J Neurocrit Care.
2017 Jun;10(1):32-35. 10.18700/jnc.170005.
Phenylephrine Induced Posterior Reversible Encephalopathy Syndrome during Resection of Solitary Pulmonary Nodule
- Affiliations
-
- 1Department of Neurology, Konyang University College of Medicine, Daejeon, Korea. nukedoc@hanmail.net
- KMID: 2385884
- DOI: http://doi.org/10.18700/jnc.170005
Abstract
- BACKGROUND
Posterior reversible encephalopathy syndrome (PRES) is a neurological complication caused by cerebral hyperperfusion.
CASE REPORT
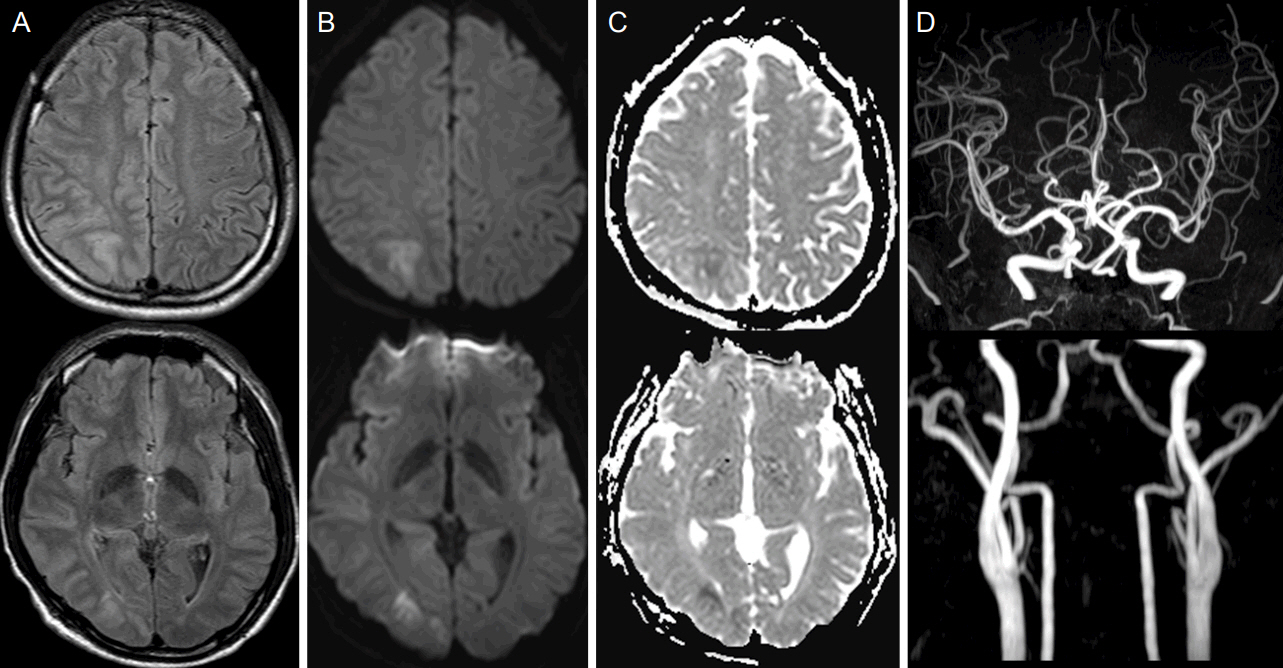
A 46-year-old male presented with decreased mental status, left facial palsy, and left-sided weakness after video-assisted thoracoscopic surgery for a solitary pulmonary nodule. During the surgery, phenylephrine was infused intravenously for general anesthesia-induced hypotension. High signal intensity at the right parietooccipital lobe was noted on fluid-attenuated inversion recovering imaging and diffusion-weighted imaging. His neurological symptoms improved two days after initial presentation. Follow-up diffusion-weighted imaging showed resolution of the brain lesions 10 days after the surgery.
CONCLUSIONS
We report a patient who presented with PRES after administration of phenylephrine during resection of a solitary pulmonary nodule. PRES should be considered for patients presented with acute neurologic symptoms following surgical procedures.
MeSH Terms
Figure
Reference
-
1. Fugate JE, Rabinstein AA. Posterior reversible encephalopathy syndrome: clinical and radiological manifestations, pathophysiology, and outstanding questions. Lancet Neurol. 2015; 14:914–25.
Article2. Fugate JE, Claassen DO, Cloft HJ, Kallmes DF, Kozak OS, Rabinstein AA. Posterior reversible encephalopathy syndrome: associated clinical and radiologic findings. Mayo Clin Proc. 2010; 85:427–32.
Article3. Rabinstein AA, Mandrekar J, Merrell R, Kozak OS, Durosaro O, Fugate JE. Blood pressure fluctuations in posterior reversible encephalopathy syndrome. J Stroke Cerebrovasc Dis. 2012; 21:254–8.
Article4. Gharabawy R, Pothula VR, Rubinshteyn V, Silverberg M, Gave AA. Epinephrine-induced posterior reversible encephalopathy syndrome: a case report. J Clin Anesth. 2011; 23:505–7.
Article5. Triquenot-Bagan A, Gerardin E, Guegan-Massardier E, Onnient Y, Leroy F, Mihout B. Postoperative reversible posterior leukoencephalopathy syndrome. Cerebrovasc Dis. 2003; 16:430–2.
Article6. Kastrup O, Schlamann M, Moenninghoff C, Forsting M, Goericke S. Posterior reversible encephalopathy syndrome: the spectrum of MR imaging patterns. Clin Neuroradiol. 2015; 25:161–71.
Article7. Allman KG, Wilson IH. Oxford Handbook of Anaesthesia. 3rd ed. New York: Oxford university press;2011. p. 367–8.8. Oderich GS, Pereira AA, Rabinstein AA, Mendes BC, Pulido JN. Posterior reversible encephalopathy syndrome from induced hypertension during endovascular thoracoabdominal aortic aneurysm repair. J Vasc Surg. 2015; 61:1062–5.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Posterior reversible encephalopathy syndrome and reversible cerebral vasoconstriction syndrome associated with acute exacerbation of chronic obstructive pulmonary disease
- Posterior Reversible Encephalopathy Syndrome in a Patient with Intoxication of Arisaema amurense
- Hypertension-induced Posterior Reversible Encephalopathy Syndrome
- Posterior Reversible Encephalopathy after Quetiapine Overdose
- Posterior Reversible Encephalopathy Syndrome after Massive Blood Transfusion in a Normotensive Patient