J Korean Neurosurg Soc.
2017 Jul;60(4):456-464. 10.3340/jkns.2015.0910.003.
Prognostic Factor Analysis for Management of Chronic Neck Pain: Can We Predict the Severity of Neck Pain with Lateral Cervical Curvature?
- Affiliations
-
- 1Department of Neurological Surgery, Bumin Hospital Seoul, Seoul, Korea.
- 2Department of Neurology, Gangneung Asan Hospital, University of Ulsan College of Medicine, Gangneung, Korea.
- 3Department of Neurological Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 4Department of Neurological Surgery, Gangneung Asan Hospital, University of Ulsan College of Medicine, Gangneung, Korea. grandblue@gnah.co.kr
- KMID: 2387884
- DOI: http://doi.org/10.3340/jkns.2015.0910.003
Abstract
OBJECTIVE
Although little is known about its origins, neck pain may be related to several associated anatomical pathologies. We aimed to characterize the incidence and features of chronic neck pain and analyze the relationship between neck pain severity and its affecting factors.
METHODS
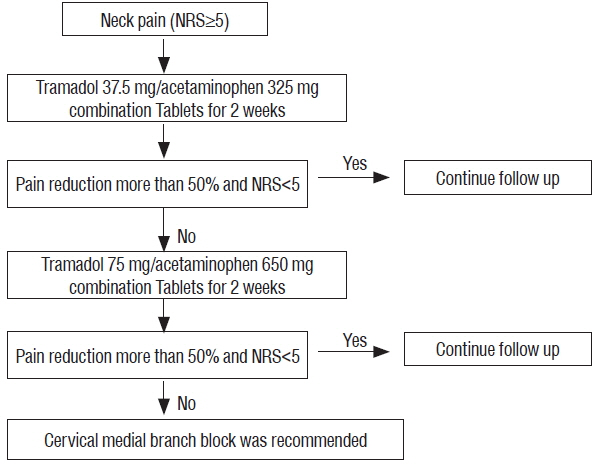
Between March 2012 and July 2013, we studied 216 patients with chronic neck pain. Initially, combined tramadol (37.5 mg) plus acetaminophen (325 mg) was administered orally twice daily (b.i.d.) to all patients over a 2-week period. After two weeks, patients were evaluated for neck pain during an outpatient clinic visit. If the numeric rating scale of the patient had not decreased to 5 or lower, a cervical medial branch block (MBB) was recommended after double-dosed previous medication trial. We classified all patients into two groups (mild vs. severe neck pain group), based on medication efficacy. Logistic regression tests were used to evaluate the factors associated with neck pain severity.
RESULTS
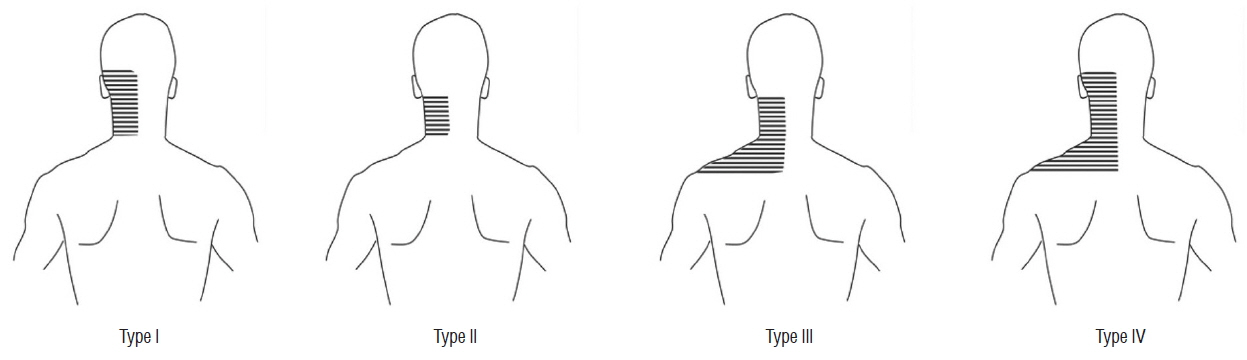
A total of 198 patients were included in the analyses, due to follow-up loss in 18 patients. While medication was successful in reducing pain in 68.2% patients with chronic neck pain, the remaining patients required cervical MBB. Lateral cervical curvature, such as a straight or sigmoid type curve, was found to be significantly associated with the severity of neck pain.
CONCLUSION
We managed chronic neck pain with a simple pharmacological management protocol followed by MBB. We should keep in mind that it may be difficult to manage the patient with straight or sigmoid lateral curvature only with oral medication.
MeSH Terms
Figure
Reference
-
References
1. Alperovitch-Najenson D, Sheffer D, Treger I, Finkels T, Kalichman L. Rehabilitation versus nursing home nurses’ low back and neck-shoulder complaints. Rehabil Nurs. 40:286–293. 2015.
Article2. American Society of Anesthesiologists Task Force on Chronic Pain Management, American Society of Regional Anesthesia and Pain Medicine. Practice guidelines for chronic pain management: an updated report by the American Society of Anesthesiologists Task Force on Chronic Pain Management and the American Society of Regional Anesthesia and Pain Medicine. Anesthesiology. 112:810–833. 2010.3. Barnsley L. Percutaneous radiofrequency neurotomy for chronic neck pain: outcomes in a series of consecutive patients. Pain Med. 6:282–286. 2005.
Article4. Benyamin RM, Datta S, Falco FJ. A perfect storm in interventional pain management: regulated, but unbalanced. Pain Physician. 13:109–116. 2010.5. Bogduk N. Practice guidelines: spinal diagnostic and treatment procedures. San Francisco: International Spine Intervention Society;2004.6. Borghouts JA, Koes BW, Bouter LM. The clinical course and prognostic factors of non-specific neck pain: a systematic review. Pain. 77:1–13. 1998.
Article7. Bot SD, van der Waal JM, Terwee CB, van der Windt DA, Scholten RJ, Bouter LM, et al. Predictors of outcome in neck and shoulder symptoms: a cohort study in general practice. Spine (Phila Pa 1976). 30:E459–E470. 2005.8. Brandt M, Sundstrup E, Jakobsen MD, Jay K, Colado JC, Wang Y, et al. Association between neck/shoulder pain and trapezius muscle tenderness in office workers. Pain Res Treat. 2014:352735. 2014.
Article9. Buckwalter JA. Aging and degeneration of the human intervertebral disc. Spine (Phila Pa 1976). 20:1307–1314. 1995.
Article10. Carroll LJ, Hogg-Johnson S, van der Velde G, Haldeman S, Holm LW, Carragee EJ, et al. Course and prognostic factors for neck pain in the general population: results of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders. Spine (Phila Pa 1976). 33(4 Suppl):S75–S82. 2008.11. Côté P, Cassidy JD, Carroll LJ, Kristman V. The annual incidence and course of neck pain in the general population: a population-based cohort study. Pain. 112:267–273. 2004.
Article12. Croft PR, Lewis M, Papageorgiou AC, Thomas E, Jayson MI, Macfarlane GJ, et al. Risk factors for neck pain: a longitudinal study in the general population. Pain. 93:317–325. 2001.
Article13. Dwyer A, Aprill C, Bogduk N. Cervical zygapophyseal joint pain patterns. I: a study in normal volunteers. Spine (Phila Pa 1976). 15:453–457. 1990.14. Enthoven P, Skargren E, Oberg B. Clinical course in patients seeking primary care for back or neck pain: a prospective 5-year follow-up of outcome and health care consumption with subgroup analysis. Spine (Phila Pa 1976). 29:2458–2465. 2004.
Article15. Falco FJ, Datta S, Manchikanti L, Sehgal N, Geffert S, Singh V, et al. An updated review of the diagnostic utility of cervical facet joint injections. Pain Physician. 15:E807–E838. 2012.16. Falco FJ, Erhart S, Wargo BW, Bryce DA, Atluri S, Datta S, et al. Systematic review of diagnostic utility and therapeutic effectiveness of cervical facet joint interventions. Pain Physician. 12:323–344. 2009.17. Falco FJ, Manchikanti L, Datta S, Wargo BW, Geffert S, Bryce DA, et al. Systematic review of the therapeutic effectiveness of cervical facet joint interventions: an update. Pain Physician. 15:E839–E868. 2012.18. Fejer R, Kyvik KO, Hartvigsen J. The prevalence of neck pain in the world population: a systematic critical review of the literature. Eur Spine J. 15:834–848. 2006.
Article19. Fukui S, Ohseto K, Shiotani M, Ohno K, Karasawa H, Naganuma Y, et al. Referred pain distribution of the cervical zygapophyseal joints and cervical dorsal rami. Pain. 68:79–83. 1996.
Article20. Ghafouri N, Ghafouri B, Fowler CJ, Larsson B, Turkina MV, Karlsson L, et al. Effects of two different specific neck exercise interventions on palmitoylethanolamide and stearoylethanolamide concentrations in the interstitium of the trapezius muscle in women with chronic neck shoulder pain. Pain Med. 15:1379–1389. 2014.
Article21. Gore DR, Sepic SB, Gardner GM. Roentgenographic findings of the cervical spine in asymptomatic people. Spine (Phila Pa 1976). 11:521–524. 1986.
Article22. Grob D, Frauenfelder H, Mannion AF. The association between cervical spine curvature and neck pain. Eur Spine J. 16:669–678. 2007.
Article23. Hartvigsen J, Frederiksen H, Christensen K. Back and neck pain in seniors-prevalence and impact. Eur Spine J. 15:802–806. 2006.
Article24. Hill J, Lewis M, Papageorgiou AC, Dziedzic K, Croft P. Predicting persistent neck pain: a 1-year follow-up of a population cohort. Spine (Phila Pa 1976). 29:1648–1654. 2004.25. Hoving JL, de Vet HC, Twisk JW, Devillé WL, van der Windt D, Koes BW, et al. Prognostic factors for neck pain in general practice. Pain. 110:639–645. 2004.
Article26. Kawakami M, Tamaki T, Yoshida M, Hayashi N, Ando M, Yamada H. Axial symptoms and cervical alignments after cervical anterior spinal fusion for patients with cervical myelopathy. J Spinal Disord. 12:50–56. 1999.
Article27. Laimi K, Pitkänen J, Metsähonkala L, Vahlberg T, Mikkelsson M, Erkintalo M, et al. Adolescent cervical disc degeneration in MRI does not predict adult headache or neck pain: a 5-year follow-up of adolescents with and without headache. Cephalalgia. 34:679–685. 2014.
Article28. Lord SM, Barnsley L, Wallis BJ, McDonald GJ, Bogduk N. Percutaneous radio-frequency neurotomy for chronic cervical zygapophyseal-joint pain. N Engl J Med. 335:1721–1726. 1996.
Article29. Malanga GA, Patel AD. The pharmacologic management of spine pain. Rao RD, Smuck M, editors. Orthopaedic knowledge update: spine. ed 4. Rosemont, IL: American Academy of Orthopaedic Surgeons;2012. p. 93–105.30. Manchikanti L, Boswell MV, Singh V, Benyamin RM, Fellows B, Abdi S, et al. Comprehensive evidence-based guidelines for interventional techniques in the management of chronic spinal pain. Pain Physician. 12:699–802. 2009.31. Manchikanti L, Manchikanti KN, Damron KS, Pampati V. Effectiveness of cervical medial branch blocks in chronic neck pain: a prospective outcome study. Pain Physician. 7:195–201. 2004.32. Manchikanti L, Singh V, Falco FJ, Cash KA, Fellows B. Comparative outcomes of a 2-year follow-up of cervical medial branch blocks in management of chronic neck pain: a randomized, double-blind controlled trial. Pain Physician. 13:437–450. 2010.33. Manchikanti L, Singh V, Helm S 2nd, Trescot AM, Hirsch JA. A critical appraisal of 2007 American College of Occupational and Environmental Medicine (ACOEM) Practice Guidelines for Interventional Pain Management: an independent review utilizing AGREE, AMA, IOM, and other criteria. Pain Physician. 11:291–310. 2008.34. Marchiori DM, Henderson CN. A cross-sectional study correlating cervical radiographic degenerative findings to pain and disability. Spine (Phila Pa 1976). 21:2747–2751. 1996.
Article35. Martin BI, Deyo RA, Mirza SK, Turner JA, Comstock BA, Hollingworth W, et al. Expenditures and health status among adults with back and neck problems. JAMA. 299:656–664. 2008.
Article36. Ofiram E, Garvey TA, Schwender JD, Denis F, Perra JH, Transfeldt EE, et al. Cervical degenerative index: a new quantitative radiographic scoring system for cervical spondylosis with interobserver and intraobserver reliability testing. J Orthop Traumatol. 10:21–26. 2009.
Article37. Park JH, Jeong EK, Lee MK, Chul Rhim S, Roh SW, Kim JH, et al. A unilateral open door laminoplasty technique: prospective analysis of the relationship between midline extensor muscle preservation and postoperative neck pain. J Clin Neurosci. 22:308–314. 2015.
Article38. Pernold G, Mortimer M, Wiktorin C, Tornqvist EW, Vingård E. Musculoskeletal Intervention Center-Norrtälje Study Group. Neck/shoulder disorders in a general population. Natural course and influence of physical exercise: a 5-year follow-up. Spine (Phila Pa 1976). 30:E363–E368. 2005.
Article39. Peterson C, Bolton J, Wood AR, Humphreys BK. A cross-sectional study correlating degeneration of the cervical spine with disability and pain in United kingdom patients. Spine (Phila Pa 1976). 28:129–133. 2003.
Article40. Rasmussen-Barr E, Grooten WJ, Hallqvist J, Holm LW, Skillgate E. Are job strain and sleep disturbances prognostic factors for neck/shoulder/arm pain? A cohort study of a general population of working age in Sweden. BMJ Open. 4:e005103. 2014.
Article41. Ruivo RM, Pezarat-Correia P, Carita AI. Cervical and shoulder postural assessment of adolescents between 15 and 17 years old and association with upper quadrant pain. Braz J Phys Ther. 18:364–371. 2014.
Article42. Yin W, Bogduk N. The nature of neck pain in a private pain clinic in the United States. Pain Med. 9:196–203. 2008.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Radiologic Finding of Patients with Neck Pain
- Differences of Spinal Curvature, Thoracic Mobility, and Respiratory Strength Between Chronic Neck Pain Patients and People Without Cervical Pain
- Review of Neck Pain, Kyphotic Change in the Cervical Spine and Exercise Treatment in Pilots
- Neck Pain
- The Change of Cervical Spine Curvature by Three Measurement Methods in Cervical Pain Patients