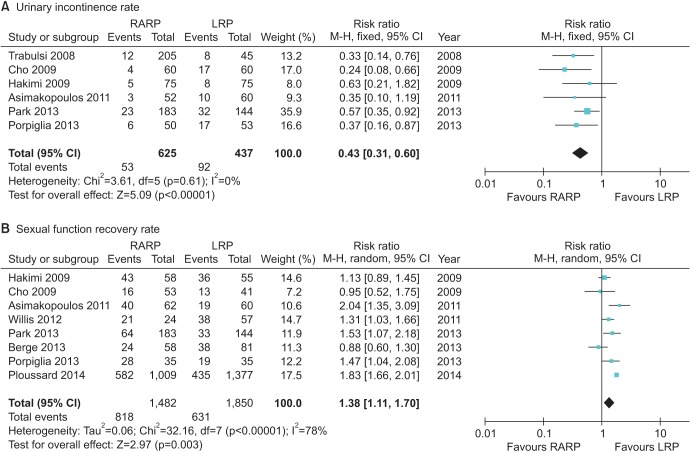
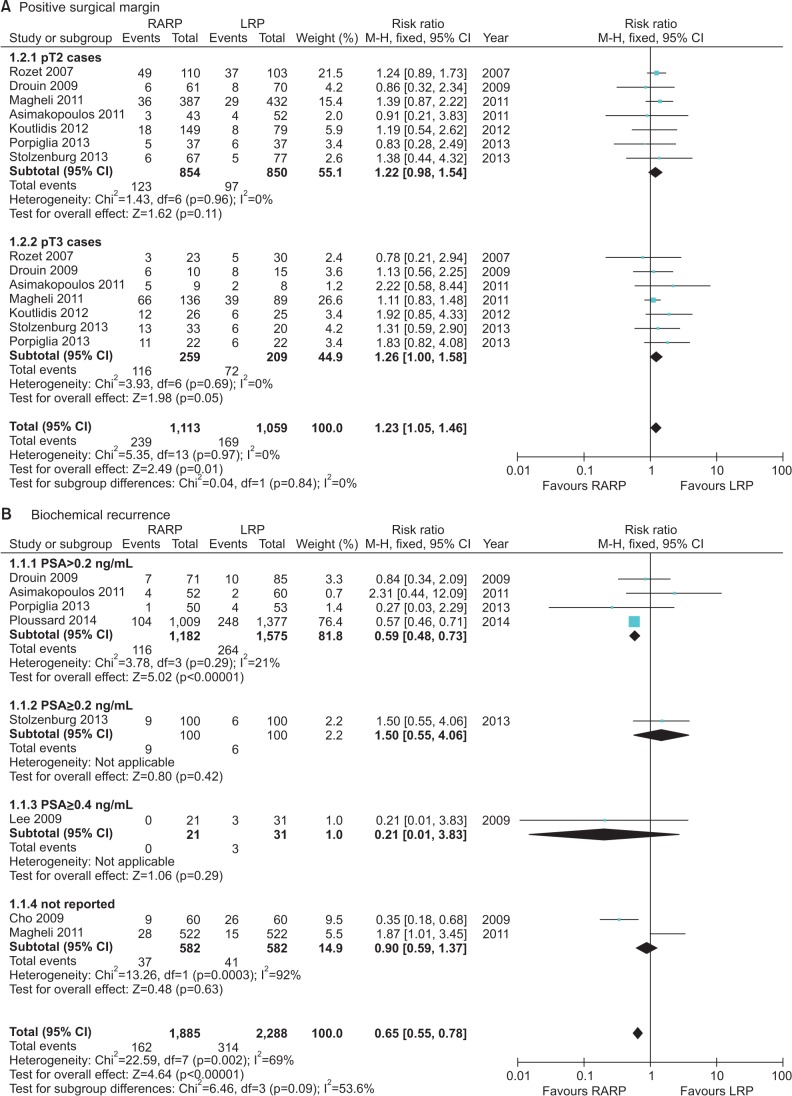
Two systematic reviews and 16 additional studies were selected from a search performed of existing systematic reviews. These included 2 randomized controlled clinical trials and 28 nonrandomized comparative studies. The risk of complications, such as injury to organs by the Clavien-Dindo classification, was lower with RARP than with LRP (relative risk [RR], 0.44; 95% confidence interval [CI], 1.23-0.85; p=0.01). The risk of urinary incontinence was lower (RR, 0.43; 95% CI, 0.31-0.60; p<0.000001) and the potency rate was significantly higher with RARP than with LRP (RR, 1.38; 95% CI, 1.11-1.70; I²=78%; p=0.003). Regarding positive surgical margins, no significant difference in risk between the 2 groups was observed; however, the biochemical recurrence rate was lower after RARP than after LRP (RR, 0.59; 95% CI, 0.48-0.73; I²=21%; p<0.00001).
CONCLUSIONS
RARP appears to be a safe and effective technique compared with LRP with a lower complication rate, better potency, a higher continence rate, and a decreased rate of biochemical recurrence.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Oncological and functional outcomes following robot-assisted laparoscopic radical prostatectomy at a single institution: a minimum 5-year follow-up
Jun-Koo Kang, Jae-Wook Chung, So Young Chun, Yun-Sok Ha, Seock Hwan Choi, Jun Nyung Lee, Bum Soo Kim, Ghil Suk Yoon, Hyun Tae Kim, Tae-Hwan Kim, Tae Gyun Kwon
Yeungnam Univ J Med. 2018;35(2):171-178. doi: 10.12701/yujm.2018.35.2.171.
Reference
-
1. Berge V, Berg RE, Hoff JR, Wessel N, Diep LM, Karlsen SJ, et al. A prospective study of transition from laparoscopic to robot-assisted radical prostatectomy: quality of life outcomes after 36-month follow-up. Urology. 2013; 81:781–786. PMID: 23465150.
Article2. Asimakopoulos AD, Miano R, Di Lorenzo N, Spera E, Vespasiani G, Mugnier C. Laparoscopic versus robot-assisted bilateral nerve-sparing radical prostatectomy: comparison of pentafecta rates for a single surgeon. Surg Endosc. 2013; 27:4297–4304. PMID: 23807752.
Article3. Lee YS, Han WK, Oh YT, Choi YD, Yang SC, Rha KH. Robot-assisted laparoscopic radical prostatectomy: four cases. Yonsei Med J. 2007; 48:341–346. PMID: 17461539.
Article4. Ahlering TE, Skarecky D, Borin J. Impact of cautery versus cautery-free preservation of neurovascular bundles on early return of potency. J Endourol. 2006; 20:586–589. PMID: 16903820.
Article5. Sanda MG, Dunn RL, Michalski J, Sandler HM, Northouse L, Hembroff L, et al. Quality of life and satisfaction with outcome among prostate-cancer survivors. N Engl J Med. 2008; 358:1250–1261. PMID: 18354103.
Article6. van der Poel HG, de Blok W, Joshi N, van Muilekom E. Preservation of lateral prostatic fascia is associated with urine continence after robotic-assisted prostatectomy. Eur Urol. 2009; 55:892–900. PMID: 19171418.
Article7. Borin JF, Skarecky DW, Narula N, Ahlering TE. Impact of urethral stump length on continence and positive surgical margins in robot-assisted laparoscopic prostatectomy. Urology. 2007; 70:173–177. PMID: 17656233.
Article8. Novara G, Ficarra V, D'elia C, Secco S, Cioffi A, Cavalleri S, et al. Evaluating urinary continence and preoperative predictors of urinary continence after robot assisted laparoscopic radical prostatectomy. J Urol. 2010; 184:1028–1033. PMID: 20643426.
Article9. Asimakopoulos AD, Pereira Fraga CT, Annino F, Pasqualetti P, Calado AA, Mugnier C. Randomized comparison between laparoscopic and robot-assisted nerve-sparing radical prostatectomy. J Sex Med. 2011; 8:1503–1512. PMID: 21324093.
Article10. Patel VR, Coelho RF, Palmer KJ, Rocco B. Periurethral suspension stitch during robot-assisted laparoscopic radical prostatectomy: description of the technique and continence outcomes. Eur Urol. 2009; 56:472–478. PMID: 19560260.
Article11. Coelho RF, Chauhan S, Orvieto MA, Sivaraman A, Palmer KJ, Coughlin G, et al. Influence of modified posterior reconstruction of the rhabdosphincter on early recovery of continence and anastomotic leakage rates after robot-assisted radical prostatectomy. Eur Urol. 2011; 59:72–80. PMID: 20801579.
Article12. Patel VR, Sivaraman A, Coelho RF, Chauhan S, Palmer KJ, Orvieto MA, et al. Pentafecta: a new concept for reporting outcomes of robot-assisted laparoscopic radical prostatectomy. Eur Urol. 2011; 59:702–707. PMID: 21296482.
Article13. Ficarra V, Novara G, Fracalanza S, D'Elia C, Secco S, Iafrate M, et al. A prospective, non-randomized trial comparing robot-assisted laparoscopic and retropubic radical prostatectomy in one European institution. BJU Int. 2009; 104:534–539. PMID: 19281468.
Article14. Menon M, Shrivastava A, Bhandari M, Satyanarayana R, Siva S, Agarwal PK. Vattikuti Institute prostatectomy: technical modifications in 2009. Eur Urol. 2009; 56:89–96. PMID: 19403236.
Article15. Shikanov S, Woo J, Al-Ahmadie H, Katz MH, Zagaja GP, Shalhav AL, et al. Extrafascial versus interfascial nerve-sparing technique for robotic-assisted laparoscopic prostatectomy: comparison of functional outcomes and positive surgical margins characteristics. Urology. 2009; 74:611–616. PMID: 19616830.
Article16. Heidenreich A, Bastian PJ, Bellmunt J, Bolla M, Joniau S, van der Kwast T, et al. EAU guidelines on prostate cancer. Part II: Treatment of advanced, relapsing, and castration-resistant prostate cancer. Eur Urol. 2014; 65:467–479. PMID: 24321502.
Article17. Menon M, Bhandari M, Gupta N, Lane Z, Peabody JO, Rogers CG, et al. Biochemical recurrence following robot-assisted radical prostatectomy: analysis of 1384 patients with a median 5-year follow-up. Eur Urol. 2010; 58:838–846. PMID: 20869162.
Article18. Porpiglia F, Morra I, Lucci Chiarissi M, Manfredi M, Mele F, Grande S, et al. Randomised controlled trial comparing laparoscopic and robot-assisted radical prostatectomy. Eur Urol. 2013; 63:606–614. PMID: 22840353.
Article19. Kim KH, Lim SK, Shin TY, Chung BH, Hong SJ, Rha KH. Biochemical outcomes after robot-assisted radical prostatectomy in patients with follow-up more than 5-years. Asian J Androl. 2013; 15:404–408. PMID: 23524532.
Article20. Hashimoto T, Yoshioka K, Gondo T, Ozu C, Horiguchi Y, Namiki K, et al. Preoperative prognostic factors for biochemical recurrence after robot-assisted radical prostatectomy in Japan. Int J Clin Oncol. 2014; 19:702–707. PMID: 24048883.
Article21. Choo MS, Cho SY, Ko K, Jeong CW, Lee SB, Ku JH, et al. Impact of positive surgical margins and their locations after radical prostatectomy: comparison of biochemical recurrence according to risk stratification and surgical modality. World J Urol. 2014; 32:1401–1409. PMID: 24362883.
Article22. Shikanov S, Song J, Royce C, Al-Ahmadie H, Zorn K, Steinberg G, et al. Length of positive surgical margin after radical prostatectomy as a predictor of biochemical recurrence. J Urol. 2009; 182:139–144. PMID: 19450829.
Article23. Bolenz C, Gupta A, Hotze T, Ho R, Cadeddu JA, Roehrborn CG, et al. Cost comparison of robotic, laparoscopic, and open radical prostatectomy for prostate cancer. Eur Urol. 2010; 57:453–458. PMID: 19931979.
Article24. Durand X, Vaessen C, Bitker MO, Richard F. Retropubic, laparoscopic and robot-assisted total prostatectomies: comparison of postoperative course and histological and functional results based on a series of 86 prostatectomies. Prog Urol. 2008; 18:60–67. PMID: 18342158.25. Hakimi AA, Blitstein J, Feder M, Shapiro E, Ghavamian R. Direct comparison of surgical and functional outcomes of robotic-assisted versus pure laparoscopic radical prostatectomy: single-surgeon experience. Urology. 2009; 73:119–123. PMID: 18952268.
Article26. Ball AJ, Gambill B, Fabrizio MD, Davis JW, Given RW, Lynch DF, et al. Prospective longitudinal comparative study of early health-related quality-of-life outcomes in patients undergoing surgical treatment for localized prostate cancer: a short-term evaluation of five approaches from a single institution. J Endourol. 2006; 20:723–731. PMID: 17094746.27. Drouin SJ, Vaessen C, Hupertan V, Comperat E, Misraï V, Haertig A, et al. Comparison of mid-term carcinologic control obtained after open, laparoscopic, and robot-assisted radical prostatectomy for localized prostate cancer. World J Urol. 2009; 27:599–605. PMID: 19421755.
Article28. Gosseine PN, Mangin P, Leclers F, Cormier L. Pure laparoscopic versus robotic-assisted laparoscopic radical prostatectomy: comparative study to assess functional urinary outcomes. Prog Urol. 2009; 19:611–617. PMID: 19800550.29. Hu JC, Nelson RA, Wilson TG, Kawachi MH, Ramin SA, Lau C, et al. Perioperative complications of laparoscopic and robotic assisted laparoscopic radical prostatectomy. J Urol. 2006; 175:541–546. PMID: 16406991.
Article30. Joseph JV, Vicente I, Madeb R, Erturk E, Patel HR. Robot-assisted vs pure laparoscopic radical prostatectomy: are there any differences? BJU Int. 2005; 96:39–42. PMID: 15963117.
Article31. Rozet F, Jaffe J, Braud G, Harmon J, Cathelineau X, Barret E, et al. A direct comparison of robotic assisted versus pure laparoscopic radical prostatectomy: a single institution experience. J Urol. 2007; 178:478–482. PMID: 17561160.
Article32. Trabulsi EJ, Linden RA, Gomella LG, McGinnis DE, Strup SE, Lallas CD. The addition of robotic surgery to an established laparoscopic radical prostatectomy program: effect on positive surgical margins. Can J Urol. 2008; 15:3994–3999. PMID: 18405448.33. Cho JW, Kim TH, Sung GT. Laparoscopic radical prostatectomy versus robot-assisted laparoscopic radical prostatectomy: a single surgeon's experience. Korean J Urol. 2009; 50:1198–1202.
Article34. Kasraeian A, Barret E, Chan J, Sanchez-Salas R, Validire P, Cathelineau X, et al. Comparison of the rate, location and size of positive surgical margins after laparoscopic and robot-assisted laparoscopic radical prostatectomy. BJU Int. 2011; 108:1174–1178. PMID: 21392221.
Article35. Kermarrec I, Mangin P, Koutlidis N, Mourey E, Cormier L. Does robotics improve laparoscopic radical prostatectomy in complex surgical cases? Prog Urol. 2010; 20:638–643. PMID: 20951932.36. Koutlidis N, Mourey E, Champigneulle J, Mangin P, Cormier L. Robot-assisted or pure laparoscopic nerve-sparing radical prostatectomy: what is the optimal procedure for the surgical margins? A single center experience. Int J Urol. 2012; 19:1076–1081. PMID: 22860572.
Article37. Lee HW, Lee HM, Seo SI. Comparison of initial surgical outcomes between laparoscopic radical prostatectomy and robot-assisted laparoscopic radical prostatectomy performed by a single surgeon. Korean J Urol. 2009; 50:468–474.
Article38. Magheli A, Gonzalgo ML, Su LM, Guzzo TJ, Netto G, Humphreys EB, et al. Impact of surgical technique (open vs laparoscopic vs robotic-assisted) on pathological and biochemical outcomes following radical prostatectomy: an analysis using propensity score matching. BJU Int. 2011; 107:1956–1962. PMID: 21044243.
Article39. Nakamura LY, Nunez RN, Castle EP, Andrews PE, Humphreys MR. Different approaches to an inguinal hernia repair during a simultaneous robot-assisted radical prostatectomy. J Endourol. 2011; 25:621–624. PMID: 21355775.
Article40. Park B, Kim W, Jeong BC, Jeon SS, Lee HM, Choi HY, et al. Comparison of oncological and functional outcomes of pure versus robotic-assisted laparoscopic radical prostatectomy performed by a single surgeon. Scand J Urol. 2013; 47:10–18. PMID: 22835035.
Article41. Ploussard G, de la Taille A, Moulin M, Vordos D, Hoznek A, Abbou CC, et al. Comparisons of the perioperative, functional, and oncologic outcomes after robot-assisted versus pure extraperitoneal laparoscopic radical prostatectomy. Eur Urol. 2014; 65:610–619. PMID: 23245815.
Article42. Stolzenburg JU, Qazi HA, Holze S, Mende M, Nicolaus M, Franz T, et al. Evaluating the learning curve of experienced laparoscopic surgeons in robot-assisted radical prostatectomy. J Endourol. 2013; 27:80–85. PMID: 22834963.
Article43. Willis DL, Gonzalgo ML, Brotzman M, Feng Z, Trock B, Su LM. Comparison of outcomes between pure laparoscopic vs robot-assisted laparoscopic radical prostatectomy: a study of comparative effectiveness based upon validated quality of life outcomes. BJU Int. 2012; 109:898–905. PMID: 21933328.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- CORRIGENDUM: Correction of the Figure. Robot-assisted radical prostatectomy has lower biochemical recurrence than laparoscopic radical prostatectomy: Systematic review and meta-analysis
- Erratum: Robot-Assisted Laparoscopic Radical Prostatectomy
- Robot-Assisted Laparoscopic Radical Prostatectomy
- A Case of Robot-Assisted Laparoscopic Radical Prostatectomy in Primary Small Cell Prostate Cancer
- Floating Hem-o-Lok Clips in the Bladder without Stone Formation after Robot-Assisted Laparoscopic Radical Prostatectomy