J Korean Soc Spine Surg.
2017 Jun;24(2):109-114. 10.4184/jkss.2017.24.2.109.
A Long, Solitary, Rosary-Shaped Spinal Neurofibroma
- Affiliations
-
- 1Department of Orthopaedic Surgery, Soonchunhyang University Seoul Hospital, Seoul, Korea. schsbj@schmc.ac.kr
- KMID: 2385647
- DOI: http://doi.org/10.4184/jkss.2017.24.2.109
Abstract
- STUDY DESIGN: Case report.
OBJECTIVES
We report the case of a long, solitary, rosary-shaped neurofibroma that was misdiagnosed as another disease due to the patient's surgical history involving repetitive procedures and its abnormal appearance. SUMMARY OF LITERATURE REVIEW: Neurofibroma is an intradural-extramedullary spinal tumor. It is generally not difficult to diagnose due to its frequent occurrence and specific magnetic resonance imaging (MRI) findings. However, to date, neurofibromatosis stigmata and long, solitary, rosary-shaped neurofibromas have rarely been reported.
MATERIALS AND METHODS
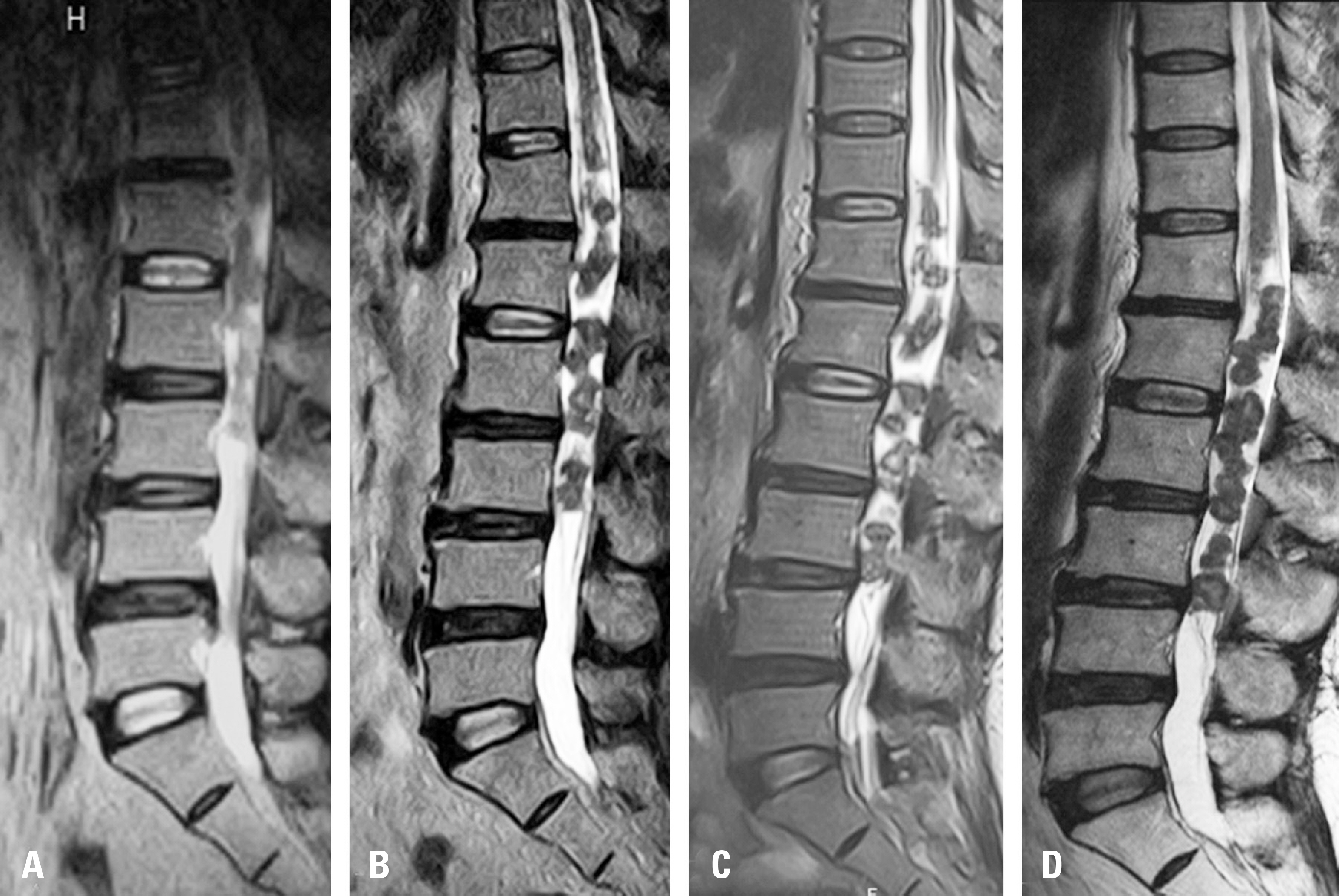
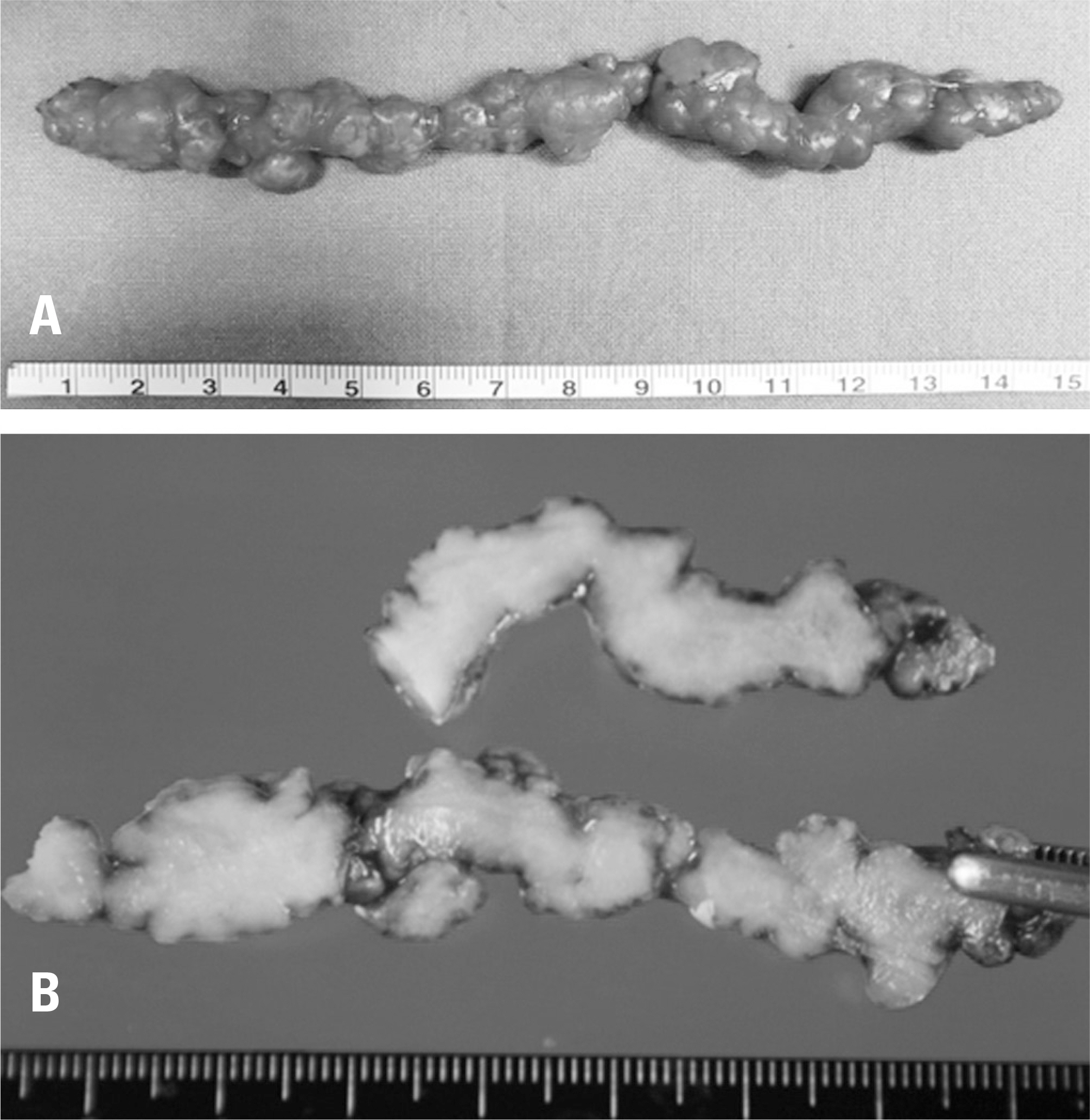
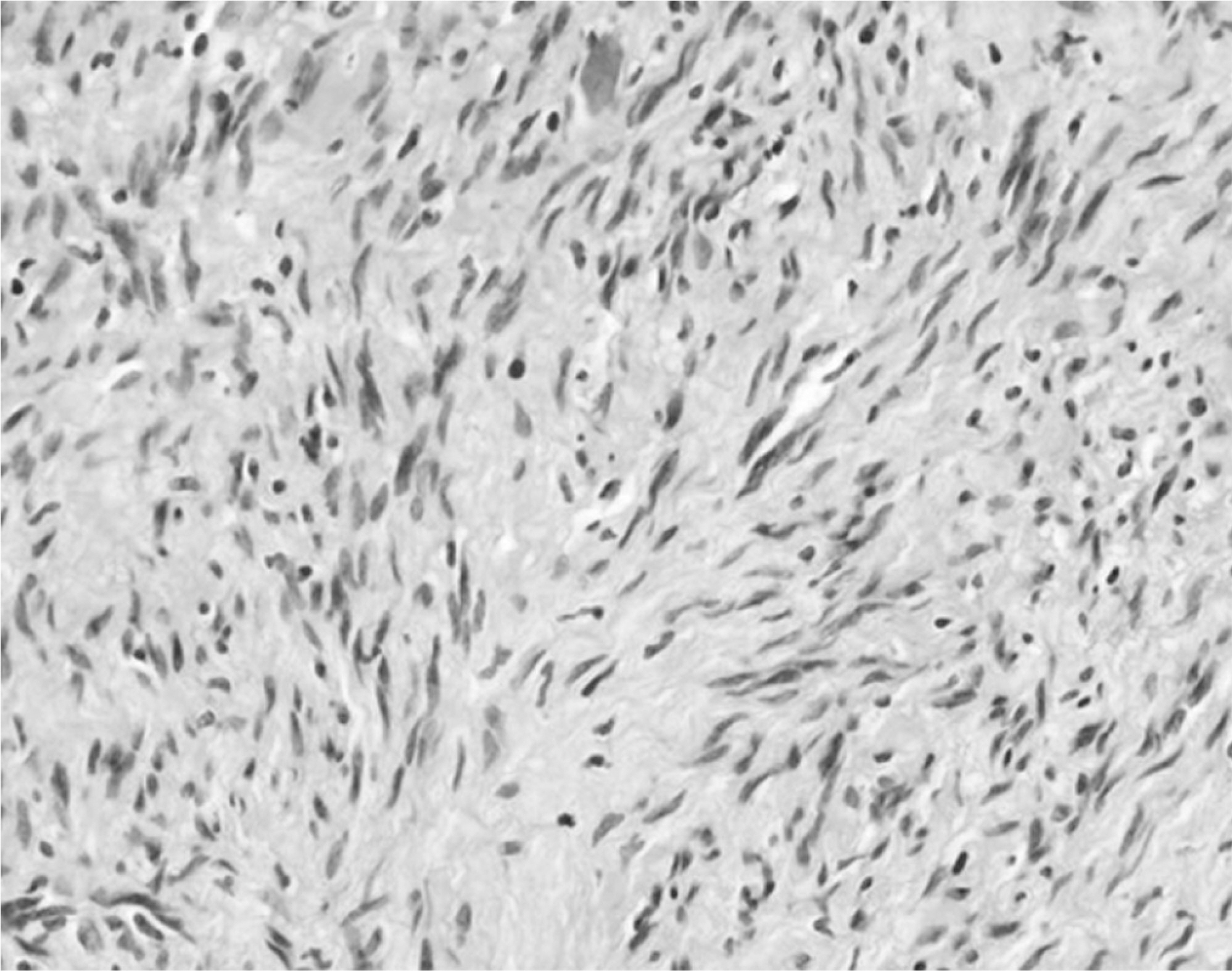
A 60-year-old woman was admitted to our hospital due to persistent pain, despite previous surgery and repetitive procedures. On physical examination, vision loss, hearing loss, skin discoloration, or subcutaneous nodules were not observed. A neurologic examination revealed normal motor and sensory function and voiding sensation. No pathologic reflexes such as the Babinski sign were observed. Previous sequential MRIs revealed intradural lesions that progressed from the thoracic vertebra 11 to the lumbar vertebra 3. She had no signs of neurofibromatosis stigmata, and the neurologic examination was unremarkable. The initial diagnosis was based on serial MRIs, which revealed a parasite infestation, a spinal cord tumor (myxopapillary-type ependymoma with hemorrhage), arachnoiditis, and vascular malformations. Total mass excision was performed, and the final diagnosis was neurofibroma.
RESULTS
There were no signs of a tumor remnants or local recurrence in a 1-year follow-up MRI study.
CONCLUSIONS
Although intradural spinal tumors are very rare, their clinical features are nonspecific and resemble other degenerative spinal diseases, including spinal stenosis and disc herniation. These diseases may easily be overlooked by physicians.
MeSH Terms
-
Arachnoid
Arachnoiditis
Christianity
Diagnosis
Diagnostic Errors
Ependymoma
Female
Follow-Up Studies
Hearing Loss
Humans
Magnetic Resonance Imaging
Middle Aged
Neurofibroma*
Neurofibromatoses
Neurologic Examination
Parasites
Physical Examination
Recurrence
Reflex
Reflex, Babinski
Sensation
Skin
Spinal Cord Neoplasms
Spinal Diseases
Spinal Stenosis
Spine
Vascular Malformations
Figure
Reference
-
1. Seppala MT, Haltia MJ, Sankila RJ, et al. Longterm outcome after removal of spinal neurofibroma. J Neurosurg. 1995; 82:572–7.2. Sanguinetti C, Specchia N, Gigante A, et al. Clinical and pathological aspects of solitary spinal neurofibroma. J Bone Joint Surg Br. 1993; 75:141–7.
Article3. Carra BJ, Sherman PM. Intradural Spinal Neoplasms: A Case Based Review. J Am Osteopath Coll Radiol. 2013; 2:13–21.4. Prasad K, Chandrashekar N. Long segment spinal neurofibroma: An unusual cause of low back pain. Indian Journal of Neurosurgery. 2013; 2:89.5. Park JH, Park YS, Kim JS, et al. Sparganosis in the lumbar spine: report of two cases and review of the literature. J Korean Neurosurg Soc. 2011; 49:241–4.6. Kwon JH, Kim JS. Sparganosis presenting as a conus medullaris lesion: case report and literature review of the spinal sparganosis. Arch Neurol. 2004; 61:1126–8.
Article7. Cho YD, Huh JD, Hwang YS, et al. Sparganosis in the spinal canal with partial block: an uncommon infection. Neuroradiology. 1992; 34:241–4.
Article8. Fassett DR, Schmidt MH. Lumbosacral ependymomas: a review of the management of intradural and extradural tumors. Neurosurg Focus. 2003; 15:E13.
Article9. Wright MH, Denney LC. A comprehensive review of spinal arachnoiditis. Orthop Nurs. 2003; 22:215–9.
Article10. Cho WS, Kim KJ, Kwon OK, et al. Clinical features and treatment outcomes of the spinal arteriovenous fistu-las and malformation: clinical article. J Neurosurg Spine. 2013; 19:207–16.